An Unusual Case of a Malignant Peripheral Nerve Sheath Tumor
Article information
Malignant peripheral nerve sheath tumor (MPNST) is a rare soft tissue sarcoma comprising 5-10 percent of all soft tissue sarcomas [1]. MPNST frequently develops in young adults with preexisting plexiform neurofibroma in the majority of neurofibromatosis type 1 (NF-1) patients, accompanied by a prominent change in size and pain [1]. Most NF-1 shows benign growth, but in some people, a malignancy such as MPNST occurs. MPNST related to NF-1 has shown a highly aggressive pattern and a poor prognosis characterized by a high recurrence and metastasis rate, even after radical surgery [1].
MPNST usually presents as a solitary lesion. Lymph node metastasis in MPNST is rarely reported. In addition, distant skin and soft tissue metastases are very rare [2]. Herein we report an unusual case of MPNST occurring on the right thigh in a NF-1 patient.
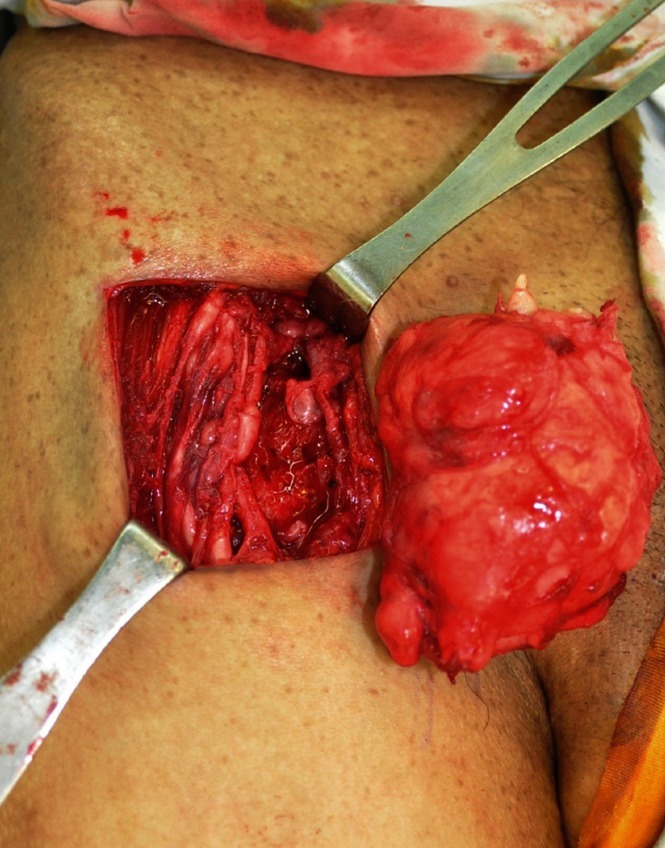
A 41-year-old male, with a previously known history of NF-1, visited with a rapidly growing mass in his right thigh, which presented with symptoms of right thigh pain over the previous six months (Fig. 1). Seven years earlier, he had undergone surgical treatment for a benign schwannoma on the posterior mediastinum and multiple neurofibromas of the chest soft tissues at our hospital. Physical examination revealed multiple soft nodules along with café-au-lait spots on the entire body. A thigh magnetic resonance image (MRI) showed an oval, heterogeneous, approximately 11.6 cm×6.8 cm×4.8 cm T1 low and T2 high signal mass lesion (Fig. 2). In addition, all neural foramina of the sacrum were widened. On the MRI, it was not fully possible to exclude malignant tumors and surgical biopsy was subsequently performed (Fig. 3). Histopathologically, the mass consisted of a proliferation of long spindle cells. In the cellular areas, it showed hyperchromatic nuclei and an increased number of mitotic figures (Fig. 4). Immunohistochemical analysis revealed positive results for vimentin, S-100, CD56, and CD99, and 30% positivity for Ki-67, whereas staining for desmin and CD34 yielded negative findings. Histologic examination confirmed the diagnosis of MPNST.
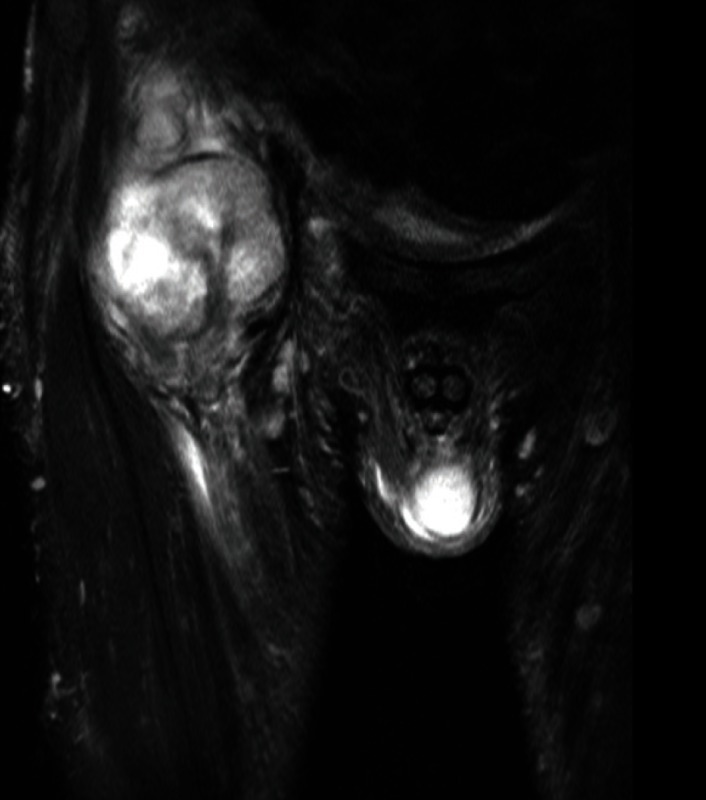
A thigh magnetic resonance imaging represented an oval, heterogeneous T1 low and T2 high signal mass lesion without a "target sign."
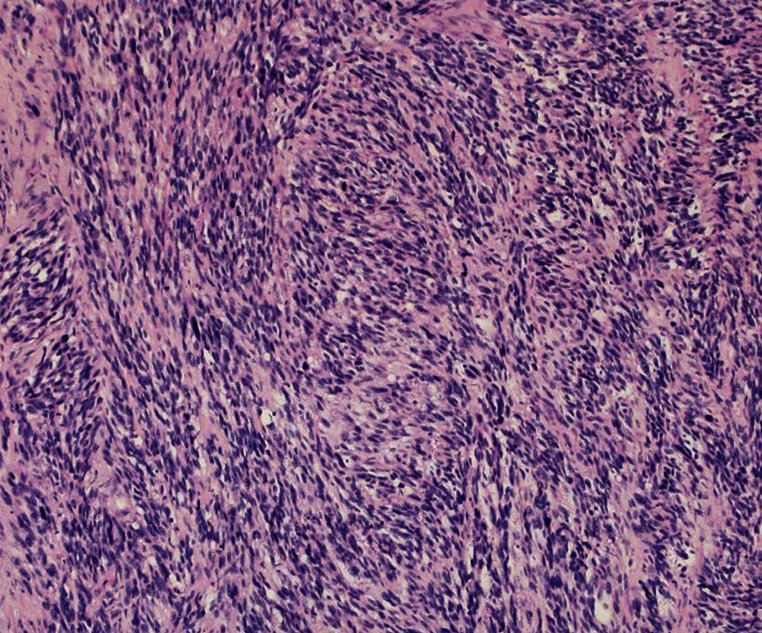
The dense cellular area showed fasciculated growth of hyperchromatic spindle cells (H&E, ×100). The tumor cells had abundant, faintly eosinophilic cytoplasm with elongated hyperchromatic nuclei. Frequent mitoses were noted, including atypical mitosis.
A positron emission tomography-computed tomography (PET-CT) examination of the whole body was performed in order to rule out any possible metastasis or additional lesions. Fluorine-18-fluorodeoxyglucose (18F-FDG) uptake was increased in the lower neck, left 4th rib, left lung, and right inguinal lymph node, suggesting metastatic MPNSTs and lymph node metastasis (Fig. 5). A chest CT revealed the pulmonary metastases. The patient was treated with adjuvant chemotherapy. Complete surgical excision was considered given the response to chemotherapy. He started chemotherapy with cisplatin 75 mg/m2 on day 1 and adriamycin 25 mg/m2/day on days 1 to 3, every three weeks. However, the patient's condition continued to worsen, and he died 7 months postoperatively.
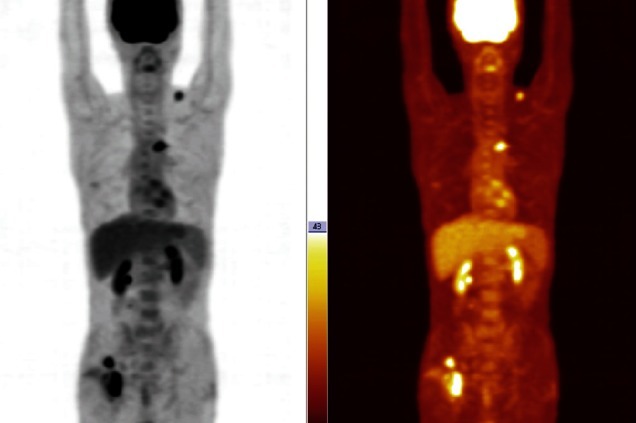
Positron emission tomography-computed tomography examination showed an increase in fluorine-18-fluorodeoxyglucose uptake in the left lower neck, left 4th rib, left lower lobe of the lung, and right inguinal lymph node.
The etiology of MPNST is unclear, but MPNST has a 10% post-irradiation incidence and 25% to 50% incidence with NF-1 in contrast to 0.001% in the general population [1]. Therefore, NF-1 patients should be closely monitored for the early detection of MPNST transformation. MPNST occurs at all ages but is more common between the ages of 20 and 50 [1]. MPNST is generally solitary and clinically occult [1]. However, it can be aggressive, locally invasive, and cause erosive changes to adjacent bone such as erosion of the rib and vertebral body and enlargement of the neural foramen [1]. Our patient showed wide neural foramina of the entire sacrum and bony deformity on the posterior arc of the left 4th rib. Although MPNST is rare, a sudden enlargement in the size of a mass and increased pain, particular in NF-1 patients, should be cause to suspect malignant transformation, such as our case.
MPNST in NF-1 patients may be difficult to detect. According to Bhargava et al. [3], T2-weighted MRIs of benign peripheral nerve sheath tumors showed round lesions with a central low intensity and a peripheral hyper-intense rim resembling a target. They claimed that this target sign appeared in all benign neurofibromas but only a few cases of MPNST. Our case also did not demonstrate the target sign. Additionally, fluorodeoxyglucose (FDG)-PET is sensitive and specific in identifying malignant change, particularly in NF-1 patients, because FDG-PET may help to avoid multiple surgical operations for benign neurofibromas [4]. Cardona et al. [4] reported that the FDG uptake value was significantly higher in MPNSTs, whereas benign neurofibromas did not demonstrate high FDG uptakes.
The most common distant metastatic site of MPNST is the lung, followed by bone and pleura [1]. Lymph node metastasis in MPNST, such as in our case, is rare [1]. In our patient, the lesions in the left lower lobe of the lung, left 4th rib, and lower neck lesion were determined to be metastasis from MPNST in an FDG-PET scan. In our case, FDG-PET showed an increased uptake in the lower neck, which was suggestive of the existence of metastatic soft tissue MPNST. However, distant skin and soft tissue are unusual sites of metastasis from all sarcomas [2]. The prognosis of MPNST is generally poor.
Histopathologically, MPNST is composed of spindle cells arranged in fascicular or whirling patterns. It is also characterized by hypercellularity, widespread hyperchromatic nuclei, increased mitotic activity, atypical mitoses, and the lack of differentiated cells [1]. Markers such as S-100, vimentin, Leu7, and myelin basic protein can be used [1]. Also, to distinguish from MPNST and benign peripheral nerve sheath tumor, the expression of Ki-67 may be used because the upregulation of Ki-67 is highly indicative of MPNST [5]. Our case was positive for S-100, vimentin, CD56, and CD99, with 30% positivity for Ki-67. The case was also negative for CD34, which is correlated with MPNST formation [1]. We report an unusual case of MPNST with distant soft tissue and lymph node metastasis in a NF-1 patient. Our case expands the understanding of the clinical behavior of MPNST, especially in NF-1 patients.
Notes
This work was supported in part by the Soonchunhyang University Research Fund.
No potential conflict of interest relevant to this article was reported.