Usefulness of a Lateral Thoracodorsal Flap after Breast Conserving Surgery in Laterally Located Breast Cancer
Article information
Abstract
Background
Breast-conserving surgery is widely accepted as an appropriate method in breast cancer, and the lateral thoracodorsal flap provides a simple, reliable technique, especially when a mass is located in the lateral breast. This study describes the usefulness of a lateral thoracodorsal flap after breast conserving surgery in laterally located breast cancer.
Methods
From September 2008 to February 2013, a lateral thoracodorsal flap was used in 20 patients with laterally located breast cancer treated at our institution. The technique involves a local medially based, wedge shaped, fasciocutaneous transposition flap from the lateral region of the thoracic area. Overall satisfaction and aesthetic satisfaction surveys were conducted with the patients during a 6-month postoperative follow-up period. Aesthetic results in terms of breast shape and symmetry were evaluated by plastic surgeons.
Results
The average specimen weight was 76.8 g. The locations of the masses were the upper lateral quadrant (n=15), the lower lateral quadrant (n=2), and the central lateral area (n=3). Complications developed in four of the cases, partial flap necrosis in one, wound dehiscence in one, and fat necrosis in two. The majority of the patients were satisfied with their cosmetic outcomes.
Conclusions
Partial breast reconstruction using a lateral thoracodorsal flap is well matched with breast color and texture, and the surgery is less aggressive than other techniques with few complications. Therefore, the lateral thoracodorsal flap can be a useful, reliable technique in correcting breast deformity after breast conserving surgery, especially in laterally located breast cancer.
INTRODUCTION
Breast-conserving surgery is widely performed for the treatment of early-stage breast cancer patients, and has been substantially developed over several decades. Between breast-conserving surgery and total mastectomy, no significant statistical differences in local disease recurrence or survival rate have been found [1,2]. Breast-conserving surgery requires appropriate excision margins to achieve the desired aesthetic results. Moreover, new developments have been primarily aimed at improving the patient's quality of life [3].
Some reports have suggested that partial breast reconstruction after a breast-conserving surgery does not guarantee acceptable aesthetic results; breast asymmetry was found in many patients, and poor aesthetic results were obtained in approximately 20% to 30% of patients [4,5]. Success in oncoplastic breast surgery is determined by the surgeon's experience, tumor location, size of the residual breast, and tumor size, among other factors [6]. When the breast is large enough, such as those of many Westerners, glandular reshaping after partial mastectomy can be performed using residual breast tissues. However, in ethnic East Asians, who generally have small breasts, the partial breast reconstruction method after partial mastectomy can have limitations and requires sufficient tissue replacement using local flaps from surrounding autologous tissues that match the volume of the excised area [7]. In particular, partial breast reconstruction using lateral thoracodorsal flaps can be useful when the defect site is laterally located.
Lateral thoracodorsal flap surgery was first introduced by Holmstrom and Lossing [8] as an implant-based teche using local flaps for delayed postmastectomy breast reconstruction. Woerdeman et al. [9] then reported its clinical usefulness, albeit with precautions. Furthermore, the clinical usefulness of immediate partial breast reconstruction using lateral thoracodorsal flaps after a breast-conserving surgery was strongly recommended by Munhoz et al. [10].
The lateral thoracodorsal flap procedure has the advantage of being similar in texture and color to the native breast; in addition, morbidity of the donor site is minimized without sacrificing muscles or nerves, implying less invasiveness, a shorter hospital stay, and good aesthetic and functional results. For these reasons, we chose to perform immediate breast reconstruction with the lateral thoracodorsal flap procedure in cases of laterally located cancer tumors. In our study, we demonstrated the successful use of the technique, which achieved satisfactory results without incurring other complications except 4 cases of minor complications.
METHODS
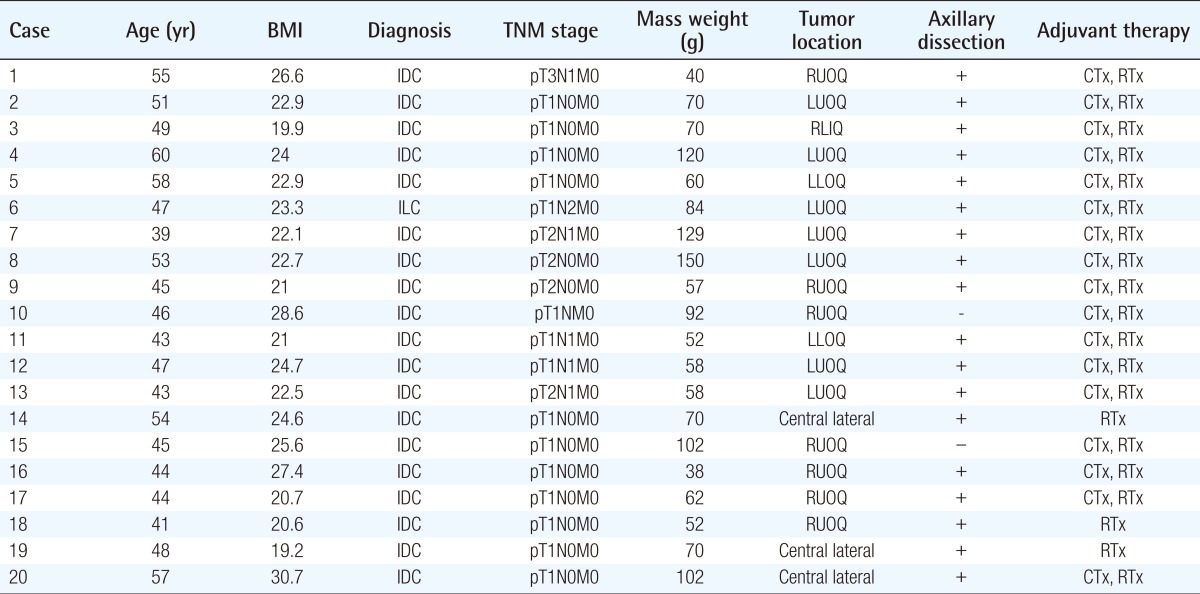
The subjects of this study were 20 patients who underwent partial breast reconstruction with a lateral thoracodorsal flap. These patients were selected from among patients who underwent breast-conserving surgery in our hospital between September 2008 and February 2013. All the surgical procedures were performed by a single surgeon. From the patients' medical and surgical records, information such as underlying disease, age, and body mass index, as well as the weight and surface area of skin excised during surgery, history of smoking or radiation treatment, and complications were obtained and assessed. In addition, a satisfaction survey, including breast symmetry and shape, and overall aesthetic effects, was conducted with the patients and doctors 6 months after the surgery.
Surgery was performed under general anesthesia. If no cancer cells were detected in the marginal area of the tumor on frozen section analysis of the surgically excised tissues (approximately 2 cm) and normal tissues surrounding the initial tumor location, oncoplastic breast surgery was performed. Meanwhile, total excision of the axillary lymph nodes was performed if cancer cells were found in the sentinel lymph nodes in the same axilla.
Surgical technique
In the lateral thoracic area, a wedge-shape flap was designed, applying the pinch test, which uses the thumb and index finger, to measure the remaining tissue. The axis of the flap was set along the line of the inframammary fold, extending toward the lateral and posterior sides, and the base of the flap was designed to lie on the anterior axillary line so that the postoperative scar could be hidden under the brassiere line. The base of the flap was set at 5 to 7 cm, as determined by the pinch test, and the length of the flap was measured to be 7 to 15 cm.
When the flap was elevated, with caution taken to include the fascia of the serratus anterior and latissimus dorsi muscles, the skin, subcutaneous tissue, and fat were also included. A lateral thoracodorsal flap is a perforator-based fasciocutaneous flap originating from the lateral intercostal artery; therefore, caution was taken to include the fascia from the superficial to the deep layer during dissection. Dissection was performed with 2 or 3 perforators as flap center after Doppler tracing to find the perforators. The flap was transposed laterally to the breast excision site and stapled temporarily on the skin; both breasts were compared in the lying and sitting positions to determine the mold of the flap and shape of the breast, and the flap was partially deepithelized when necessary. A drainage tube was inserted, and interrupted and subcuticular sutures were performed layer by layer. Depending on the shape of the breast defect, a V-Y advancement flap implantation was performed as an adjunct to the existing lateral thoracodorsal flap procedure.
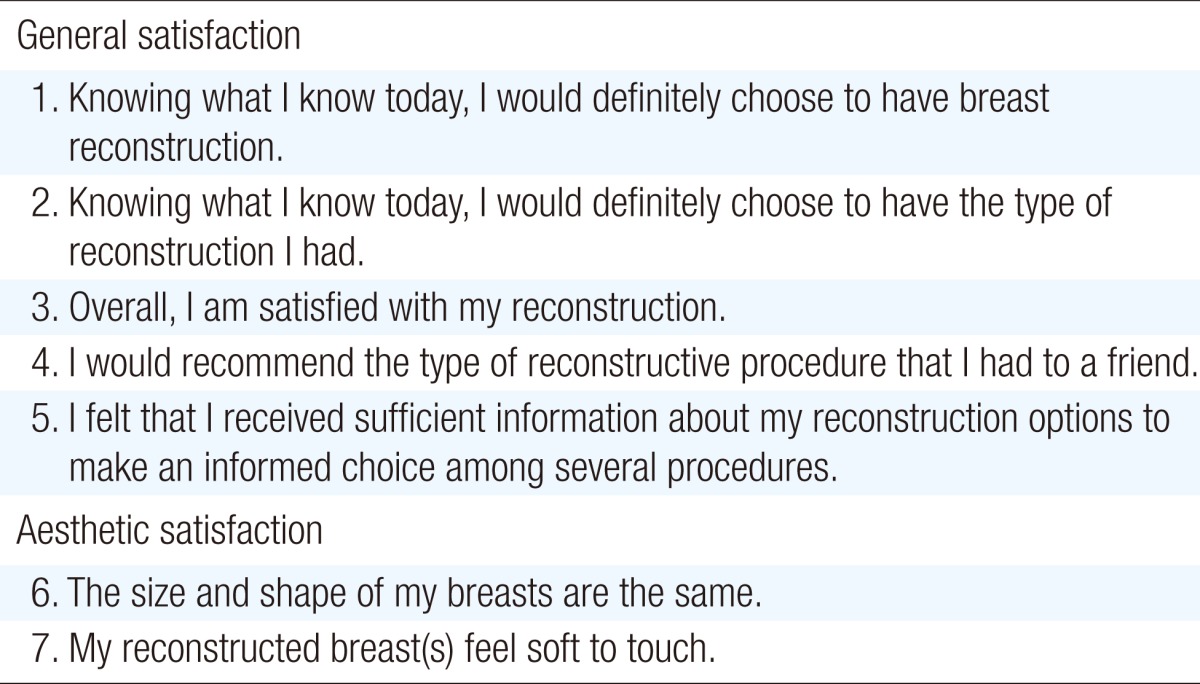
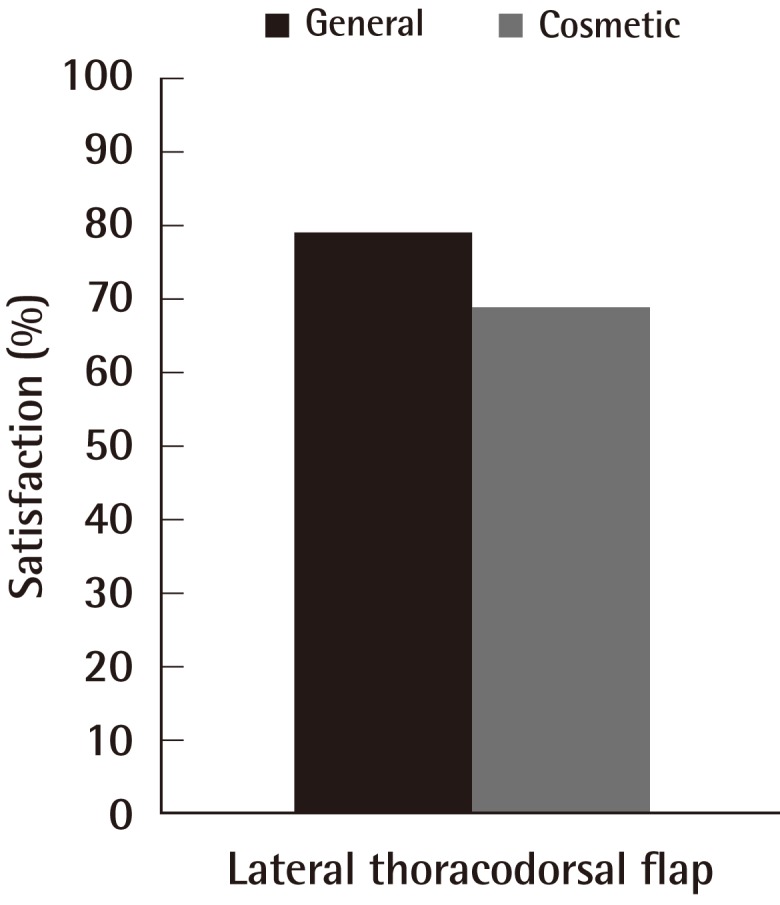
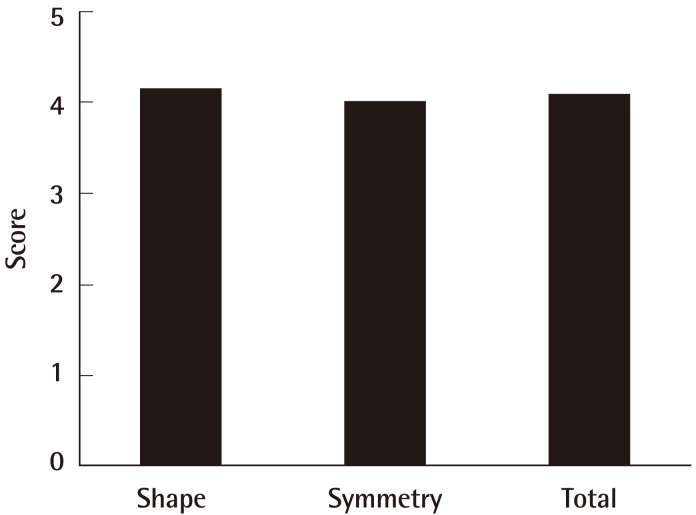
Overall satisfaction and aesthetic satisfaction surveys, based on the Modified Michigan Breast Reconstruction Outcome Survey, were conducted with the patients at 6 months postoperatively [9] (Table 1). Two patients who were followed up for just 2 months could not be evaluated with the survey. Five survey items pertained to overall patient satisfaction with the breast reconstruction surgery, and 2 items investigated aesthetic satisfaction. The original phrase "the implant, transverse rectus abdominis myocutaneous, deep inferior epigastric perforator, or latissimus procedure" was changed to "lateral thoracodorsal flap" in our questionnaire. The score ranged from 1 to 5, with 1 indicating "very dissatisfied" and 5 "very satisfied." Scores of 4 and 5 were treated as satisfaction; and 1, 2, and 3, as dissatisfaction (Fig. 1). Aesthetic results in terms of breast shape and symmetry were scored from 1 (bad) to 5 (very good) by 3 surgeons based on pictures taken after the surgery. Fig. 2 presents the survey results quantified according to the scoring system.
RESULTS
A total of 20 patients who underwent partial breast reconstruction using a lateral thoracodorsal flap were selected from among patients who underwent breast-conserving surgery in our hospital between September 2008 and February 2013. The mean age of the patients was 48.5 years (range, 39 to 60 years), and the mean follow-up observation period in the outpatient department was 8 months (range, 2 to 28 months). When the follow-up duration of the patients reached 28 months, no more follow-up at the clinic was carried out. Among our patients, 1 had diabetes and 1 was a chronic hepatitis carrier. The mean weight of the excised tumor was 76.8 g (range, 40 to 150 g), and the tumor was most frequently (15 patients) located in the upper lateral part, followed by the middle lateral part in 3 patients and lower lateral part in 2 patients (Table 2). The tumor diagnosis was invasive ductal carcinoma in 19 cases and invasive lobular carcinoma in 1 case. Chemotherapy was performed after surgery in 17 cases, and radiotherapy was performed in all of the cases after surgery. Among the 20 postoperative patients, only 1 had an incidence of dehiscence, 1 had partial skin necrosis, and 2 had fat necrosis, but these complications were resolved with secondary conserving treatments.
Of the patients, 79% and 69% reported a score of 4 or 5, indicating "satisfaction" in the overall satisfaction and aesthetic satisfaction surveys, respectively (Fig. 1). In the surgeons' assessment, the overall aesthetic score was 4.15 for breast shape and 4.01 for symmetry, with a mean aesthetic score of 4.08, indicating satisfactory overall results (Fig. 2).
DISCUSSION
Radical mastectomy or modified mastectomy had been performed as a standard treatment regardless of the stage of breast cancer until the 1970s. Since then, studies have gradually turned their focus to developing methods to conserve breast tissues as much as possible, especially in cases of small tumors, without affecting the survival rate. Veronesi and Zurrida [12] reported the safety of partial mastectomy for tumors smaller than 2 cm, without metastasis to the lymph nodes. Meanwhile, Fisher et al. [13] reported that the patient survival rate was not affected by a tumor size smaller than 4 cm when radiotherapy was executed after partial mastectomy. Since then, breast-conserving surgery has undergone further development.
Over the past 30 years since the usefulness of breast-conserving surgery was firmly verified, surgical methods for breast cancer have evolved and numerous studies have been conducted with the aim of improving aesthetic results and patient quality of life while reducing the risk of undergoing surgery and radiotherapy [14]. Early-stage breast cancer detection has been facilitated by mammography and ultrasonography. Studies on improving patient quality of life involve conserving tissues of the breasts and performing precise radiotherapy. However, predicting aesthetic outcomes after partial mastectomy has often been difficult, and numerous incidences of asymmetry and aesthetically undesirable outcomes and adverse events in daily life have been reported [15]. Consequently, interest in the aesthetic aspect of breast-conserving surgery has increased, and methods that safely improve aesthetic effects by oncoplastic breast surgery have been developed. Along with this trend, some studies have tried to ensure an optimal balance between the risk of local recurrence and the aesthetic results of breast-conserving surgery. Fitoussi et al. [16] reported satisfactory results in 540 patients.
The determining factors for oncoplastic breast surgery include the size of the excised breast tissue, tumor location, breast size, and radiotherapy. If the tumor is located on the lateral part of the breast, the resulting breast shape might appear unnatural because of a depression, or a scar may form after partial mastectomy is performed. The nipple areola complex occasionally requires excision, which can have an aesthetically undesirable result when only partial mastectomy is performed. A local flap is useful for partial breast reconstruction after tumor excision because the skin texture and color are similar and the surgical technique is simple, with a short recovery period, which is advantageous when chemotherapy or radiotherapy is required after the surgery. Lateral thoracodorsal flaps for the oncoplastic breast surgery in the authors' cases was indicated when breast tumors were located on the lateral side and the weight of the excised masses was below 100 g. If the excised masses which were located on lateral side of the breast were over 100 g, other methods of breast reconstruction such as thoracodorsal artery perforator flap or mini latissimus dorsi flap were performed [7].
Lateral thoracodorsal flap was first performed by Holmstrom and Lossing [8] in delayed breast reconstruction, whereby a method using a local flap along with an implant was introduced. Woerdeman et al. [9] later used lateral thoracodorsal flaps for immediate breast reconstruction; expanded its application to subjects by de-epithelization of the flap; investigated risk factors such as patient age, obesity, medical history, and smoking; and reported its usefulness and precautions. The usefulness of immediate breast reconstruction using lateral thoracodorsal flaps has also been reported by Munhoz et al. [10], and overall aesthetically satisfactory results according to plastic surgeons and clinical usefulness have been reported. The base of the flap was transposed to the medial portion of the breast, and the wedge-shaped fasciocutaneous flap on the lateral thorax was elevated for transposition to the defect site; a lateral breast defect can be filled to create a natural mastoptosis. Generally, an aesthetically satisfactory result is achieved by creating a pear shape. In addition, similarity of skin texture or color with the original inframammary fold can be maintained, and morbidity of the donor site can be minimized without sacrificing muscles or nerves as skin fascia flaps. A scar is created on the donor site of the flap on the lateral thoracic area, but it can be hidden under breast supports.
Munhoz et al. [10] performed oncoplastic breast surgery with a lateral thoracodorsal flap in 34 patients. In 58.8% of these patients, the tumors located in the upper lateral area were targeted; tumors located in the upper lateral area were preferred, and patients with a small or medium degree of mastoptosis were targeted. Garcia et al. [17] performed oncoplastic breast surgery using lateral thoracodorsal flaps for tumors located in the upper lateral areas. Among the 20 patients treated in our hospital, 15 (75%) had tumors in the upper lateral area. For tumors located in the middle or lower lateral area, if the shape of the defect site of the breast was extended perpendicularly to the base of the flap as a result of the tumor excision, additional dissection was performed at the base of the flap, unlike in the current lateral thoracodorsal flap design, to create a V-Y advancement flap without transposing the flap, and to reconstruct the breast by filling the defect site.
Munhoz et al. [10] reported that of 18 patients, 3 experienced partial flap necrosis (8.8%) and 2 had fat necrosis (5.8%) as complications of breast reconstruction using lateral thoracodorsal flaps. Woerdeman et al. [9] reported that flap-related complications occurred in 18.3% of cases, of which 11.6% were partial flap necrosis and 3.3% were fat necrosis. Moreover, the suggested length of the flap should be kept shorter than 17 cm, considering the statistical significance between partial flap necrosis and flap length. The authors also reported that partial flap necrosis increased in proportion to the flap length. The standard flap length used in our hospital is 7 to 15 cm. Of the 20 patients, 1 showed partial flap necrosis; 1, dehiscence; and 2, fat necrosis. However, these were resolved through secondary conserving treatment. Though patients who underwent postoperative radiotherapy did not experience a change in the flap condition throughout the follow-up duration, the state of the flaps should be checked in long-term follow-up.
In most cases of breast-conserving surgery, radiotherapy is performed as an adjunct treatment. Unlike in oncoplastic breast surgery through breast reduction, in lateral thoracodorsal flap implantation, the exact location can be targeted during radiotherapy because the location of the existing breast cancer excision does not change. In addition, it is easy to locate the remainder of the cancer tumor and re-excise the peripheral area because the original cancer location is maintained even if postmastectomy permanent pathology detects the presence of cancer cells in the periphery. However, thorough planning with the breast surgeon is needed, and close cooperation during surgery is necessary, as there can be a problem with vascular supply if excessive dissection is performed around the inframammary fold when the tumor is located in the lateral inferior portion.
When the breast is large, as those of some Westerners, glandular reshaping can be performed with the remaining breast tissues after the partial mastectomy. However, when the breast is small, as those of many East Asians, the volume of the remaining breast tissue can be insufficient after a partial mastectomy; thus, a sufficient quantity of tissue to fit the volume of the excised area is needed, using surrounding autologous tissues to create a local flap. Especially when the breast cancer is located in the lateral portion, a lateral thoracodorsal flap can be relatively simple, with few complications or cases of decreased function in the donor site. In addition to the advantage of having a similar skin texture and color to the breast tissues, reliable results were obtained (Figs. 3, 4). No major complications were encountered in the lateral breast cancer patients who underwent immediate breast reconstruction surgery using lateral thoracodorsal flaps after breast-conserving surgery in our hospital. Though the satisfaction scores by the patients and plastic surgeons differed, the results of the survey conducted with the patients and plastic surgeons provide evidence of satisfactory outcomes and good aesthetic results. The scores by patients were often subjective while the scores by plastic surgeons were often more objective. It seems that the difference in the satisfaction scores between the two groups occurred based on the difference between subjective and objective opinion. The lateral thoracodorsal flaps can be useful for oncoplastic breast surgery, and satisfactory results can be obtained if a thorough preoperative plan is set up in consultation with the surgeon and implemented in appropriate patients.
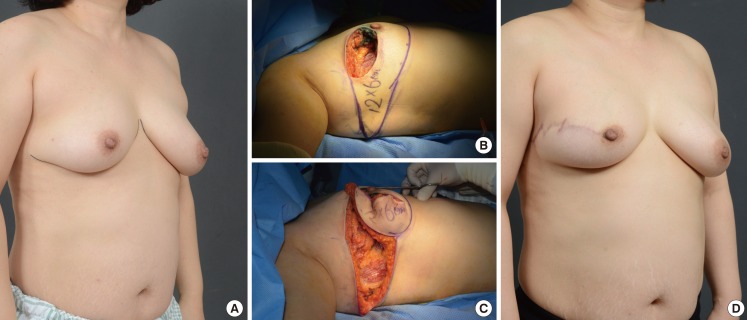
Case 1 with lateral thoracodorsal flap
A 45-year-old woman with invasive ductal carcinoma in the right breast. (A) Preoperative design view of patient. (B) Intraoperative view of the designed lateral thoracodorsal flap after partial mastectomy (weight of tumor, 92 g). (C) Intraoperative view of the elevated flap. (D) 4-month postoperative outcome.
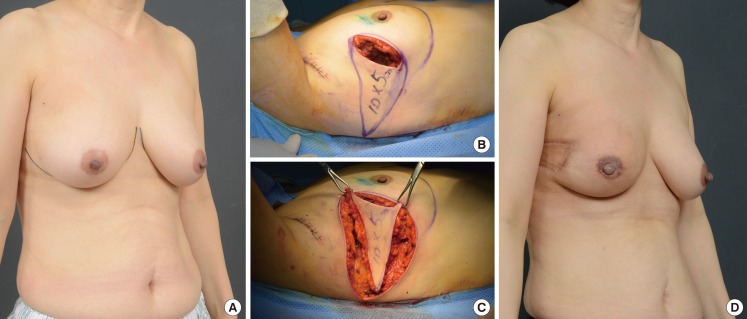
Case 2 with lateral thoracodorsal flap
A 48-year-old woman with invasive ductal carcinoma in the right breast. (A) Preoperative design view of patient. (B) Intraoperative view of the designed lateral thoracodorsal flap after partial mastectomy (weight of tumor, 70 g). (C) Intraoperative view of the elevated flap. (D) 4-month postoperative outcome.
Notes
This research was supported by Kyungpook National University Research Fund, 2012.
No potential conflict of interest relevant to this article was reported.