Tracheal Laceration Related to Endotracheal Intubation
Article information
Tracheal laceration is a complication of general endotracheal anesthesia. Tracheal laceration during intubation is uncommon but fatal, and is difficult to recognize. Therefore, we have to pay considerable attention to the symptoms of tracheal laceration. We report a case of tracheal laceration after a simple plastic surgery operation.
A 44-year-old woman (height, 151 cm; weight, 55 kg) who had a nasal bone fracture was scheduled to undergo a closed reduction under general endotracheal anesthesia. She had no underlying disease.
However, 48 hours after the operation, she had dyspnea along with subcutaneous emphysema on her shoulder (Fig. 1). Diagnostic bronchoscopy revealed an approximately 1.5-cm-sized vertical tracheal laceration above the carina with split thickness (Fig. 2). She was started on antibiotics, O2 inhalation, expectorants and non-per oral. The emphysema spontaneously resolved. The patient was discharged uneventfully on postoperative day 7.
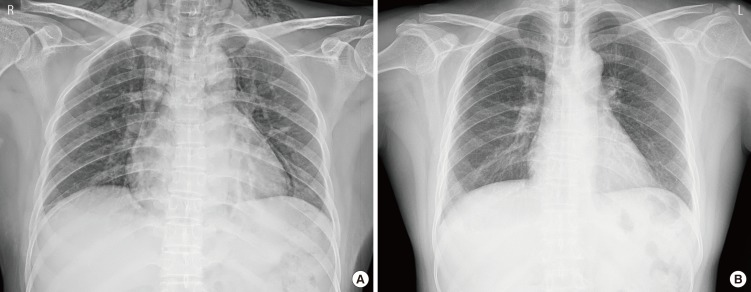
(A) Chest X-ray 1 day after admission. Subcutaneous emphysema can be observed on both shoulders. (B) Chest X-ray 2 days after admission. The previous subcutaneous emphysema has disappeared.
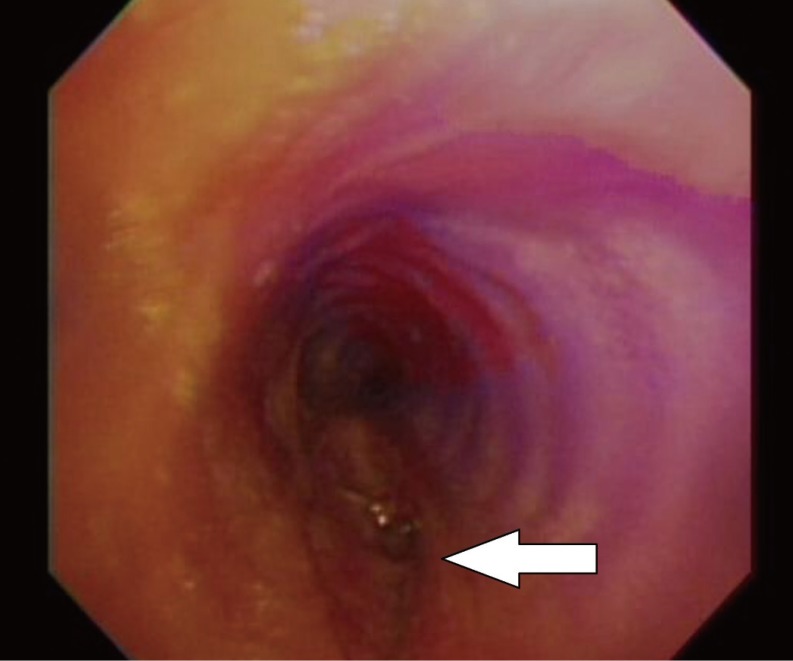
Diagnostic bronchoscopy. A lacerated wound (white arrow) can be observed above the carina. It is approximately 1.5 cm vertically and has split thickness.
Many operations in plastic surgery are simple and quick. However, general endotracheal intubation may be required for various reasons. Therefore, it is important for a plastic surgeon operating on the face to be familiar with the complications of intubation.
The incidence of postintubation tracheal laceration is reported to be approximately 1/20,000 [1]. Thus far, the cause of this laceration has not been definitely established, but the condition is generally attributed to pre-existing tracheal wall weakness, difficult intubation, emergency intubation, inexperience of the health professional, a double-lumen tube, and movement of the head and neck while the patient is intubated [2,3]. A higher incidence is observed in patients who have a chronic use of steroids, are of advanced age, are female [4] and/or have other inflammatory lesions of the trachea.
The common symptoms of postintubation tracheal laceration are chest discomfort, dyspnea, dysphonia, cough, hemoptysis, mediastinal emphysema, subcutaneous emphysema, and pneumothorax. The tracheal laceration is detected early when the laceration is large and deep. In these cases, it is usually detected intraoperatively. However, smaller tears are detected during the postoperative period.
The exact site and size of the abovementioned laceration is determined by bronchoscopy; this knowledge helps in planning the therapeutic approach.
Nonoperative indications are stable vital signs, no difficulty ventilating while intubated or respiratory distress while extubated, no evidence of esophageal injury, minimal mediastinal fluid collection, nonprogressive pneumomediastinum or subcutaneous emphysema, and no signs of sepsis [5].
In our case, the tracheal laceration could have arisen after elective operation or uncomplicated intubation, as the patient had no underlying diseases. Her risk factors were only the head and neck surgery and her gender. These risk factors are common in patients who undergo operations in plastic surgery. We assume two possible causes in this case. First, potadine and bleeding could have irritated the trachea and triggered a cough and gag reflex. Secondly, repeated sterilization for reuse may have increased the stiffness of the intubation tube.
A plastic surgeon must be familiar with the causes and the symptoms of tracheal laceration. In particular, such a laceration could have occurred during a short operation such as a closed reduction of the nasal bone. For the prevention of tracheal laceration, we need to determine a patient's underlying disease. Further, plenty of irrigation is required for the removal of the potadine and blood before extubation.
Notes
No potential conflict of interest relevant to this article was reported.