Facial Transplantation Surgery
Article information
SUMMARY
It is well known that patients with severe facial injuries accompanied by facial disfiguration are vulnerable to a poor quality of life. With the help of facial transplantation, it has become possible to achieve an optimal anatomical reconstruction. As compared to conventional methods, it can provide more desirable functional, aesthetic, and psychosocial outcomes. Face transplantation surgeons need to consider many problems associated with the criteria for selecting patients, techniques for harvesting the donor tissue, prediction of the expected functional outcomes, limitations in obtaining written informed consent for conducting the procedure, evaluation of the post-transplant immunological response and postoperative immunosuppressant requirements, psychological and social outcomes for the patients, and other concerns about funding and ethical issues.
INTRODUCTION
Over the past few decades, great advancements have been made in the field of facial transplantation as per the experimental and clinical studies on trauma or congenital malformation [1]. Nowadays, vascularized composite tissue allotransplantation is considered another treatment option in patients with complex craniofacial defects. This is because controversy exists regarding whether autologous facial reconstruction is optimal for them. In 2005, facial allograft transplantation was first reported in France. Since then, it has been performed worldwide in a total of 25 patients [2,3,4]. This shows that the functional and aesthetic outcomes of facial transplantation are encouraging. With a dramatic improvement in functional status, patients have a restored ability to make facial expressions such as a smile and to perform various functions such as smelling, eating, drinking, and speaking [5,6]. However, the risks and benefits of facial composite tissue allotransplantation, involving mandatory lifelong immunosuppression similar to that in the case of a renal transplantation, should also be considered by the multidisciplinary team of facial transplantation experts [7,8]. In this article, we have summarized the published clinical studies on all the facial transplantations that have been performed thus far; we have then attempted to provide a basis for further studies on facial transplantation.
PROGRAM AND COST OF FACIAL TRANSPLANTATION
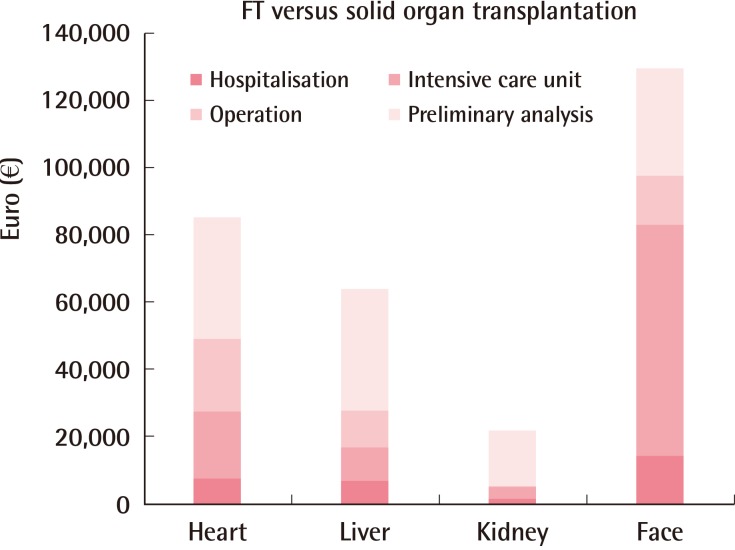
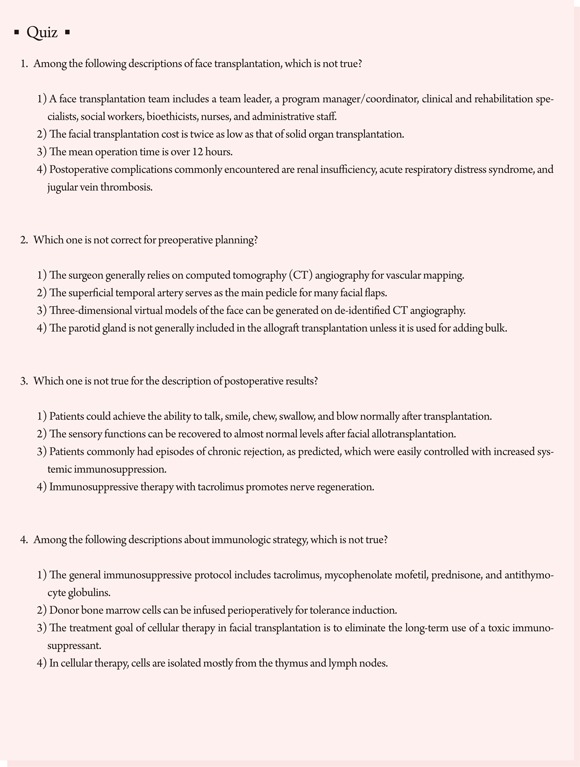
Before the initiation of the facial transplantation program, there was disagreement over its risks and benefits. Robust research protocols, strong infrastructure, specialized personnel, and adequate financial support were considered essential factors for the success of this program [9,10]. To date, only a few active facial transplantation programs have been implemented worldwide; however, there is a growing interest in these programs. Thus, they would be of help for refining highly effective multi-disciplinary protocols for recruiting patients, obtaining their written informed consent, screening them, making a preoperative plan, and performing facial transplantation and long-term postoperative follow-up (Fig. 1) [11]. The members of the facial transplantation team are responsible for being compliant with the protocol; they include a team leader, a program manager/coordinator, clinical and rehabilitation specialists, social workers, bioethicists, nurses, and administrative staff [12,13]. Their experience has demonstrated that patients can achieve optimal care both before and after the facial transplantation through the collaboration, creativity, and unique multidisciplinary approaches of the team members [11,14]. Facial transplantation costs more than the transplantation of other solid organs including the heart. For example, its cost is twice as high as that of a liver transplantation (Fig. 2) [9]. However, there is a possibility that the cost might fall with the experience of the team, which could shorten the period of postoperative intensive care and the overall length of hospital stay. Two specialty areas contribute the most to the high cost of the program: surgery and nursing. These are followed by anesthesia and pharmacy. The cost of a facial transplantation is approximately equal to that of multiple conventional reconstructions [10,11]. The cost for a facial transplantation is considerable, but for candidates of this procedure, it is priceless to be able to alleviate psychological and physiological suffering, to achieve a dramatic functional recovery, and to realize lasting hope for social reintegration. Overall, the early outcomes of the facial transplantation program have been generally accepted as positive. Because of these positive outcomes, and the ongoing refinement of the process, facial transplantation has eventually become a first-line treatment option in the reconstruction of patients with extensive facial disfiguration [14,15].
Stages of face transplantation. The elapsed time from patient referral to placement on transplant waitlist may be 3 to 11 months. Time spent on the transplant waitlist is unpredictable. Postoperative follow-up will continue until allograft failure or the patient's death (From Bueno et al. J Plast Reconstr Aesthet Surg 2011;64:1572-9, with permission from Elsevier [11]).
ANESTHESIA
In the facial transplantation procedure, patients are anaesthetized; this requires the surgeons to plan in advance for airway management, vascular access, anesthetic technique, and fluid management [16]. The preparation and grafting phases are highly hemorrhagic (>one blood volume), for which a massive blood transfusion may be required. Despite the actual methods and technology for hemostasis, there may be limitations in the management of intraoperative bleeding. Moreover, the anesthesiologist should prepare for long anesthesia during the facial allograft transplantation in patients with rapid blood loss after the reperfusion of the graft. Furthermore, hemostasis monitors may be required for urgently assisting the clinicians in making a correct, prompt diagnosis. The mean operation time is 19.1 hours (range, 15-28 hours). Most of the patients in this series present with severe graft edema after surgery. They also encounter complications at the intensive-care-unit stage; these include renal insufficiency, acute respiratory distress syndrome, and jugular vein thrombosis. In addition, they are immunocompromised and then are vulnerable to opportunistic bacterial infections during the postoperative period. Therefore, the anesthesiologist should have detailed access to the medical history of the donor in the early planning phase, thus suggesting alternative anticoagulation for both the donor and the recipient in order to prevent the occurrence of possible complications [16,17].
SURGERY PLAN
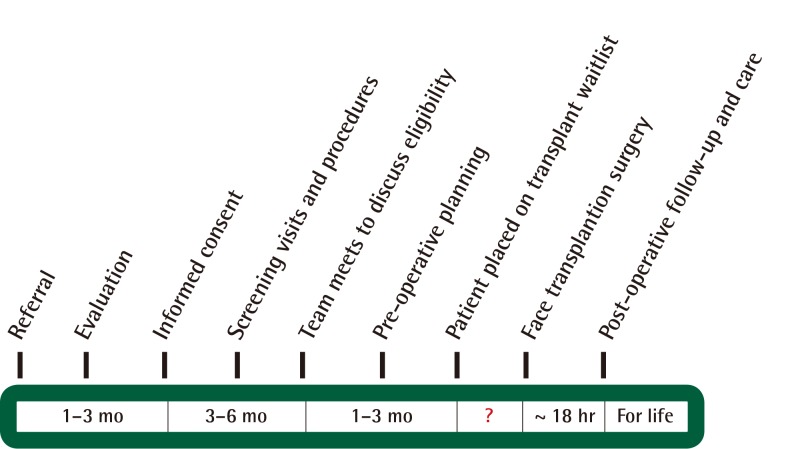
In making a treatment plan for the facial transplantation, surgeons should consider the craniofacial and orthognathic factors, including both bone and soft tissue, for the purposes of restoring the normal anatomy by achieving an optimal relationship between the face and the skull base. In routine orthognathic planning based on cephalometric parameters, patients can achieve a restoration of most of the anatomical structures and thereby recover their occlusion, speech, and airway functions [18]. Candidates are typically characterized by the extremely complex vascular anatomy arising from severe injury or multiple previous reconstructive attempts. This explains why each procedure is rigorously determined on the basis of their defects and vascular anatomy. With vascular mapping on computed tomography (CT) angiography, surgeons should evaluate the clinical relevance of the images, the concept of angiosome, the non-invasive delineation of major vessels, and current controversial issues associated with vascular anastomosis. The facial artery is mainly distributed in the facial skin envelope, thus serving as the main pedicle for many facial flaps, including those for facial transplantation. The predominant distribution of the facial artery in the facial region is commonly seen but cannot be predicted. Therefore, it is mandatory to carefully perform a vascular work-up prior to the facial transplantation and unipedicled flap procedure [19]. For the facial transplantation procedure, three-dimensional virtual models of the face are generated on de-identified CT angiography. They are used as the donor and the recipient for the virtual facial transplantation. The facial allografts harvested from the donor model are dissected in a cranio-caudal and a lateral-to-medial manner. In addition, the facial nerve branches are dissected medially to the parotid gland and then attached to the recipient ones. The parotid gland is not generally included in the allograft transplantation unless it is used to add bulk. In the recipient model, specific facial defects (e.g., mandibular, midfacial, or large ones) are created using surgical planning software [20,21]. Then, they are restored with allografts harvested from the donor model (Fig. 3) [22].
(A) Schematic outline of the donor operating room. A, Facial mask molding; B, Facial graft procurement; C, Donor defect coverage. (B) Guidelines of sequences of donor operation for face allograft procurement (C) Schematic outline of the recipient operating room. A, Recipient defect before the input; B, Recipient defect after removal of scar tissue and hardware; C, Inset of donor facial graft (From Siemionow and Ozturk. J Reconstr Microsurg 2012;28:35-42, with permission from Lippincott Williams [22]).
POSTOPERATIVE RESULTS
The initial experience demonstrated that the facial transplantation is a feasible surgical modality. It is indicated for patients with gunshot injuries who had previously undergone multiple conventional surgical reconstructive procedures but failed to obtain favorable treatment outcomes. It has been reported that the functional and aesthetic outcomes were very encouraging with good motor and sensory recovery after transplantation. The types of allografts varied according to the anatomical components forming the face as well as the amount of skin, muscle, bone, and other tissues. Patients achieved a recovery of phonation to such an extent as to talk normally. They could smile, chew, swallow, and blow normally but still had difficulty in pouting and kissing. Patients commonly had episodes of acute rejection, as predicted, which were easily controlled with increased systemic immunosuppression [23,24]. Patients also achieved dramatic recovery of psychological functioning to such an extent as to be reintegrated into society. All the candidates were fully informed of the risks of developing cytomegalovirus infection, and they submitted written informed consent for aggressive prophylaxis for viral, bacterial, or fungal infections [25,26]. There were some long-term complications, as similarly seen in patients undergoing solid organ transplantation. However, the patients were satisfied with their new facial appearance and could be reintegrated into society. In facial transplantation, it is important to identify healthy nerves for neurotization, which is essential for successful nerve regeneration within the allograft. However, depending on the severity of the initial injury and the resulting scar formation, it is commonly found that healthy nerve stumps are missing in the recipient. Nevertheless, sensory functions can be recovered to almost normal levels after facial allotransplantation without repairing the sensory nerve [27]. This is based on the mechanisms arising from the preservation of the normal density of the receptors within the facial allograft, the nerve regeneration from the recipient bed and allograft margins, the transmission of the sensory signals via the afferent fibers forming the facial nerve, the nervi nervorum of the facial nerve or trigeminofacial communicating rami. Furthermore, it is noteworthy that immunosuppressive therapy with tacrolimus promotes nerve regeneration [28].
IMMUNOLOGICAL STRATEGY
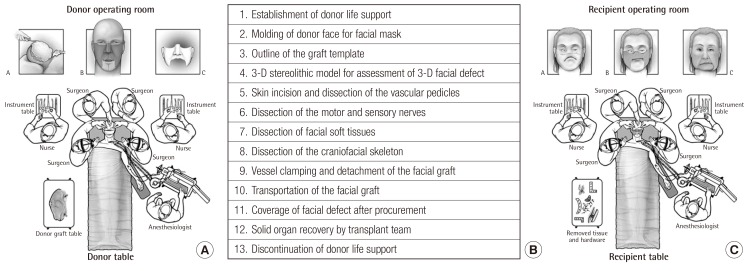
Most of the patients undergoing facial transplantation presented with a few episodes of acute rejection during the first year. In these patients, the immunosuppressive protocol included tacrolimus, mycophenolate mofetil, prednisone, and antithymocyte globulins [29]. In addition, they were infused with donor bone marrow cells perioperatively. They presented with major adverse effects such as progressive renal dysfunction, but achieved an improvement of symptoms after switching from tacrolimus to sirolimus. The treatment goal of cellular therapy in facial transplantation is to continuously develop new strategies that will eliminate the use of toxic immunosuppressive protocols [30,31]. It is useful in prolonging allograft survival and shortening the healing time to a significant extent. In cellular therapy, cells are isolated mostly from the bone marrow and the adipose tissues [32,33]. They can proliferate and differentiate in the transplanted tissue, thus having an immunomodulatory effect (Fig. 4) [32]. Several experimental studies examining the usefulness of cellular therapies using T-regulatory, dendritic, and chimeric cells are in progress [34]. However, thus far, no studies have established the molecular characteristics of these cells and the mechanisms by which they are involved in the acceptance and rejection of allografts. This deserves further study contributing to the future of modern transplantology.
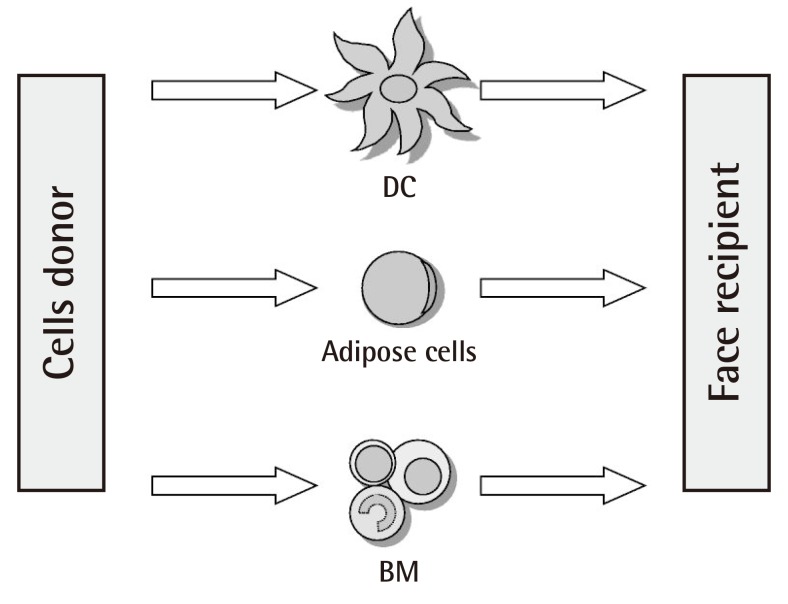
The variety of cells serving as therapeutic populations in face transplant recipient. Bone marrow (BM) cells, adipose cells, and dendritic cells (DCs) are easily accessible and harvestable from the donor and could potentially function as a supportive therapy to prolong face transplant survival without the need for immunosuppression. The possibility of their in vitro multiplication, cryopreservation, and modification through molecular biology tools make them a universal approach. It is hoped that their use in clinical settings will be possible in the future (From Siemionow et al. Ann Plast Surg 2012;69:575-9, with permission from Lippincott Williams [32]).
FUTURE OF FACIAL TRANSPLANTATION
As described in this paper, facial transplantation is effective in restoring the facial appearance and functions of patients with severe facial defects. Thus, it has been considered to be the most comprehensive transplant that has been performed to date. In the field of facial transplantation, ongoing efforts are being made to restore the facial appearance and functions in patients with severe facial disfiguration through a systematic approach and an adherence to the principles of aesthetic surgery, craniofacial surgery, microsurgery, and other innovative surgical techniques [35,36]. Comprehensive, multidisciplinary approaches are essential for effectively addressing this innovative surgical strategy. This includes an infrastructure of basic science, a supportive clinical background, innovative technologies, model simulations of cadaveric studies, real-time clinical rehearsals, and voluntary participation of patients who have submitted written informed consent. At present, only a limited number of patients have undergone facial transplantation not only because there are no established studies on the transplant's long-term outcomes but also because patients need to undergo lifelong immunosuppression and receive revision reconstructive surgery in case of treatment failure [37]. Based on the initial experience, the indications for facial transplantation have been expanded to full facial defects. Moreover, other indications have been considered in a patient-specific manner. Patients are fully informed of the risks and benefits of the facial transplantation, thus being involved in the decision-making process, on the condition that there are no absolute exclusion criteria [38]. Although infrequently, facial transplantation is also performed in combination with composite tissue allotransplantation, combining various types of tissues harvested from the face (e.g., myocutaneous vs. osteomyocutaneous) and the upper extremity, in a clinical setting [39]. Further studies are warranted for examining the long-term outcomes of facial transplantation with a safe reduction of immunosuppression. This will eventually contribute to expanding the indications for facial transplantation from major unreconstructable defects to potentially minor ones. Thus, it is also called block surgery [40].
Notes
This work was supported by the general research supporting program of National Research Foundation of Korea (08-2013-032).
No potential conflict of interest relevant to this article was reported.