The Effect of Breast Hypertrophy on Patient Posture
Article information
Abstract
Background
One of the reasons women with macromastia chose to undergo a breast reduction is to relieve their complaints of back, neck, and shoulder pain. We hypothesized that changes in posture after surgery may be the reason for the pain relief and that patient posture may correlate with symptomatic macromastia and may serve as an objective measure for complaints. The purpose of our study was to evaluate the effect of reduction mammaplasty on the posture of women with macromastia.
Methods
A prospective controlled study at a university medical center. Forty-two patients that underwent breast reduction were studied before surgery and an average of 4.3 years following surgery. Thirty-seven healthy women served as controls. Standardized lateral photos were taken. The inclination angle of the back was measured. Regression analysis was performed for the inclination angle.
Results
Preoperatively, the mean inclination angle was 1.61 degrees ventrally; this diminished postoperatively to 0.72 degrees ventrally. This change was not significant (P-value=0.104). In the control group that angle was 0.28 degrees dorsally. Univariate regression analysis revealed that the inclination was dependent on body mass index (BMI) and having symptomatic macromastia; on multiple regression it was only dependent on BMI.
Conclusions
The inclination angle of the back in breast reduction candidates is significantly different from that of controls; however, this difference is small and probably does not account for the symptoms associated with macromastia. Back inclination should not be used as a surrogate "objective" measure for symptomatic macromastia.
INTRODUCTION
Reduction mammaplasty is a common procedure in plastic surgery. The principal reasons for women with macromastia to undergo a breast reduction are back pain (92%), painful bra grooving (94%), neck pain (95%), and shoulder pain (94%) [1]. These physical complaints combined with psychological and social complaints can lower the patients' quality of life [2,3].
Reduction mammaplasty has an overall high patient satisfaction rate [3]. It is effective in alleviating the symptoms associated with macromastia [4], and the improvement in quality of life and self-esteem is well documented [1,5-9]. Patients have overwhelming physical and psychological benefits from surgery [1,3,7]. Bra grooving and back, neck, and shoulder pain significantly decrease or totally disappear after reduction mammaplasty [5,10,11]. However, all the above-mentioned findings are based on data of the subjective perceptions of the patients. Although valuable, such research does not provide a causal explanation for the beneficial effects of reduction mammaplasty.
Foreman et al. [12] measured a 35% reduction in average maximum low-back compressive forces during a lifting task after reduction mammaplasty. Findikcioglu et al. [13] revealed that both the thoracic kyphosis and the lumbar lordosis angle were higher in women with bra size D than in women with bra size A, B, or C. Letterman and Schurter [14] noted that the center of gravity changes in women with macromastia, and results in increased cervical lordosis. Tenna et al. [15] were the first to investigate the effect of breast reduction on posture and described an improvement using static stabilometry. Except for the above mentioned studies, little is known about the influence of macromastia on posture and whether altered posture is responsible for the pain symptoms seen in patients seeking breast reduction for symptomatic macromastia.
Posture may be objectively quantified by measuring the inclination angle of the back, which is the sum of kyphosis and lordosis. It has been hypothesized that women with macromastia adopt a corrective posture due to the effect of the breasts on their center of gravity and possibly in a subconscious effort to conceal their breasts [14].
The aim of this study was to assess whether patients with macromastia have a different back angulation than patients without macromastia and to determine the effect of breast reduction surgery on back angulation.
METHODS
This study was approved by the institutional medical ethics committee, and the tenets to the ethical guidelines of the 1975 Declaration of Helsinki were adhered to. Informed consent was obtained from the participants.
The study used a prospective study design, with patients serving as their own controls. Normal subjects served as controls for the patient group at baseline.
The setting was a university medical center. Patients who underwent bilateral reduction mammaplasty for symptomatic macromastia with complaints including back pain, neck pain, shoulder pain, or painful bra grooving were eligible for inclusion in the study. Exclusion criteria were musculoskeletal diseases such as rheumatism, spinal disk herniation, or ankylosing spondylitis. Patients that previously had undergone back surgery were also excluded. In the end, 42 patients were included in the study group, while 37 female patients without complaints of back pain served as controls.
The weight, height, and cup size of the patients in the reduction group (preoperative and postoperative) and the women in the control group were measured, and the body mass index (BMI) in kg/m2 was calculated.
Visual analogue scale (VAS) scores for back pain were documented, ranging from "0" indicating no pain to "10" as the worst possible pain. These were recorded preoperatively and postoperatively.
Standardized lateral pictures of the patients were taken with a Nikon D200 and 60 mm lens. The patients stood without a bra, with a standard grid used as a background and the camera at the level between T1 and L5 at a distance of 2.5 m from the patient. Two hemispheric markers were attached to the patient's body: one on the first thoracic vertebra and the other on the fifth lumbar vertebra. The diameter of the markers was 5 centimeters, with a red dot in the middle. In order to achieve maximal relaxation, the patients were asked to stand relaxed; in addition, they were distracted with a mental task in order to reduce their focus on their posture. A sequence of ten pictures was taken in each session at random intervals in order to exclude measurement artifacts as a result of the natural postural sway of the subjects. This sequence was repeated at least one year after reduction mammaplasty.
The coordinates of the markers were assessed using Adobe Photoshop Elements 2.0 (Adobe, San Jose, CA, USA). The mean (M) and standard deviation of the different markers of the ten pictures were used for the analysis.
The angle between the back inclination T1-L5 and the vertical gridlines was calculated as angle α (Fig. 1).
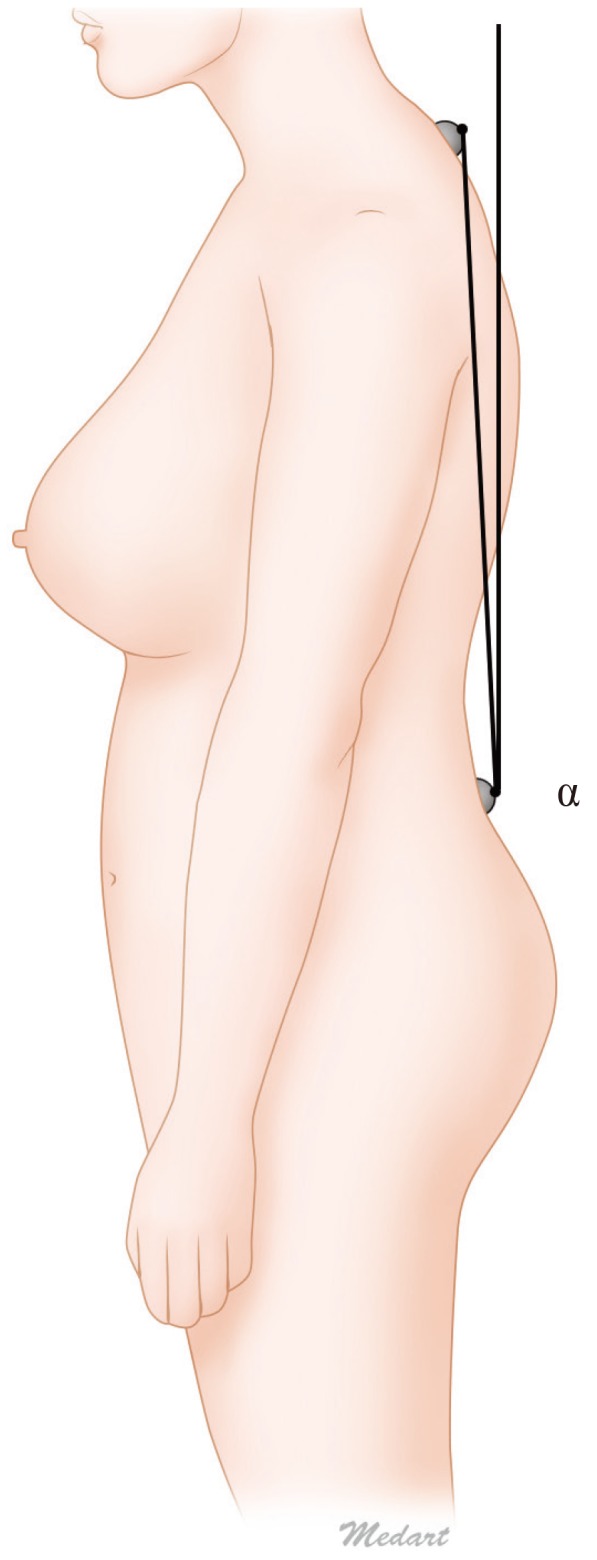
Experimental setup
The inclination angle of the back α was calculated as the angle between the line T1-L5 and a vertical line.
We compared the preoperative and postoperative inclination angle using the paired T-test. The preoperative inclination was compared to the postoperative inclination, and to the control group using the unpaired T-test.
To evaluate determinants for the inclination angle, we performed regression analyses with the inclination angle as the dependent variable, and BMI, cup size, and being a patient or a control as the predictors. The BMI scores were categorized into an overweight group and a non-overweight group, with a BMI ≥25 being considered overweight. Cup sizes were divided into two categories: cup sizes D or larger were considered hypertrophied and smaller cup sizes, non-hypertrophied. SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses.
RESULTS
Forty-two patients were included in the study group. At the time of inclusion, their mean age was 35.6±11.7 and their mean BMI was 26.0±2.7. The total weight of the removed breast tissue ranged from 312 to 2,155 g, with an average of 1,111±470 g. The preoperative reported cup size ranged from D to HH. Postoperative follow-up took place for 4.3±2.3 years.
The control group included 37 women with a mean age of 34±14.4. The mean BMI was 23.3±2.9, and the cup size of this group ranged from A to G.
The mean preoperative inclination angle in the reduction group was 1.61±3.66 degrees ventrally. After surgery, this angle decreased to 0.72±3.48 ventrally. The mean inclination angle of the control group was 0.28±4.18 dorsally. The average postoperative change of the inclination angle was 0.89±3.48 degrees towards the inclination angle of the control group (Fig. 2).
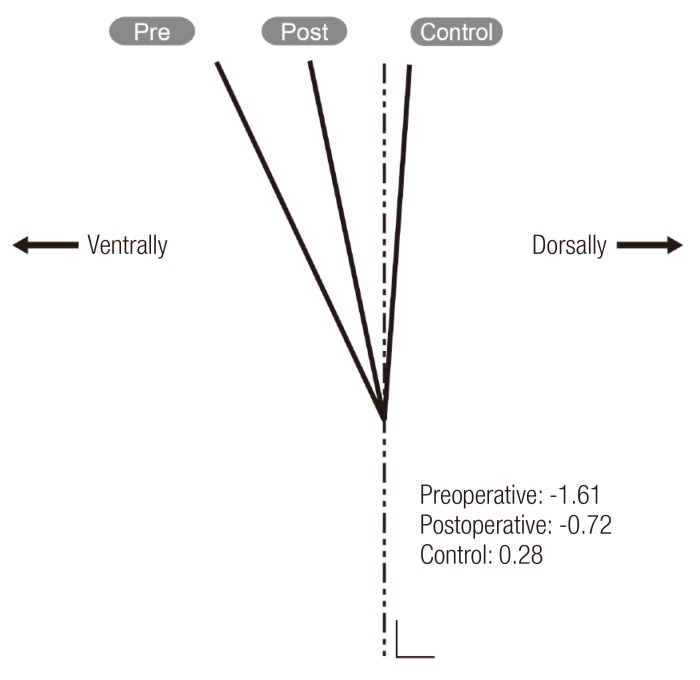
Measured back inclination
Schematic representation of the inclination angles in patients and controls. The dotted line represents a vertical line. The control patients had a dorsal inclination; the patients who underwent surgery had a ventral angulation that showed normalization following surgery. pre, preoperative; post, postoperative.
The paired T-test result of the preoperative and postoperative inclination was 0.104 and therefore not significant. The unpaired T-test of the preoperative inclination and that of the control group was 0.035, which was significant. The unpaired T-test of the postoperative and the control group inclination was 0.249. In the control group a sub-analysis was performed to test if the inclination angle in the women with larger breasts differed from that of the women with smaller breasts. The women were divided into two groups based on their reported cup size. The nonhypertrophied group included 21 women with cup size A to C, and they were found to have a dorsal inclination of 0.32±4.42 degrees, while the hypertrophied group of 16 women with cup sizes D to G had a dorsal inclination of 0.23±3.98 degrees. The difference in inclination angle between the large-breasted and small-breasted controls was not significant (P=0.949).
Before reduction, 30 out of 42 patients had a VAS score for back pain higher than 3. Postreduction, only 8 out of 42 patients had a VAS score higher than 3.
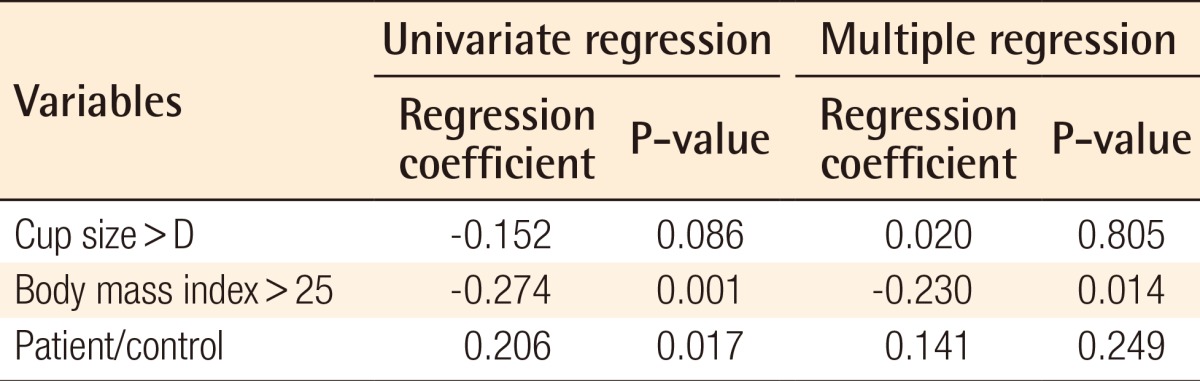
The data was further analyzed using linear regression for inclination. On univariate analysis, BMI and being a patient or a control were significant predictors, while on multiple regression it was found that only BMI was a significant predictor (Table 1).
DISCUSSION
The aim of this study was to determine whether the back inclination is different in patients with symptomatic macromastia than that of asymptomatic women, and if so, whether it normalizes following reduction mammaplasty. Such a change could explain the improvement in pain symptoms following reduction mammaplasty reported in the literature and observed in our study.
We found a small but significant difference in back inclination between symptomatic patients with macromastia, who had a ventral angulation, and controls, who had a dorsal angulation. There was normalization in back angulation following surgery; however, this change was not significant. In the regression analysis, back inclination was found to be dependent on the BMI and not the cup size or having requested breast reduction.
We cannot conclude that the difference in posture between the patients with macromastia and the controls was the result of the breast size. We assume that the small change in posture does not explain the pain in patients with symptomatic macromastia seeking breast reduction surgery or the subsequent reported alleviation of pain after the surgery.
Collins et al. [5] stated that unlike reduction mammaplasty, conservative measures such as weight loss, medications, physical therapy, and special brassieres did not provide effective permanent relief of symptoms. Spector and Karp [16] quantified a significant improvement in back complaints after reduction of less than a total of 1,000 g of breast tissue, and concluded that even small reductions are effective curative procedures for the burdensome condition of macromastia. No physiological explanation has so far been found for this improvement after such small reductions in load. Nevertheless, in a study investigating whether fatigue occurs in trunk extensor muscles during low level activity, Electromyography (EMG) testing indicated that sustained mean activity levels as low as 2% EMG max may lead to fatigue [17]. This fatigue could ultimately result in discomfort and pain. The sustained extra load on the back muscles of women with macromastia may well be in the range of 2% EMG max, especially in a ventrally angulated back, and as such, induce back pain [14].
Additionally, Tenna et al. [15] demonstrated a decrease in the effort required to maintain a stable posture following breast reduction using static stabilometry, and this reduction in muscle activity may also explain the reduction in back pain following surgery.
Findikcioglu et al. [13] revealed that both thoracic kyphosis and lumbar lordosis were greater in women with macromastia. The small inclination angles we observed may be a combination of a large lordosis angle countered by a large kyphosis angle. Findikcioglu et al. [13] examined the vertebral column only preoperatively, and thus could not observe if there was a change. Our study has the advantage that we also performed postoperative measurements to account for the effects of surgery. Further studies should focus on the effect of surgery specifically on the lordosis and kyphosis curves.
The experimental set-up and the comparison with a control population that includes a group of women with cup size D or more without functional complaints and not seeking surgical care ensured an objective comparison of posture. However, a possible weakness in our study is the difference in BMI and the discrepancy in cup size between the patients and the control group. The average BMI and the average cup size were lower in the control group. This however reflects the clinical situation that macromastia is often correlated with a higher BMI; thin patients with large breasts are a rather the exception than the rule [18].
Based on our results, we conclude that, in women with symptomatic macromastia seeking reduction mammaplasty for relief of their physical complaints, the difference in the back inclination angle compared to the control is too small to account for the development of back pain and should not be used as an "objective" surrogate measure for back pain. The improvement in inclination seen following surgery is not significant and cannot explain the relief of the symptoms. Back inclination angles should not be used as a measure for back pain and resource allocation in patients seeking breast reduction.
Notes
No potential conflict of interest relevant to this article was reported.