Treatment of Refractory Lower Extremity Ulcer Associated with Sneddon's Syndrome
Article information
A patient with livedo reticularis and ischemic cerebrovascular disease was first reported by Sneddon in 1965, after which the disease was named Sneddon's syndrome [1], a very rare disease with the incidence of four new cases per million per year [2].
A 49-year-old male patient was referred from the dermatologic clinic to our department for painful long lasting ulcers in the right lower leg and left heel. The larger one was about 9×5 cm in size on the right shin and the other was about 4×4 cm on the left heel. However, there was no exposure of bony or tendinous structures; the ulcer was covered with unhealthy granulation tissues. The patient's medical history included hypertension and diabetes mellitus, which were well controlled with medication. About 2 months before, he had experienced the first cerebral stroke episode of a transient ischemic attack, and he had been hospitalized for a while. During the period, small painful ulcers developed on both lower extremities, and a dermatologist had regularly followed up with him and had treated the ulcers for 2 months. Histological examination of the ulcer-biopsy specimen revealed a kind of vasculitis (Fig. 1). However, the major arteries of the lower extremity were intact without any stenotic lesions on angiography. The lesions had been aggravated since then, and the patient was referred to our department for surgical management.
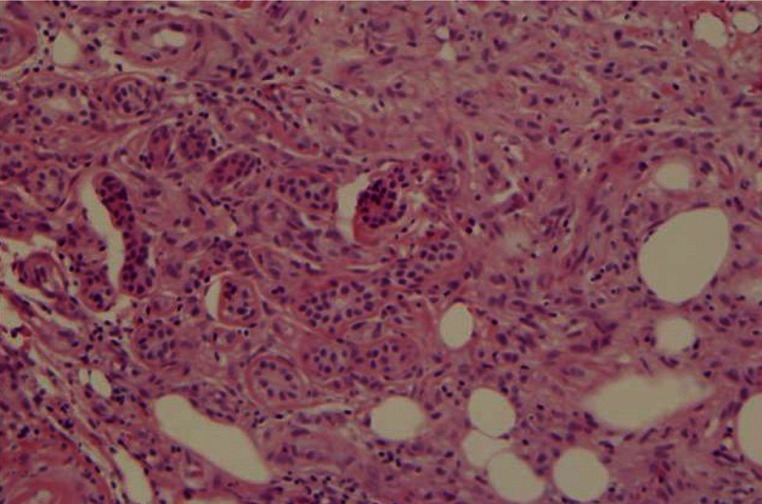
Hisological findings of the ulcers. A 3-mm punch biopsy showed endothelial inflammation, subendothelial myointimal hyperplasia, and partial occlusion (H&E, ×200).
After a second debridement in our department, the ulcers grossly showed relatively healthy granulation tissue without evidence of infection (Fig. 2), so he was scheduled to undergo debridement and skin grafting. During the preoperative period, motor weakness in his left upper and lower extremities suddenly developed again. He had already been taking low-dose aspirin and an antihypertensive drug since his first episode of the transient ischemic attack. The scheduled operation was postponed temporarily due to his perioperative risk based on the recurrent and recent cerebrovascular accidents. He was immediately seen by a neurologist for the management of the recurrent attacks. Multiple subcortical infarct lesions were identified on MRI (Fig. 3). The neurologist diagnosed him with Sneddon's syndrome, a rare disease, from his clinical course including the skin lesions. An additional anticoagulation treatment with heparin and warfarin was started and maintained for the treatment of the disease. The skin ulcers were treated daily with aseptic dressing. The neurologist administered intravenous immunoglobulin (IVIG) at 0.5 g/kg per day for 5 days in order to attenuate the course of disease, including preventing further aggravation of the skin lesions. The neurologic symptoms were slowly relieved. The wound was not healed but generally stabilized. After 1 month of treatment, the patient was readmitted to our department for a skin graft operation. The granulation tissue had grown, but a small shallow ulcer had newly formed caudally to the previous lesion on the right shin. Debridement of the unhealthy granulation tissue and split thickness skin grafting were performed. The graft had taken by the postoperative fifth day, particularly on the longer lasting lesion of grossly observed granulation tissue, but the graft was almost lost afterward in the newly developed caudal lesion. During the subsequent follow-up period, the newly developed lesion healed spontaneously with aseptic dressing changes. The wound healed completely on the right pretiabial area as shown in Fig. 4. All of the grafts remained stable until the most recent visit for evaluation.

The ulcers with livedo reticularis. This photograph shows the wound on the right pretibial area. After the second debridement, this ulcer grossly showed relatively healthy granulation tissue without any sign of infection.
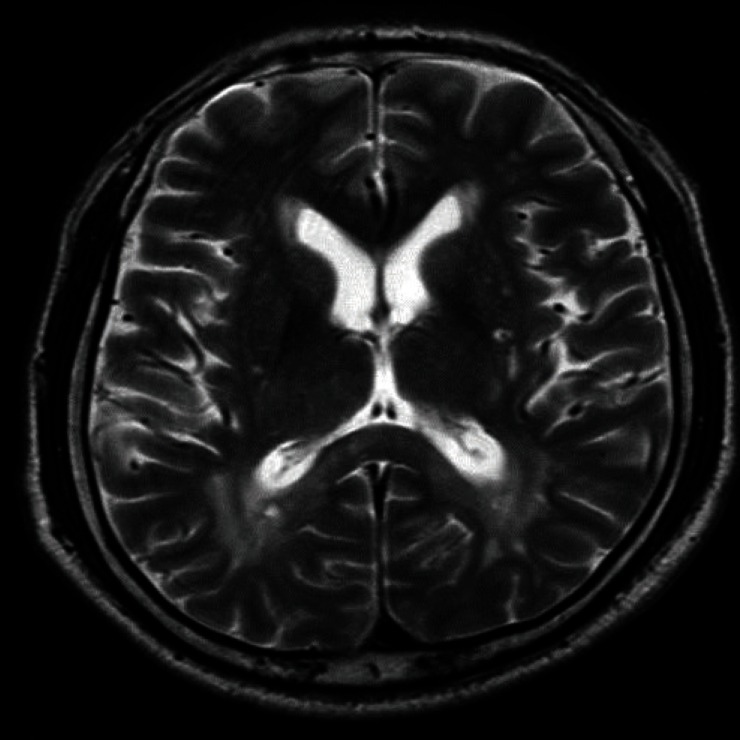
T2-weighted axial image showed multiple focal high signal intensity areas in both coronal radiata, the left internal capsule of the posterior limb, the paraventricular white matter, and the left parietooccipital white matter. It was compatible with acute infarction.

Photograph of the lesion 5 months after the operation. Healing had completed in the right pretibial area.
The etiology of Sneddon's syndrome remains to be elucidated; possible causes have been thought to be related to autoimmunity, a thrombophilic tendency, or inflammatory vascular processes. Some assert that this disease is a progressive non-inflammatory thrombotic vasculopathy affecting small and medium-sized arteries in the brain and skin [3]. This presumption suggests a possible biological link between vasculopathy and primary coagulopathy that many Sneddon's syndrome patients manifest. The biopsy reports revealed that skin lesions in patients with this syndrome often show vasculitic components, although not in every case.
Another symptom that Sneddon's syndrome patients manifest is livedo reticularis, which is caused by thrombosis of the subcutaneous arterioles leading to a compensatory reaction activated via capillary dilation. The mottled appearance of such skin lesions is due to blood stagnation. The pattern of livedo reticularis varies according to the presence of antiphospholipid antibodies. The pattern of mottling is said to be finer in seropositive patients than seronegative patients [3].
Treatment of Sneddon's syndrome is often unsatisfactory and no standard therapy is available. Treatment for Sneddon's syndrome is mainly based on rheological and immunosuppressive agents. The only treatment plan that has been proven to be effective is warfarin anticoagulation [4]. Warfarin can be effective for asymptomatic cardiac valvulopathy and the cerebral microemboli that are frequently associated with Sneddon's syndrome. Livedo reticularis and acrocyanosis can be reduced by nifedipine but cannot prevent cerebrovascular complications. Various antiplatelet and immunomodulatory agents including steroids and aszathioprine sodium seem to have little effect on Sneddon's syndrome.
Ulcerated skin lesions in the lower extremities are also representative manifestations in Sneddon's syndrome. These lesions usually heal spontaneously with non-surgical dressing changes, as supported by some previous reports, but most articles have not clearly commented on the clinical assessment and treatment of skin ulcer lesions.
The skin lesion in the present patient was caused by ischemic vasculitis which deteriorating oxygen perfusion through the tissue in the area, which would be incompatible with a skin graft. However, skin grafting could be an effective reconstructive method for diabetic ulcers or other chronic wounds from vascular insufficiency if they have been prepared with adequate preoperative management. These large ischemic ulcers are also challenging to reconstructive surgeons. The clinical progression of Sneddon's syndrome involves a waxing and waning condition as in other chronic diseases. In our case, the period of wound care was quite long and the ulcer bed seemed to be prepared for skin grafting; that is to say, the wound had healthy red granulation tissue and signs of epithelial migration. In addition, the event of recurred stroke before the operation allowed us to make an accurate diagnosis with the help of a neurologist. A review of the literature revealed that Sneddon's syndrome was formerly understood to be a kind of autoimmune disease. Immunosuppressive agents were often used in some cases chronically resistant to routine anticoagulation treatment [3,5]. However, our case was not chronic; the clinical course became rapidly unstable and was accompanied by long lasting large skin ulcers on the lower extremities. The dilemma of treating Sneddon's syndrome is that immunosuppressive agents may help the remission of this disease, but would at the same time hinder the wound healing. However, IVIG is a fusion of immunoglobulin antibody only, so its effect on the wound is less than that of other agents. It is likely to be beneficial in the modulation of the disease activity while having a positive effect on the skin graft on the ulcer in this case.
In the case reported here, a split thickness skin graft on the lower extremity ulcer associated with Sneddon's syndrome took successfully. The other lesions healed and satisfactory results were obtained. Due to the extremely rare incidence of this syndrome, this report could be a good reference for selecting treatment options for patients with similar conditions.
Notes
No potential conflict of interest relevant to this article was reported.