Fabrication of Stable Cartilage Framework for Microtia in Incomplete Synchondrosis
Article information
Abstract
The synchondrosis between the sixth and seventh costal cartilage is usually used for the base frame in autogenous ear reconstruction. If the synchondrosis is loose, a variety of modifications can be devised. This report introduces new methods for these problems. In cases of incomplete synchondrosis, only the surface of the base block margin was smoothly tapered without carving for the removal of the conchal deepening. The secure fixation of the two segments (helix and antihelix) to the base block using fine wire sutures gave stability to the unstable basal frame. After confirming that all the segments were assembled in one stable piece, the remaining conchal deepening of the basal framework was removed, and the outer lower portion of the basal cartilage was trimmed along its whole length. A total of 10 consecutive patients with microtia, ranging from 8 to 13 years old, were treated from 2008 to 2009. The follow-up period was 6 months to 2 years. Despite incomplete synchondrosis, the stable frameworks were constructed using the authors' method and aesthetically acceptable results were achieved. The proposed method can provide an easy way to make a stable cartilage framework regardless of the variable conditions of synchondrosis.
INTRODUCTION
In order to reconstruct the ear, numerous materials have been used; however, autologous costal cartilage is the most commonly used and preferred material for ear reconstruction by Tanzer and many other surgeons such as Brent, Nagata, Park, and Firmin [1]. Although the cartilage framework construction method varies from surgeon to surgeon, the base frame is constructed from the sixth and seventh rib cartilage. Segments for the helical rim from the eighth cartilageand antitragus with superior and inferior crus are added. Sometimes, this framework needs to overcome technical challenges due to variable anatomical properties including the width, thickness, length of the available cartilages, and the synchondrosis between cartilages. The synchondrosis between the sixth and seventh costal cartilage is the most important factor in constructing the base frame. If the synchondrosis is loose or small, there are a variety of devised modifications that can be used such as wiring, suture, attaching additional cartilage, or assembling several pieces of cartilage [2-5]. In addition, most surgeons have removed the conchal deepening on the basal framework before the helix and antihelix constructions. This often leads to a lack of stability in the small, completed basal framework, and this instability makes it difficult to construct the helix and antihelix. Therefore, the current authors introduce a new technique for the fabrication of a stable cartilage framework that solves these problems in cases of incomplete synchondrosis through the modification of previous techniques.
IDEA
In the first stage, a pattern for the construct was made by placing a piece of X-ray film against the normal ear with moderate pressure and tracing its anatomic landmarks as a one-dimensional architecture of the ear. The template was then reversed and made several millimeters smaller throughout to accommodate the thickness of the skin cover. Once configured, the template was aligned symmetrically with the contralateral ear using the ear's relationship to the nose, the lateral canthus, and the position of the lobule.
The ipsilateral sixth, seventh, and eighth costal cartilages were harvested because the perichondrium of the outer surface would become the inner surface and might be helpful to prevent late absorption. Although the construct base was usually formed by the synchondrosis of the sixth and seventh cartilages, in cases of incomplete synchondrosis, only the surface of the base block margin was smoothly tapered without carving for the removal of the conchal deepening. The floating eighth-rib cartilage was used to fabricate the helical element. A lateral segment of the seventh cartilage 4 to 5 cm in length was used to fabricate the antihelix including the superior and inferior crus.
The cartilage pieces were fixed in place with 5/0 clear nylon suture or wire. When the carved helix was fixed to the basal cartilage, the helix was anchored with a slight outward inclination of 10-15 at the middle one-third of the ear [1]. The secure fixation of the two segments (helix and antihelix) to the base block with several fine wire sutures gave stability to the unstable basal frame. After confirming that all the segments were assembled as a stable one-piece structure, the remaining conchal deepening of the basal framework was removed, and the outer lower portion of the basal cartilage was trimmed along its whole length by using the X-ray template as a reference (Figs. 1, 2). The scaphoid fossa was carved with smooth deepening. The surface was smoothly tapered to avoid block-like corners so that the covering skin would fit smoothly onto the framework. Cartilage wedges were removed to form the helical sulcus and triangular fossa. The remnant cartilaginous fragments after carving were banked into the subcutaneous pocket of the donor site for elevation of the auricle in the second stage.
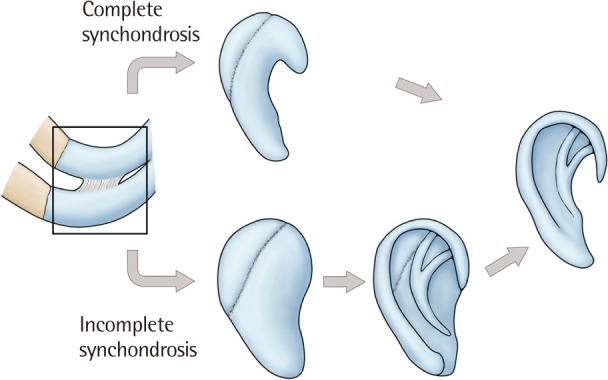
Schematic diagram of the author's technique
The constructed base was formed by the synchondrosis of the sixth and seventh cartilages. In cases of incomplete synchondrosis, the secure fixation of the two segments (helix and antihelix) to the base block with several fine wire sutures gave stability to the unstable basal frame. After confirming that all the segments were assembled as a stable one-piece structure, the remaining conchal deepening of the basal framework was removed.

Completion of the cartilage framework carving
The cartilage framework was completed by carving for the removal of the conchal deepening.
The cartilage framework constructed as such was placed into a subcutaneous pocket through an incision located at the posterior inferior border of the vestige. The tail of the framework was set into the lobule, and the outer incision was sutured. Two small polyethylene drains with multiple perforators near the end were inserted beneath and adjacent to the framework for occlusion of the overlying skin flap to the construct, and thus, the defining relief of the ear form was achieved. Two or three drains were fixed to the skin with 5/0 nylon sutures. A 50-mL disposable syringe consisting of a piston and a cylinder was connected to the polyethylene drain [1].
After the last stitch of the subcutaneous pocket incision was made, the drain was run, the flap was placed onto the frame, and adhesion was achieved. After achieving the proper tension, the piston was fixed with two wooden tongue depressors. All folds of the ear were filled with petrolatum gauze in all patients (Fig. 3). The disposable 50-mL syringe was frequently changed in the ward, and the proper tension was maintained. The drains were removed on the fourth or fifth postoperative day when the drainage volume was less than 1-mL [1]. The ear convolution was packed with petrolatum gauze for the first postoperative week. All sutures were removed on the seventh postoperative day. The second stage operation was performed 5 to 6 months after the first operation (Figs. 4, 5).

Insertion of the cartilage framework
The cartilage framework constructed as such was placed into a subcutaneous pocket through an incision located at the posterior inferior border of the vestige. After the last stitch of the skin was made, the drain was run, the flap was placed onto the frame, and adhesion was achieved. All folds of the ear were filled with petrolatum gauze in all patients.
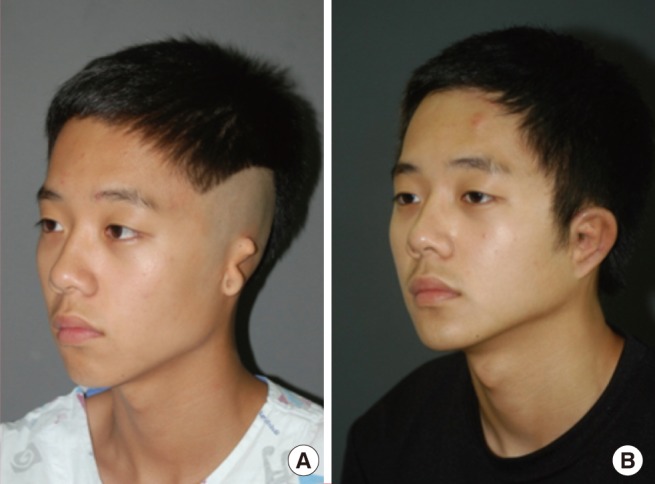
An 11-year-old patient with microtia on the left side
(A) Preoperative view. (B) Two-year postoperative view.
DISCUSSION
There are several methods for cartilage framework fabrication in autologous ear reconstruction. Brent [3] used a sculpting technique to make a cartilage block into a basal framework that had the basic shape of the ear containing the antihelix and conchal deepening. Nagata [5] made three dimensional structures of the ear by the addition of the antihelix using the ninth costal cartilage and the helix using the eighth costal cartilage as a two layer structure on the carved basal framework. The current authors proposed that in the upper one-third of the auricle, the helix and the scaphoid fossa presented a more characteristic contour than the antihelix [1]. However, in the middle one-third of the auricle, the length of the antihelix was similar to that of the helix. The antitragus portion of the antihelix was high and was trimmed lower toward the superior crus and the inferior crus. Before adding the helix and the antihelix, conchal deepening for the fabrication of the basal framework sometimes provided an unstable basal framework especially in case of a loose union between the sixth and seventh costal cartilages. The current author added the helix using the eighth costal cartilage and the antihelix using the part of the sixth costal cartilage on the basal framework before conchal deepening, which provided a more stable framework.
In this article, the current authors focused on the union between the sixth and seventh costal cartilages among the variable anatomical conditions of the rib cartilage. Since favorable cartilage framework construction starts from making a secure basal cartilage frame, this union, the so called synchondrosis, plays a key role in forming the basal frame as a supportive framework. According to the conditions of this site, some technical manipulations were often required for a secure basal frame. In fact, the union between the sixth and seventh costal cartilages was not a synchondrosis anatomically. It was an articulation between the adjacent borders of the sixth and seventh costal cartilages and the plane of the synovial joint. This joint usually has a synovial cavity that is enclosed by an articular capsule and strengthened by interchondral ligaments. The "interchondral joint" is more correct nomenclature than "synchondrosis," and mobility of this union is its native feature [6-8]. Furthermore, this union usually remains as a synovial joint in older age, despite the calcification process which is related to aging in the costal cartilages [8]. Therefore, the sixth and seventh costal cartilages rarely form a solid block because of the native looseness of this joint, and the looseness differs among individuals. In order to overcome such looseness, reinforcement of the sutures using nylon or wire was usually done before fabrication of the basal framework. However, lack of stability often remained in the small, completed basal framework because of an inadequate reinforcing suture or the extent of manipulation required for steps such as making the conchal deepening, and this status made it difficult to construct the helical rim and anthelix. Chin et al. [2] attached an additional thin sheet of Y-shaped antihelical complex to cover the notch on the basal cartilage framework in cases of loose synchondrosis between the sixth and the seventh cartilages to prevent a staircase appearance. Moreover, several surgical procedures for making a solid basal frame from the mobile cartilage block can lead to unintended damage to the cartilages.
To minimize procedures and prevent possible damage caused by difficult procedures, the current authors suggest a simple and easy method available for all cases of loose interchondral joints between the sixth and seventh rib cartilages. After harvesting, the surface of the base block margin was smoothly tapered only without carving especially for the removal of the conchal deepening. Two segments, the helix and antihelix, were fixed to the base block. Stability of the catilage framework was achieved by the secure attachment of two structures (helix and antihelix) to the base block. These procedures converted each segment into a solid one-piece material because the helix and the antihelix have an effect on the mobile base frame like a splint, and then the surgeons can complete the cartilage framework fabrication just by sculpting using the X-ray template as a reference.
There are several advantages in this proposed technique. First, its simplicity reduces the surgeon's efforts and time for making a stable basal framework. Second, it does not alter the normal anatomical structure of the cartilage block from the sixth and seventh rib cartilage with the interchondral joint. Any procedure which leads to damages on the cartilage framework can disturb the nourishment of the graft's survival. In the same manner, the current authors suggest that maintenance of the normal anatomical structure of the base cartilage block may secure the survival of the cartilage graft as well. Additional attempts at changing the interchondral joints may inevitably lead to anatomical deterioration and chondrocyte damage. Finally, the authors' method can produce consistent results despite the variable condition of the interchondral joints because the secure attachment of the helix and antihelix segments gives stability to the mobile base block and sculpting of the cartilage framework, especially for the basal frame, becomes easier.
Notes
No potential conflict of interest relevant to this article was reported.
This article was presented at the 68th Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 4-7, 2010 in Seoul, Korea.
