Proximal-type Epithelioid Sarcoma Arising in the Inguinal Area
Article information
Epithelioid sarcoma is an uncommon soft tissue malignancy that is usually slow growing in the dermal or subcutaneous area of the distal extremity of young adults. Epithelioid sarcoma was first characterized as a distinct clinicopathologic finding by Enzinger [1] in 1970. It accounts for less than 1% of all soft tissue sarcomas [2]. Epithelioid sarcoma of the perineum and pubic regions is rarer than in the distal extremity and has a higher rate of local recurrence and distal metastasis. Epithelioid sarcomas are classified into a "distal type" that occurs in the upper and lower extremities and a "proximal type" that appears in the trunk and pubic area [3]. There have been few reports on proximal-type epithelioid sarcomas, and in most cases the reports contained no description of the reconstructive method used for treating the pelvic defects after the wide excision. In this case, we dissected a pedicle of sufficient length and were able to reduce the passage length of the flap by passing the flap under the rectus femoris muscle.
A 42-year-old woman was referred to our department for a recurred perineal area mass. Two years earlier, a general surgeon had excised a mass 2 cm in diameter from the same area. Pathology reported epithelioid sarcoma. The general surgeon recommended a wider excision margin; however, the patient refused additional surgery. At time of presentation at our department, a 7×4 cm mass (Fig. 1) at the site of the previous excision was noted. The round-shaped mass was fixed to adjacent tissues and without tenderness. The inguinal lymph nodes were not palpable. Computed tomography of the pelvic and inguinal area showed a soft tissue tumor of 2.4×2 cm diameter in the perineal area. Positron emission tomography did not reveal hypermetabolism in the internal structures of the pelvis and adjacent lymph nodes. The tumor abutted the deep fascia of the gracilis muscle, but did not involve the gracilis muscle. There was no evidence of distal metastasis.
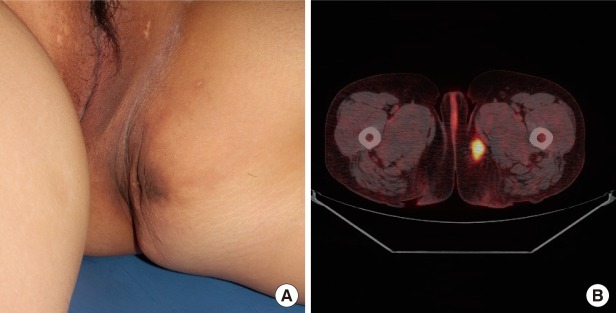
(A) Preoperative findings: 4×7 cm mass was palpable in the left perineal area. (B) Positron emission tomography-computed tomography findings: mass in subcutaneous plane.
We excised the mass with a 5-cm safety margin. The deep fascia of the internal compartment muscles of the thigh was preserved. After wide excision, the defect size was 17×14 cm (Fig. 2). The antero-lateral thigh flap was designed to be 18×15 cm size. The anterolateral thigh flap was elevated in the conventional method with a septocutaneous pedicle. The proximally-based flap was medially rotated and passed under the rectus femoris muscle to reach the perineal area. The flap donor site was covered with a split thickness skin graft. Additional lymph node dissection was not performed based on clinical staging.
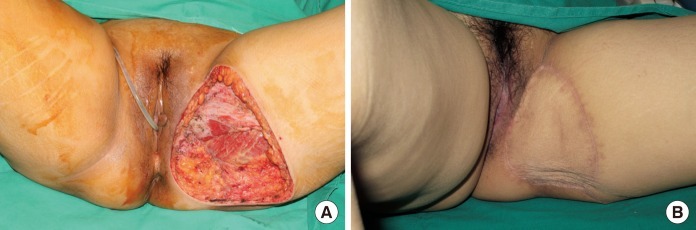
(A) After wide excision, 14×17 cm soft tissue defect. (B) At follow-up 7 months after reconstruction.
Pathology confirmed the diagnosis of epithelioid sarcoma with T2N0M0 staging. The histopathologic examination revealed the typical cell pattern of epithelioid sarcomas (Fig. 3). There were polygonal epithelioid cells and the cells had irregular vesicular nuclei with eosinophilic nucleoli.
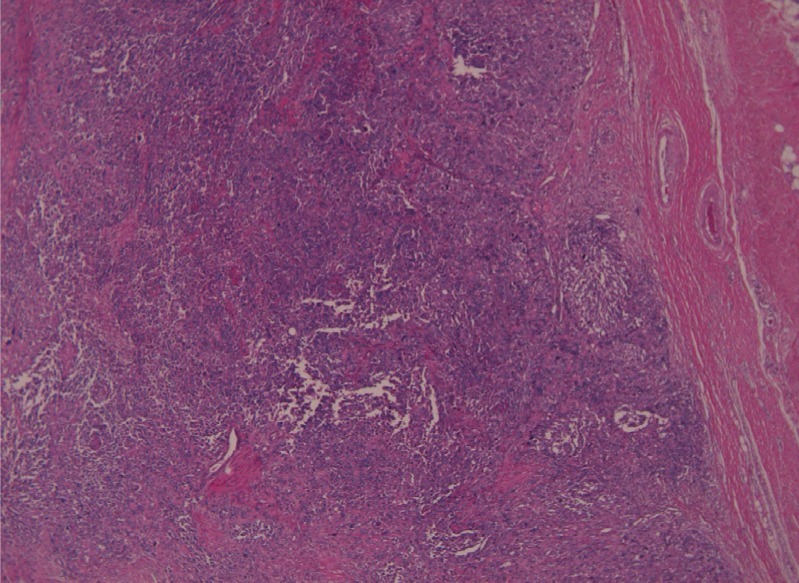
Microscopic finding showing epithelioid cells and spindle or polygonal cell components with atypia (H&E, ×40 high power field).
The wound healed uneventfully. The patient remains disease free at the time of this report (total 18 months follow-up) without any other adjuvant chemotherapy or radiation therapy. Also, no limitation of hip joint motion was noted.
Epithelioid sarcoma is a rare malignant soft tissue tumor of mesenchymal origin. It accounts for less than 1% of all soft tissue sarcomas and is usually slow growing, with a peak incidence in young adult men and occurrence predominantly in the extremities [2]. The proximal subtype occurs predominantly in adults (age range, 13 to 80; median, 40), with a slight predominance in men [4,5]. Epithelioid sarcoma is difficult to diagnose histologically, because histologic findings of epithelioid sarcoma are similar to those of other malignant sarcomas such as the synovial sarcomas, malignant rhabdoid tumors, or squamous cell carcinoma [1]. Confusion and misdiagnosis of the epithelioid sarcoma may lead to time consuming treatment and tumor recurrence.
Microscopically, epithelioid sarcoma is characterized by irregular nodules composed of relatively uniform, polygonal or epithelioid cell proliferation [2]. The mass is differentiated from the surrounding normal tissue with fibrous stroma and embedding spindle cells without a clear demarcation. On immunohistochemistry of epithelioid sarcoma, cytoplasmic immunoreactivity can be observed with cytokeratin and vimentin, and negative results for S100 and CD31 stainings [2]. These findings are useful for differentiating epithelioid sarcoma from other soft tissue tumors.
Epithelioid sarcoma requires a wide, total surgical excision with clear margins due to its high recurrence rate. Even with wide enbloc excision or amputation of the region, the reported recurrence rate of this sarcoma is 34% to 77% and the metastasis rate is about 40% [5]. Common metastasis sites are the lungs, regional nodes, scalp, bone, and brain. Proximal-type epithelioid sarcoma is even more aggressive than the distal type. Lymph node involvement is the most important prognostic factor. Young age at first diagnosis, female sex, and small size of tumor (less than 5 cm) are better prognostic factors. In our case, the patient was a woman, the size of tumor was less than 5 cm, and there was no evidence of lymph node metastasis.
In our case, we did not perform a lymph node dissection because inguinal lymph node resection is controversial. Lymph node removal is considered when it is large enough to be palpable on physical examination or appears in an imaging study to be suspiciously involved [2,5]. High-dose chemoradiotherapy may contribute to reducing the recurrence rate, but has not been proven to improve long-term survival [2]. In our patient, we did not perform any adjuvant therapy because of the many favorable prognostic factors mentioned above.
There are several options for reconstructing a soft tissue perineal defect. Regional flaps are of limited use for an extensive defect. Microsurgery in this region is limited by aesthetic contours and the complexity of the recipient vessel. The pedicled anterolateral thigh flap has a wide arc of rotation and is large enough to cover perineal defects without the need for microsurgery. In this case, we dissected a pedicle of sufficient length and were able to reduce the passage length of the flap by passing the flap under the rectus femoris muscle.
Notes
This article was noted as a poster at the 68th Congress of The Korean Society of Plastic and Reconstructive Surgeons on November 4-7, 2010 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.