Recurrent Auricular Keloids during Pregnancy
Article information
A keloid is one of the most frustrating clinical problems in wound healing. Keloids form following dermal injury and exhibit exuberant and indefinite growth of collagen. Many theories have been propounded in trying to explain some of the vagaries of keloids. From one of the theories, keloid scars may develop at any age; patients between 10 and 30 years of age (reproductive age) are the most affected population, and there may be a hormonal influence because keloid scars tend to grow during puberty and pregnancy, and resolve during menopause [1]. In our experience, pregnancy-related recurrent keloids have arisen from the ear, despite the patient's successful completion of our treatment. The case presented here illustrates the possible connection between keloid formation and hormonal changes during pregnancy.
A 27-year-old pregnant female visited our clinic due to progressive growth of her left auricular keloid. Three years prior to the visit, she had developed a scar on her left auricle after treatment for acute inflammation caused by an ear piercing procedure at a non-medical institute. She showed no other particular medical history. She also reported that the lesions appeared and became larger after the first trimester of pregnancy (Fig. 1). On physical examination, the left auricle showed a keloid of nearly circular appearance, approximately 2.2 cm in diameter, with a mean thickness of about 1.5 cm, extending from the superior pole of the auricle down to the middle ear. The skin surface of the keloid was irregular and showed dispersed minute superficial ulcer with itching sensation.
Because of pregnancy, we waited to perform a core extirpation of the keloid until 6 months after delivery. Compression on the auricle was performed postoperatively in combination with the application of scar care ointment. Even after 1 month, the clinical result remained obviously acceptable where the core extirpation had been performed.
Two years later, the patient returned with a huge enlargement of the left auricular keloid. Similar to the previous keloid, it appeared and became bigger (2.2×1.7 cm) simultaneously with child bearing. She remembered that the keloid started to enlarge rapidly in her first trimester of her second pregnancy, with mild itching and redness. She was asked to return after her delivery (Fig. 2).
Accordingly, she underwent core extirpation 6 months after her second delivery, and compression treatment was performed postoperatively in combination with the application of scar care ointment. The patient was satisfied with the results at postoperative 4 months.
The scar tissues, sized at 2.0×1.5 cm and 2.0×1.0 cm, were excised over repeated core extirpations. In both histopathologic reports, no flattening of the overlying epidermis, presence of keloidal collagen, or a prominent fascia-like fibrous band occurred, which confirms the diagnosis of keloid (Fig. 3).
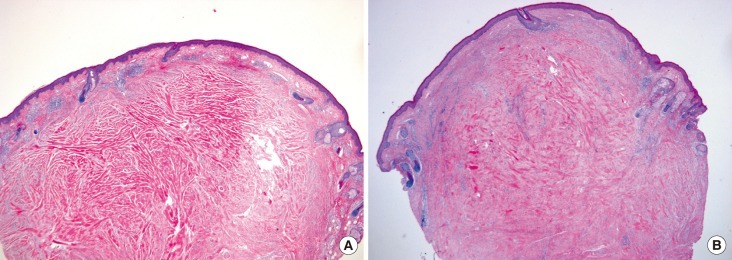
(A) First pregnancy. Histopathologic photograph showing thepresence of keloidal collagen and a prominent fascia-like fibrous band, which confirms the diagnosis of keloid (H&E, ×100). (B) Second pregnancy. Histopathologic photograph showing nearly the same appearanceof keloidal collagen and a prominent fascia-like fibrous band,as in the first pregnancy (H&E, ×100).
Up to the present, the clinical outcome has shown a clean and satisfactory auricle. The patient has not undergone another pregnancy nor presented any additional keloid growth; specifically, she has reported that her lobular keloid remains inactive.
In most known series of keloids, there is a higher incidence in women, with an apparent peak in the immediate post-pubertal years. Lane et al. [2] reported in his study that those who had ear piercings at 11 years of age or above were more likely to develop keloids (80%) than were those who had ear piercings under 11 years of age (23.5%). Because of this observation, the possibility of a female hormonal influence on keloid formation has been advanced.
In a study of connective tissue tumors, Geschichter and Lewis [3], bioassayed a single keloid of an ear that had been preserved in formalin; they reported that this keloid tissue contained large amounts of estrogen and gonadotropic substances. However, no confirmation of their work has appeared in the literature. Jacobsson [4] reported a case of a woman whose 4-year-old scar became hypertrophic during pregnancy.
Reviewing the different actions of pregnancy hormones, it appears that estrogens are the hormones most likely involved in the keloidal tendency that may accompany pregnancy [5]. The ovaries and adrenal cortex of mature women produce estrogens. In pregnancy, the major site of production is the placenta. Our patient noted rapid enlargement and irritation of her keloid, which began in the first trimester of pregnancy. This supports our view on the effect of hormonal influence in scar or keloidal tissue during pregnancy, and agrees with the concept that regression of symptoms occurs after delivery.
It is known that auricular and lobular keloids appear on account of inflammation caused by an unhygienic ear piercing procedure. However, we report our treatment experience in a case with recurrent keloids during pregnancy after showing no particular change at the time of treating the inflammation. We conclude that pregnancy is the strongest risk factor for keloid recurrence in addition to the three clinical risk factors identified through a review of the literature: treatment history, timing of keloid growth, and timing of regression.
Notes
No potential conflict of interest relevant to this article was reported.

