Paraffinoma of the Knee 60 Years after Primary Injection
Article information
A 63-year-old man, unable to walk and a candidate for a knee prosthesis, was referred to u sfor a painful ulcer of the right knee of 12 months' duration. He denied any history of recent trauma or previous surgery. Physical examination revealed a 5.5 cm×4.0 cm ulcer of the medial aspect of the right knee (Fig. 1). An injection of paraffin oil into the knee 60 years before to treat a post-traumatic sequela was the only risk factor recorded during the medical history taking. There were no comorbidities such as diabetes, heart disease, or atherosclerosis. Doppler ultrasonography was performed in the lower extremities, but no peripheral arterial disease was found. The ulcer was painful, with smooth, erythematous, and indurated skin, but without exudates or edema. The bacteriological examination revealed no growth. The patient did not have any symptoms such as fever or lymphocytosis.
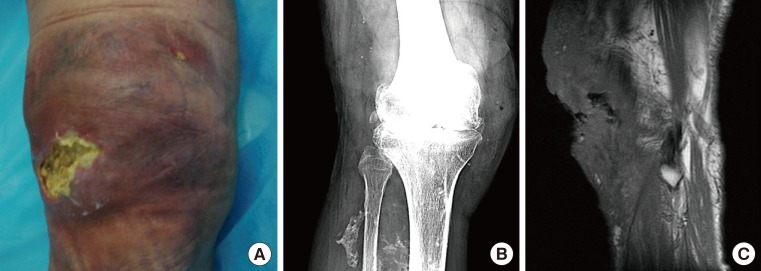
(A) Right knee at the time of admission. A 5.5 cm×4.0 cm ulcer was present, surrounded by smooth, erythematous, and indurated skin. (B) Radiography scan of the right knee. Soft tissue swelling and many dense, rounded, and streaky calcifications. (C) Magnetic resonance image showing infiltration of the soft tissue of the knee by low signal intensity.
Wide surgical debridement was performed. The specimen removed included a large piece of skin overlying the knee joint and the anterior aspect of the lower leg down to the ankle, and the underlying subcutaneous fat and skeletal muscle. Macroscopically, the typical lobulated fatty material mixed with scattered small nodules having a nearly transparent oily cut surface was not observed within the lesion. Histologically, sporadic vacuolated spaces of different sizes were detected within the adipose tissue with surrounding multinucleated giant cells and foamy histiocytes. There was no evidence of any paraffin, which had evidently been completely absorbed and replaced by dense fibrous connective tissue with an "embalmed-like" aspect. We concluded that the paraffin oil had been removed by macrophages during the long intervening period of time. This was confirmed by three sets of data: the histological results suggestive of an oleogranulomatous reaction to foreign material; the radiographic scan (Fig. 1); and the magnetic resonance imaging (MRI) examination showing irregular rounded and streaky calcifications, atypical opacities, fibrosis, and thickening of soft tissue with unusual architectural distortion of the lower limb.
Once the tissue was debrided (Fig. 2), a temporary wound closure at the defect site was achieved by application of vacuum assisted closure therapy. Finally, a right anterolateral thigh free flap with end-to-end anastomosis to the anterior tibial vessels was performed to cover the tibia and a skin graft was placed over the knee (Fig. 2).

(A) Post-debridement view of the right lower limb and (B) at six-month follow-up after free right anterolateral thigh flap reconstruction.
Paraffin oil was frequently used in the past to fill up defects in subcutaneous tissue [1]. This method has been abandoned because of several reports of serious local complications (formation of paraffinoma, inflammatory reactions, tissue necrosis, and sinus tract formation) and systemic complications (pulmonary and cerebral embolism) [2]. Although breast and facial paraffinomas are well-known and recognized complications of augmentation paraffin injections, only three patients, including the present case, have been reported to be affected by knee paraffinoma. In a 27-year-old man, a successful attempt was made to produce swelling and inflammation of a knee-joint to avoid military service. Since then, he has had attacks of painful swelling of the knee about once a year [3]. A 90-year-old man was reported to have a swollen, painful knee and a history of paraffin injections that had been present for more than 3 months [4]. He admitted self-injections of paraffin to his own knee in an attempt to avoid military service during the Second World War and experienced intermittent episodes of suppuration and fistula formation in the following years [4]. Our case is the first non-self-induced knee paraffinoma.
Paraffinomas may present with different features, from a painless mass to a destructive ulcer simulating carcinoma [5]. Dense fibrosis causing streaky opacities and bizarre architectural distortion without erosions are the conventional findings on radiographic scan. Flocculent, amorphous, ring-shaped, or rounded calcifications may also be present within the involved tissues [2,5]. The plaque-like MRI signal intensity is low to intermediate on both T1-weighted and T2-weighted sequences, whereas the signal intensity of the round component is low on both T1-weighted and T2-weighted sequences and is markedly suppressed on the fat-suppression sequence. Our long experience in managing post-paraffin oil complications [1] allowed us to reach diagnoses by detailed medical inquiry, despite the aspecificity of the radiographic investigation and the long time interval between the primary injections and the symptoms. We would like to highlight the limits of diagnosis of paraffinoma affecting an unusual site such as the knee by means of radiological and histological examination without a relevant clinical history. This paper emphasizes the importance of collecting detailed clinical information because paraffinomas may develop in unusual sites even decades after primary injections and paraffin oil may not be found.
Notes
No potential conflict of interest relevant to this article was reported.