Soft Palate Reconstruction Using Bilateral Palatal Mucomuscular Flap and Pharyngeal Flap after Resection of Squamous Cell Carcinoma
Article information
Abstract
Squamous cell carcinoma infrequently occurs at the soft palate. Although various methods can be used for reconstruction of soft palate defects that occur after resecting squamous cell carcinoma, it is difficult to obtain satisfactory results from the perspective of the functional restoration of the soft palate. A combination of bilateral palatal mucomuscular flap for the oral side and superiorly based posterior pharyngeal flap for the nasal side were performed on two patients who were diagnosed with squamous cell carcinoma of the soft palate in order to reconstruct the soft palate defects after surgical resection. After surgery, the patients were followed-up for a mean period of 11 months. The flaps were well maintained in both patients. The donor site defects were epithelialized and completely recovered. Additionally, no recurrence of the primary sites was shown. Slight hyponasality was observed in the voice assessments that were conducted 6 months after surgery. No food regurgitation or aspiration was observed in the swallowing tests. We used a combination of bilateral palatal mucomuscular flap and superiorly based posterior pharyngeal flap to reconstruct the soft palate defects that occurred after resecting the squamous cell carcinomas. We reduced the donor site complications and achieved functionally satisfactory outcomes.
INTRODUCTION
It is known that oropharyngeal cancer accounts for approximately 12% of all head and neck cancers, and that squamous cell carcinoma accounts for more than 90% of cancers that occur in the oropharynx. Squamous cell carcinoma (SCC) occurs most frequently at the peritonsillar area, followed by the tongue base, soft palate, and oropharyngeal wall in that order [1]. SCC rarely occurs at the soft palate and uvula, but in most cases of soft palate cancer, if it is diagnosed early, it can be cured using surgical resection and radiotherapy [2,3]. In the case of a surgical treatment of a lesion that invades the muscle of the soft palate, metastasis may increase and serious functional sequelae may occur after resection. Thus, radiotherapy is the preferred treatment [1]. However, considering the possible long-term side defects caused by radiation therapy and good reconstructive options with a positive functional outcome, surgery might be preferred. In principle, a combined treatment of surgical resection and postoperative radiotherapy is another treatment option for soft palate cancer in the advanced stage [2].
To overcome language impairment and dysphagia that occurs after surgical resection of a soft palate, which has various functions, surgical reconstruction with various prostheses has been conducted. Reconstruction with a prosthesis is relatively easy, but results in decreased functional recovery and patient compliance [1]. For surgical reconstruction, various reconstruction methods are used such as uvulopalatal flap [4], buccal mucosal flap [5], and radial forearm free flap [6], but they all result in donor site complications and unsatisfactory functional outcomes.
In this study, we used a combination of bilateral palatal mucomuscular flap and superiorly based posterior pharyngeal flap to reconstruct the soft palate defects that occurred after curative resection in two patients with SCC of the soft palate. Satisfactory outcomes were obtained. Thus, the authors report the surgical method and the results of the clinical follow-up here.
CASE
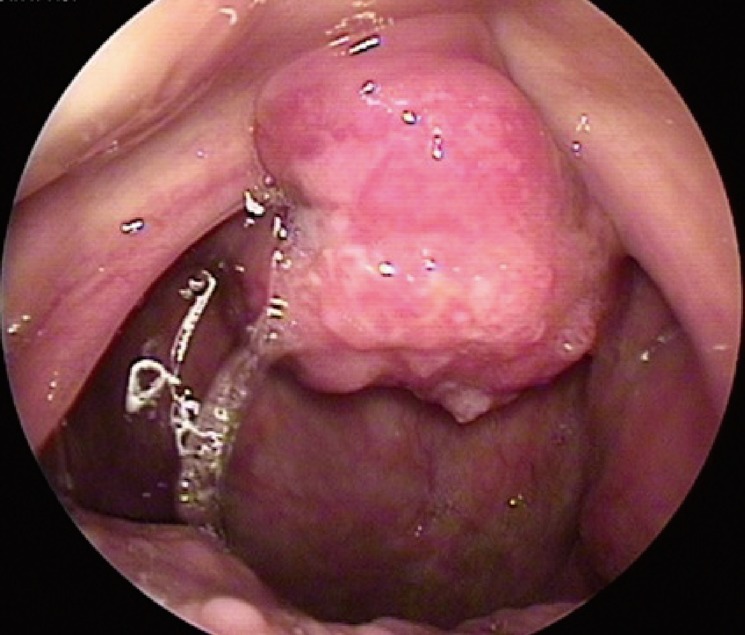
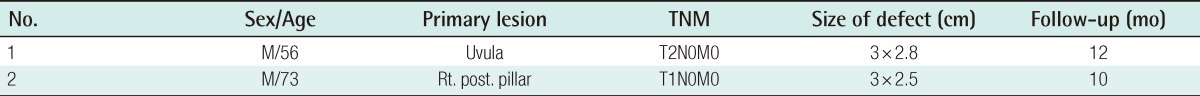
This study was conducted from April to June 2011 on two patients with a soft palate defect. Both patients were diagnosed with moderate SCC of the soft palate, and they had a tumor-node-metastasis (TNM) stage of T2N0M0 and T1N0M0, respectively (Fig. 1). No primary metastasis was found. A follow-up study was conduced for a period of 10 to 12 months (Table 1).
Surgical technique
After extensive resection of the soft palate carcinoma (Fig. 2), the incision line was designed for bilateral palatal mucomuscular flap at the boundary between the hard and soft palate in the remaining soft palatal area of the oral cavity. At the same time, the incision line was designed for superiorly based posterior pharyngeal flap for the nasal cavity (Fig. 3).
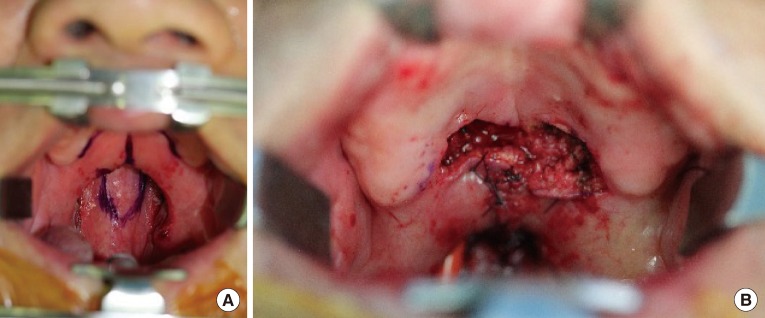
Flap design and after flap performed state (case 1)
(A) Preoperative flap design, (B) Immediate postoperative gross photo.
The midline was incised at the soft palatal area, and then bilaterally tracked using #2 black silk sutures, followed by elevating the pharyngeal flap from the posterior wall of the pharynx. An 8 French catheter was then inserted via the nostrils to determine the lateral port size. After elevating the flap, the posterior wall of the pharynx was primarily sutured using vicryl 4-0 sutures after arresting bleeding. Next, the resection line of the boundary between the soft and hard palate was incised, and the palatal mucomuscular flap was bilaterally elevated. It was then rotated toward the pharyngeal flap, followed by suturing of the pharyngeal flap using vicryl 4-0 sutures at the oral and nasal cavities (Fig. 4). After the operation, the catheter was immediately removed because it could not be used as a nasal airway.
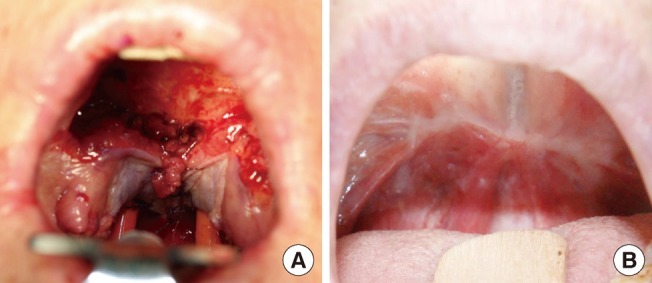
Postoperative appearance of case 2 patient
(A) Immediately postoperative gross photo, and (B) a gross photo 6 months after surgery.
The function of the lateral port was assessed using flexible nasopharyngoscopy, performed at least 6 months after surgery, and a speech and language therapist assessed the patients' speech. Food reflux or aspiration into the nasopharynx during swallowing was assessed using swallowing videofluoroscopy (Table 2).
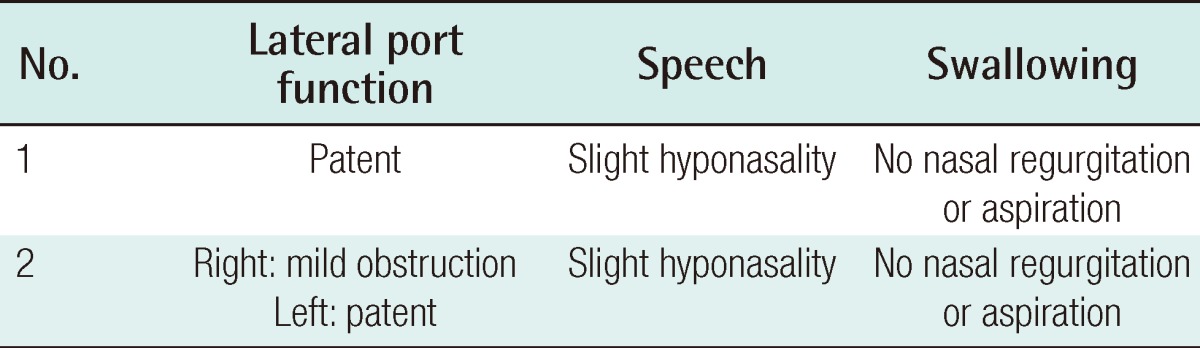
Summary of the postoperative functional assessment results of the lateral port function, speech, and swallowing
No recurrence of the primary site was found in either of the patients after surgery. The flap was well maintained without cleft, and the donor site was epithelialized and recovered 4 weeks after surgery (Figs. 5, 6). Nasal obstruction was found in one patient 6 months after the operation. Because lateral port obstruction was found during a subsequent examination, a revision was conducted on the patient. No other complications were found.
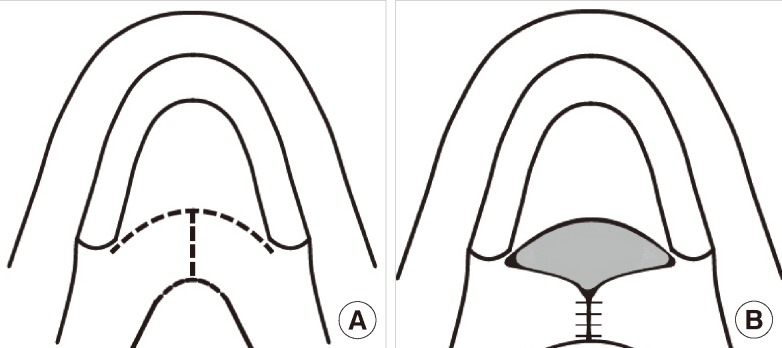
Schema of the bilateral palatal mucomuscular flap
(A) The outline of the incision, and (B) completed operation.
DISCUSSION
Oral cancer accounts for approximately 5% of the total carcinomas that occur in the body. SCC accounts for the majority of the cases of oral mucous membrane cancer. SCC that occurs at the oral cavity frequently occurs at the tongue and lower lip, whereas SCC that occurs at the soft palate and uvula is very rare [3]. Smoking, drinking, and human papillomavirus infection are known to be risk factors.
SCC of the soft palate has clinical symptoms such as dysphagia, pain, awareness of a neck mass, and intraoral bleeding. It can be easily found because it is mainly positioned at the anterior part of the oropharynx. A histologic examination can be conducted in the clinic.
In cases of early soft palate cancer, it can be cured using surgical treatment and radiotherapy. At the same time, in advanced cases, surgical resection, supportive radiotherapy, and additional chemotherapy can be applied.
The soft palatal area is a dynamic muscular structure, which effectively separates the pathway of the oral and nasal cavities. Soft palate defects that occur after resection may cause hypernasal speech and food reflux into the nose upon swallowing. Thus, functional mucomuscular soft palate structure and oronasal obstruction are the goals of reconstruction of the palate [2].
Prostheses and surgical reconstruction are used for the functional reconstruction of the soft palate. Although reconstruction with a prosthesis is relatively easy to perform, it decreases function and patient compliance, and the procedure is difficult to perform in patients with a large defect or without teeth [1].
Among the surgical reconstructions available, superior constrictor advancement-rotation flap reconstructs the valvular sphincteric function by incising the opposite tonsillar pillar and rotating the velopharyngeal area for the circumferential closure. The procedure can be used in 35% to 65% of soft palate defect cases, but it is restricted for large defects of the soft palate, tonsil, and marginal pharyngeal wall [7].
Radial forearm free flap is most frequently used among soft palate reconstructions using free flap. It can be applied without the limitation of defect size, but has disadvantages of requiring a longer operation time, the addition of skin transplantation to the donor site, and sacrificing the radial artery [8].
Gangloff et al. [9] reported that hypo-hyoid myocutaneous flap was performed in order to reconstruct small or intermediate soft palate defects, and that its use was limited if patients had previously undergone thyroid surgery or radical neck dissection.
Pharyngeal flap is commonly used for velopharyngeal insufficiency. Satisfactory speech and swallowing results can be obtained after surgery. Superiorly based posterior pharyngeal flap can be designed as a pharyngeal flap with a sufficient length and can be used in all age groups [10]. However, it may be difficult to apply a pharyngeal flap if the lateral wall movement of the pharynx is weak. Pharyngeal flap was applied in this study because the lateral wall movement of the pharynx was normal in the two patients. The defect of the oral cavity was reconstructed by posteriorly extending the soft palatal area that remained after resection using mucomuscular flap, and the defect of the nasal cavity was reconstructed using superiorly based pharyngeal flap. The adjacent tissue using the remaining soft palatal area and posterior wall of the pharynx was used in this study, and this method had the advantages of decreased impairment of the donor site, only requiring a single operation, and short hospitalization. Furthermore, a satisfactory result was obtained for swallowing. Therefore, this method is a good reconstructive option for soft palate defects of small to moderate size.
A limitation of this method is that it is difficult to perform in a large soft palate defect. Thus, in the cases of large soft palate defects or defects requiring resection of other areas, a free flap or the additional use of other flaps would be required.
In this study, slight hyponasality during speech was shown in the two patients. This is likely to have occurred due to the narrow lateral port size caused by postoperative constricture. If the lateral port size is adjusted considering the occurrence of constricture upon surgery, hyponasality could be improved. In addition, nasal obstruction occurred in one patient due to a lateral port obstruction, and the patient underwent a revision operation of the lateral port. No other complications were found.
In conclusion, we used a combination of bilateral palatal mucomuscular flap for the oral side and nasal superiorly based posterior pharyngeal flap for the nasal side to reconstruct the soft palate defect that occurred after resecting SCC of the soft palate. The results showed decreased complications of the donor site and good functional outcomes. Thus, the surgical method has been reported here with a review of the related literature.
Notes
This article was presented at the 2nd Research and Reconstructive Forum on June 1-2, 2012 in Gwangju, Korea.
No potential conflict of interest relevant to this article was reported.