Giant Epidermal Cyst on Posterior Scalp
Article information
Epidermal cysts are common subcutaneous tumors that usually involve the scalp, face, neck, back, or trunk. Conventional epidermal cysts are less than 5 cm in diameter. Giant epidermal cysts with a diameter of 5 cm or more are rare but have been reported [1]. We report a case of a giant epidermal cyst on the posterior scalp.
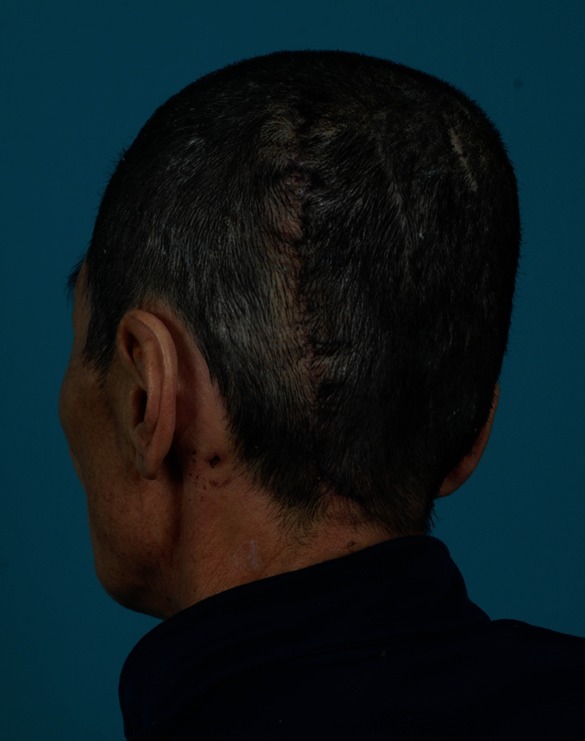
A 58-year-old male patient was referred to our institution with a huge mass of the left posterior scalp. The patient first recognized the mass on the posterior scalp area about 30 years previously. The mass had been growing slowly ever since, but during the most recent 3 years, the mass had enlarged noticeably. At the time the patient visited our clinic, the mass grossly measured 20 cm×15 cm×10 cm. The mass was soft, without pain or tenderness, and had no signs of infection (Fig. 1). The patient had no underlying disease except diabetes, which had been controlled with oral medication for 10 years.
Preoperative photograph. The mass on left occipitoparietal area was grossly measured to be about 20 cm×15 cm×10 cm.
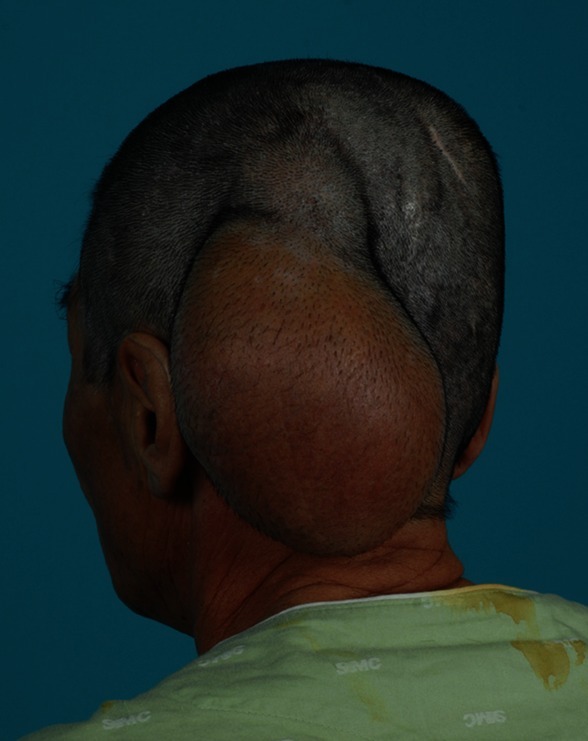
Preoperative magnetic resonance imaging (MRI) showed a well-circumscribed, unilocular 18 cm×14 cm×8 cm cystic lesion on the left occipitoparietal area without skull or brain involvement. The lesion had a homogeneous, high-intensity signal on T2-weighted images (Fig. 2).
Magnetic resonance image.
Preoperative magnetic resonance imaging showed a well-circumscribed, unilocular 18 cm×14 cm×8 cm cystic lesion without skull or brain involvement.
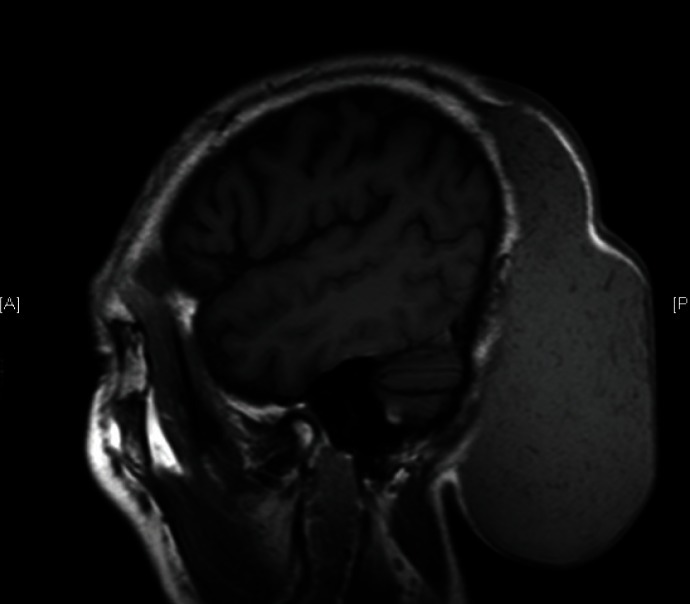
A complete excision was performed under general anesthesia. An S-shaped incision with a horizontal extension line was designed with consideration of redundant skin, and the dissection was extended from the subcutaneous layer to the subgaleal plane to expose the mass. Neovascularization was observed in the area surrounding the mass and complete ligation was performed to achieve clear visualization of the dissection plane. After confirming encapsulation of the mass, it was completely excised. The mass weighed 550 g. We resected the redundant skin that had expanded to accommodate the mass and performed primary closure. The wound healed without any problems or complications (Fig. 3).
The gross appearance of the mass showed that it had an outer membranous capsule with inner yellow and brown debris (Fig. 4). The cystic lumen was filled with degenerated and necrotic keratinaceous debris on histologic findings (Fig. 5).

Excised tumor, gross view. The mass was completely excised with ligation of the neovascularized vessels and weighed 550 g.
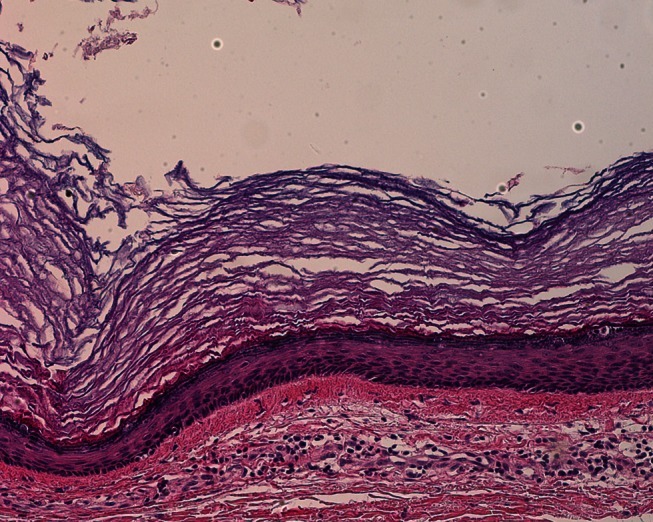
Histologic findings (H&E, ×16). There is an outer membranous capsule with inner degenerated and necrotic keratinaceous debris.
No clinical sign of recurrence was observed at the 3-month follow-up visit. The patient was satisfied with the aesthetic results of the operation.
An epidermal cyst is a common benign tumor that is frequently encountered by plastic surgeons. Epidermal cysts are usually slow-growing masses ranging from a few millimeters to a few centimeters in diameter. A giant epidermal cyst is more than 5 cm in diameter, with few cases being described since Rios Arizpe and Ocampo Candiani [2] reported an epidermal cyst in the middle sternum that was 11.5 cm×7 cm.
Proposed causes of epidermal cysts include congenital factors, squamous metaplasia of columnar epithelial cells, downward growth of epidermal cells with inflammation after obstruction of a hair follicle, and growth of implanted fragments of the epidermis within the dermis after trauma [3]. They are usually unilocular, but multilocular lesions are more common in giant epidermal cysts [4]. In our case, the cyst as appeared with a unilocular pattern.
It is necessary to conduct a physical examination on giant epidermal cysts while bearing in mind the possibility of other diagnoses. For confirmative diagnosis of giant epidermal cysts, ultrasonography, computed tomography, or MRI can be performed to exclude other tumors such as lipomas, neurofibromas, or hemangiomas. Ultrasonography is a readily available and cost-effective diagnostic method. The sonographic appearance of epidermal cysts shows mostly well-circumscribed, mildly echogenic masses confined to the subcutaneous layer. They might show internal linear echogenic reflections, dark clefts, or a hypoechoic rim. On MRI, T2-weighted images of a high signal mass, possibly with low signal intensity debris, and thin rim enhancement on T1-weighted images strengthen this preoperative diagnosis [5]. MRI, in particular, also shows the extent and the depth of the lesion with a characteristic high signal on T2-weighted images.
For epidermal cysts, complete excision is the treatment of choice. During surgery, the intraepidermal layer should be included for complete excision. Incomplete excision can induce chronic inflammation or recurrence. Therefore, complete excision is essential for treating epidermal cysts. For giant epidermal cysts, excision of redundant skin is needed to achieve good aesthetic results. Histopathologic examination is necessary for diagnosis.
Although rare, a case of malignant change of benign epidermal cysts is possible.
Epidermal cysts are a common subcutaneous tumor that can occur anywhere in the body, including the head and neck. However, reports of giant epidermal cysts with a diameter of 5 cm are rare, especially in the head and neck area. We reported a case of a giant epidermal cyst of the posterior scalp with several images.
Notes
No potential conflict of interest relevant to this article was reported.