Reconstruction of a Rare Palate Defect Originating from Extranodal Natural Killer/T-Cell Lymphoma
Article information
Extranodal natural killer (NK)/T-cell lymphoma is a very rare and aggressive form of non-Hodgkin's lymphoma, derived from NK cells [1]. The primary site of extranodal NK/T-cell lymphoma is the nose; however, it often extends to adjacent tissues, including the nasopharynx, paranasal sinuses, and oral cavity. Progression of this disease leads to erosion of the palate, accompanied by destruction of the palatal structure, which is an extremely rare condition, and the prognosis is usually poor. A palate defect is difficult to repair conservatively. It causes speech disorders and oronasal regurgitation, significantly impacting patients' quality of life. To our knowledge, a case of reconstruction of a palate defect originating from extranodal NK/T-cell lymphoma has only been reported once in the literature worldwide, but not yet in Korea [2]. In the present study, we report a rare palate defect originating from extranodal NK/T-cell lymphoma that was treated with radial forearm free flap (RFFF) surgery with favorable results.
A 26-year-old male patient had symptoms of chronic sinusitis, night sweating, and a 5-kg weight loss over 5 months. Nasopharyngoscopy showed that the majority of the hard palate was notably absent and ulcerative, and an ill-defined mucosal lesion was detected. Neck computerized tomography showed a heterogeneously enhancing mass lesion on the right nasoethmoidal area (Fig. 1). A biopsy of the palatal and nasal mucosa showed diffuse infiltration of medium-sized lymphoma cells with irregular nuclear contours. Extranodal NK/T-cell lymphoma positive for CD56 was diagnosed by immunohistochemistry (Fig. 2). The patient was started on adjuvant chemotherapy with four cyclophosphamide, adriamycin, vincristine, and prednisone (CHOP) cycles and radiation therapy. In follow-up two years later, the patient was in complete clinical remission. The result of palatal and nasal mucosal biopsy showed no evidence of malignancy. Neck computerized tomography showed no evidence of recurrent tumor in the sinonasal cavity and neck (Fig. 3). The patient was transferred to our hospital for reconstruction due to a 5 cm×5 cm defect in his hard palate (Fig. 4). He complained of oronasal regurgitation, dysphagia, and hypernasal voice resonance. In the perceptual speech evaluation performed by a speech-language pathologist, the patient was noted to have severe hypernasality and audible nasal emission. The palate defect was repaired surgically with a RFFF under general anesthesia. With the patient in the supine position and a tourniquet inflated, an incision was made on the ulnar flap margin in order to include the deep fascia of the forearm. The 6 cm×8 cm rectangularly shape flap was designed to fit the size of the palatal defect. After the full dissection, the total length of the pedicle harvested was 11 cm. At the same time, a 5 cm×15 cm, 8/1,000 inch in thickness, split-thickness skin graft was harvested from the right thigh. Then, the harvested split thickness skin graft was sutured to the RFFF on the fascial side. The defect on the oral lining was covered with the RFFF skin paddle, and the nasal lining was covered with the RFFF fascia, with the split thickness skin graft. The pedicles were anastomosed with the left facial artery and concomitant vein in an end-to-end fashion. The postoperative course was uneventful, and no complications were observed. Two years after surgery, the patient remains in good health, without recurrence, and shows good aesthetic results (Fig. 5). In follow up perceptual speech evaluations, the patient was noted to have significantly decreased hypernasality, with greatly improved speech intelligibility. Nasalance scores were 59%, which was measured with a nasometer (Model 6450, KayPENTAX, Lincoln Park, NJ, USA). A cutoff value of 63% was used; that is, nasalance scores higher than 63% were considered to indicate hypernasality.
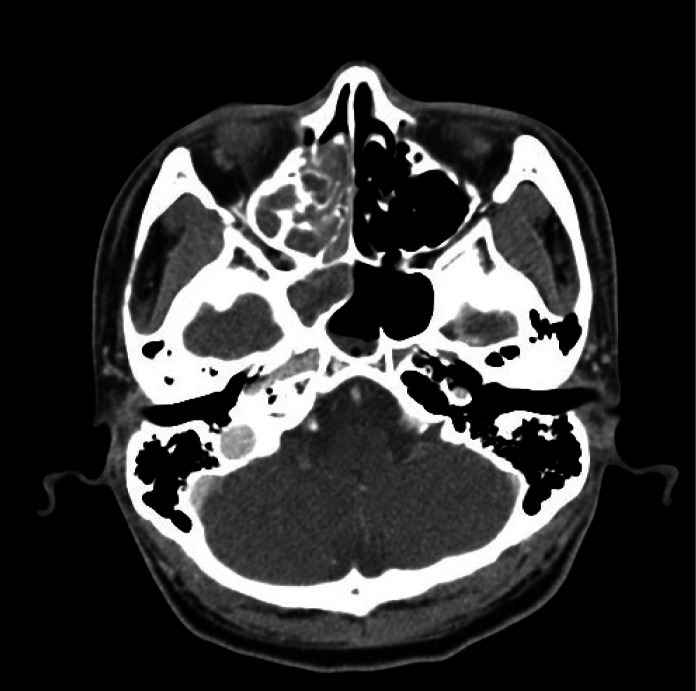
Neck computed tomography image at diagnosis: heterogeneously enhancing mass lesion on the right nasoethmoidal area.
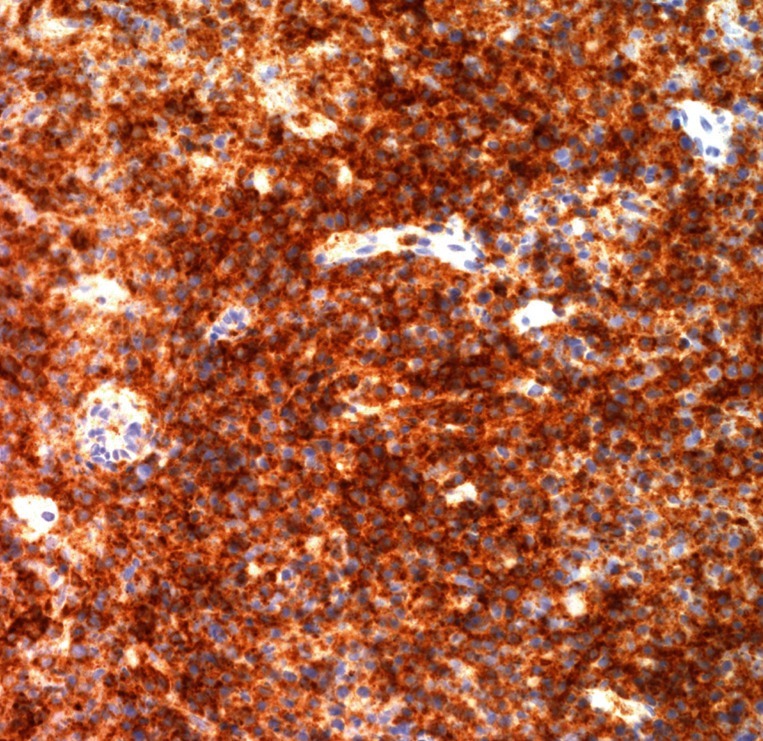
Immunohistochemical findings of the extranodal natural killer/T-cell lymphoma marker: ×400. That CD56 shows that atypical lymphoid cells react positively with the marker and appear brown.
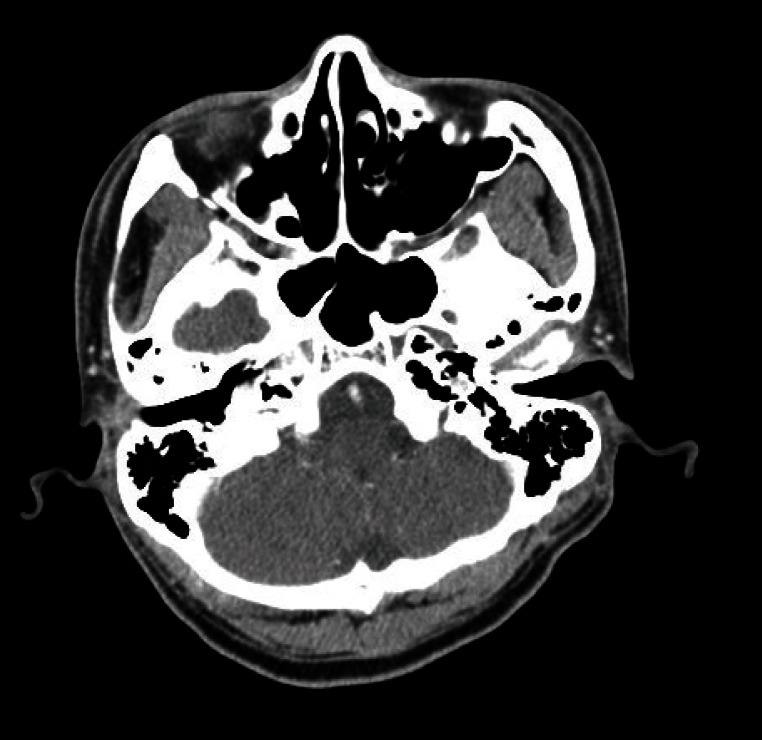
Neck computed tomography image after complete remission of extranodal natural killer/T-cell lymphoma: no evidence of recurrent tumor.

Preoperative view: a 26-year-old man with a palatal defect originating from extranodal natural killer/T-cell lymphoma.
Extranodal NK/T-cell lymphoma is known as a rare form of non-Hodgkin's lymphoma. Patients' subjective symptoms are non-specific, such as nasal obstruction or purulent nasal discharge. These findings are easy to misdiagnose as chronic sinusitis, or they result in a delayed diagnosis. Diagnosis of extranodal NK/T-cell lymphoma is confirmed by histologic and immunohistochemistry analysis. Immunohistochemical staining demonstrates positive reactions to NK cell marker CD56 and a negative reaction to CD3, which meet the description of markers positive for extranodal NK/T-cell lymphoma [3]. Extranodal NK/T-cell lymphoma is an aggressive malignancy with rapid progression. The 5-year overall survival rate in early stage disease is more than twice that of the advanced stage at diagnosis: 54% versus 20% [4]. Highly aggressive types involve anatomical destruction, such as septal perforation and palatal perforation. The treatment for this, combined with radiation therapy and chemotherapy, could prolong long-term survival and achieve greater local control. One month following the completion of planned therapy, the response to treatment should be documented by history, physical examination, flexible nasal endoscopic examination, and an imaging study [5]. In highly aggressive cases, it is difficult for palatal perforation to heal conservatively, and its symptoms, such as speech disorder and oronasal regurgitation, can significantly impact patients' quality of life. Following the completion of treatment, patients should be evaluated for damage to the neighboring bony structures to assess whether reconstructive surgery is needed [5]. Surgical reconstruction must take into account the complicated anatomy, postoperative speech, and swallowing function. As many studies have reported, methods of palate reconstruction include palatal local flap, folded free flap, and free flap combined with pharyngeal flap. RFFF is the most common flap used to reconstruct the oropharynx and oral cavity. The main advantage of RFFF is that the forearm skin is thin and pliable enough to adapt easily to the shapes of defects and is suitable for obliterating dead space in defects.
In conclusion, extranodal NK/T-cell lymphoma is a rare type of lymphoma. Because of its aggressive behavior and the high incidence of tumor recurrence, annual follow-up with detailed imaging studies and histologic and immunohistochemistry analysis are recommended. Furthermore, considering the poor quality of a patient's life due to speech disorders and oronasal regurgitation caused by palate defects, the RFFF is a valuable option for restructuring composite and three-dimensional palatal defects.
Notes
No potential conflict of interest relevant to this article was reported.
