Aesthetic Design of Skin-Sparing Mastectomy Incisions for Immediate Autologous Tissue Breast Reconstruction in Asian Women
Article information
Abstract
Background
The advent of skin-sparing mastectomy has allowed for the reconstruction of the breast and nipple with improved cosmesis. However, the nipple-areolar complex (NAC) in Asian patients is more pigmented and scars easily. Therefore, commonly described incisions tend to result in poor aesthetic outcomes in Asian patients with breast cancer.
Methods
We describe an algorithmic approach to skin-sparing mastectomy incisions in Asian patients on the basis of the location of the biopsy scar and the tumor site and size. Four incision types are described: peri-areolar, a peri-areolar incision with a second distant skin paddle, "racquet handle," and peri-areolar with adjacent skin excision.
Results
281 immediate breast reconstructions were performed between May 2001 and February 2012 after skin-sparing mastectomy. The mastectomy incisions used included the peri-areolar design (n=124, 44%), peri-areolar design with a second distant skin paddle (n=39, 14%), "racquet handle" (n=21, 7.5%), and peri-areolar design with adjacent skin excision (n=42, 14%). The traditional elliptical incision and other variants where the NAC outline was not preserved were performed in the remaining 55 patients. The average follow-up was 44.7 months during which there was 1 case of total flap loss and 7 cases of partial flap necrosis; all remaining flaps survived. 24% of the patients (68/281) underwent subsequent nipple reconstruction.
Conclusions
Our algorithm avoids breast incisions that are randomly placed or excessively long and prevents the unnecessary sacrifice of normal breast skin. This allows skin-sparing mastectomy and immediate breast reconstruction to be performed with a consistently achievable aesthetic result in Asian women without neglecting oncological safety.
INTRODUCTION
The advent of skin-sparing mastectomy with immediate breast reconstruction in recent years [1,2,3,4] has resulted in a greater appreciation for the importance of planning mastectomy incisions preoperatively. In turn, reproducible aesthetic results can be achieved after surgery for tumor extirpation. Ideally, all mastectomies should be performed through a peri-areolar incision following the dimensions of the original areola [5] in order to avoid visible scars on the breast mound following subsequent breast and nipple reconstruction. However, this approach cannot be used in the setting of an unfavorably located biopsy scar or when the diameter of the areola is too small [6].
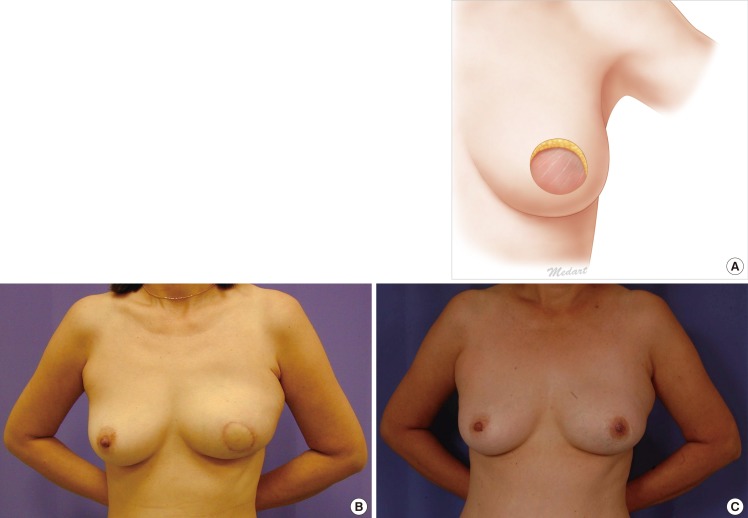
Other incisions that have been described include an elliptical design for increased access [7] and modified Wise or inverted-T incisions for larger breasts [1,8,9]. However, these incisions are less amenable to a favorable cosmetic outcome in Asian women, who generally have less voluminous breasts than their Western counterparts because there is a large area of donor skin in proportion to the reconstructed breast following autologous tissue transfer. The resultant "circle-within-a-circle" effect after nipple reconstruction at a later stage is also particularly noticeable (Fig. 1). Hence, we have been advocating the peri-areolar approach for the majority of our breast cancer patients.

Breast reconstruction after mastectomy with an elliptical incision
Breast reconstruction following mastectomy performed with a traditional elliptical incision in Asian women has a poor aesthetic result due to the vivid contrast between the highly pigmented nipple and the paler skin overlying the transverse rectus abdominis myocutaneous flap reconstruction as seen in this middle-aged woman. Particularly evident is the "circle-within-a-circle" effect due to the large area of flap skin after nipple reconstruction.
In this article, we present our institution's experience with immediate breast reconstruction following skin-sparing mastectomy in Asian women and an algorithm to aid with the decision-making process for the preoperative planning of incision placement on the basis of the site of the biopsy scar.
METHODS
Study group
The records of 281 consecutive patients who underwent immediate autologous tissue breast reconstruction by the senior surgeon (B.K.T.) between May 2001 and February 2012 following skin-sparing mastectomy for both invasive and in situ breast cancer were reviewed. Reconstructions following nipple-sparing mastectomy and implant-based methods constitute a separate series and are not included in this study.
Every case was discussed preoperatively with the resection surgeon to ensure adequate surgical exposure while preserving the maximal extent of the skin envelope in order to optimize the final aesthetic outcome. The mean age at surgery was 46.5 years (range, 23-71 years). Majority of the patients underwent autologous tissue reconstruction with either a latissimus dorsi (LD) flap (±implant) or a transverse rectus abdominis myocutaneous (TRAM) flap (pedicled, muscle-sparing free). The other flaps used were the deep inferior epigastric perforator (DIEP), superficial inferior epigastric artery (SIEA), and the vertical rectus abdominis myocutaneous (VRAM) flap. Following breast reconstruction, all patients were offered nipple reconstruction.
Algorithm for the design of incisions
A peri-areolar incision is designed initially for all patients. Further extension of the incision is planned based on the distance of the biopsy scar from the nipple-areolar complex (NAC) and its size with the aim of preserving at least a part of the NAC outline. Four types of incisions are described:
1) The first group of patients with a biopsy scar within the NAC or in the peri-areolar region will benefit most from a peri-areolar incision where the mastectomy scar can be concealed within the boundary of the native breast skin and the subsequently reconstructed NAC (Fig. 2). A separate axillary incision to facilitate axillary dissection and microanastomosis in the setting of autologous reconstruction with a free flap is made if required intraoperatively.
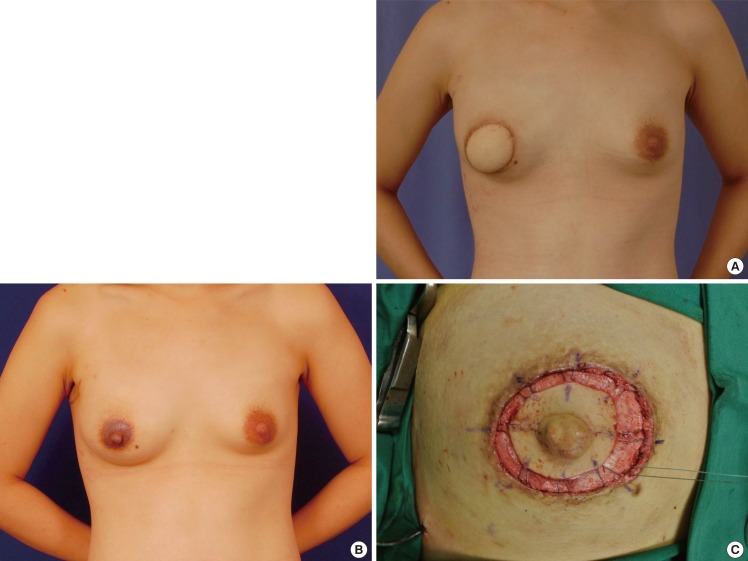
Breast reconstruction after mastectomy with the peri-areolar incision
An optimal aesthetic result is achieved by muscle-sparing free transverse rectus abdominis myocutaneous (ms-TRAM) flap reconstruction following skin-sparing mastectomy through a peri-areolar incision: (A) prereconstruction schematic, (B) postoperative view, and (C) following nipple reconstruction. The scar, which would otherwise be hyperpigmented and prominent, is hidden in the boundary of the reconstructed nipple-areolar complex (NAC). NAC reconstruction using our technique results in a pigmented area of skin, which closely resembles that of the contralateral NAC.
2) The second group of patients with a biopsy scar of more than the distance of one-areola-diameter from the NAC should have the scar excised through a separate elliptical incision. A second skin paddle can be used, if necessary, during autologous tissue reconstruction and serves to prevent skin distortion and pulling on the NAC, which may occur during tight primary closure (Fig. 3) by the preservation of the volume of the breast envelope; direct closure of the biopsy site should only be performed in women with bigger breasts and loose skin.
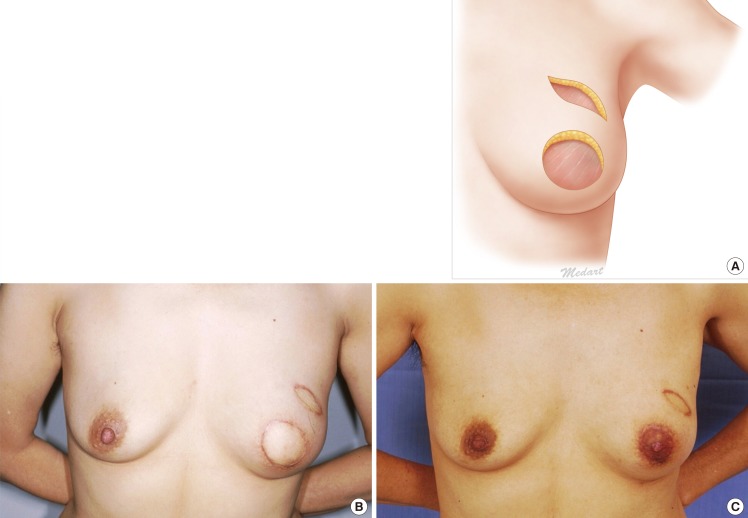
Breast reconstruction after mastectomy with the peri-areolar and second elliptical incisions
A second elliptical skin paddle allows reconstruction with a muscle-sparing free transverse rectus abdominis myocutaneous (ms-TRAM) flap following the excision of a distant biopsy scar: (A) prereconstruction schematic, (B) postoperative view, and (C) following nipple reconstruction. The outline of the nipple-areolar complex is entirely preserved, and the scar is well-hidden while the second skin paddle remains small and relatively inconspicuous.
3) The third group of patients commonly seen consists of those with a radial biopsy scar within the distance of one-areola-diameter from the NAC. A radial extension of the incision from the peri-areolar design will be most appropriate in this case. The incision opens up as a "tear drop" to allow the excision of the biopsy scar and is closed in the configuration of a "racquet handle" (Fig. 4) [10]. A limit of one-areola-diameter's distance of the biopsy scar from the NAC is chosen for extension of the peri-areolar incision design as a more peripherally sited biopsy scar would require the resection of an unnecessarily large area of breast skin envelope.
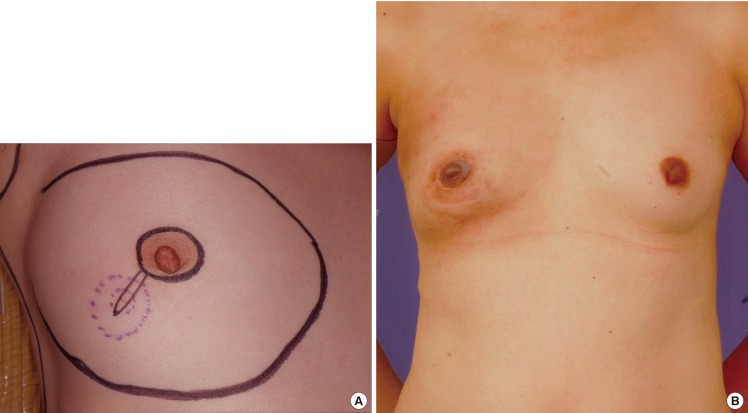
Breast reconstruction after mastectomy with the "racquet handle" incision
Design of incision in patients with a radial biopsy scar and underlying tumor: (A) preoperative skin marking is designed to include the biopsy scar and is opened up in the form of a "tear drop" to allow excision of the tumor and (B) following reconstruction with a latissimus dorsi flap, the incision is closed in the form of a "racquet handle" with subsequent nipple reconstruction. The outline of the nipple-areolar complex is preserved in its entirety, and most of the scar is effectively camouflaged.
4) The fourth group of patients with a curvilinear or transverse biopsy scar poses a greater challenge in the planning of the incision design. While a conventional elliptical incision around the NAC can be used [7,11], our experience is that this leads to a "circle-within-a-circle" appearance with a less than desirable postoperative aesthetic result as described previously (Fig. 1). This is particularly noticeable on Asian skin, which tends to be more pigmented, particularly in the region of the breasts. Therefore, a peri-areolar skin incision with adjacent skin extension will allow both sufficient access to perform the mastectomy and reconstitution of the circle of the NAC, as much as possible, during insetting of the flap (Fig. 5).
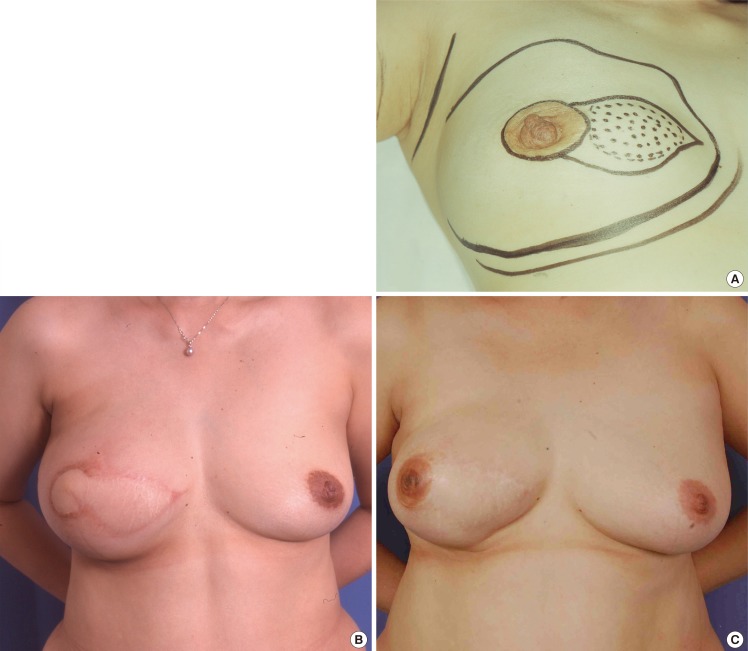
Breast reconstruction after mastectomy using the peri-areolar incision with adjacent skin extension
An extended peri-areolar incision used in instances where tumor involvement of the skin around the nipple-areolar complex necessitates the creation of an irregular, unsightly skin defect can still result in a satisfactory aesthetic result following reconstruction: (A) preoperative skin marking, (B) postoperative view following muscle-sparing free transverse rectus abdominis myocutaneous (ms-TRAM) flap reconstruction, and (C) following nipple reconstruction. The highly pigmented reconstructed nipple contrasts vividly with the paler skin paddle overlying the ms-TRAM flap used for reconstruction in this patient. However, reconstitution of as much of the nipple-areolar outline as possible optimizes the aesthetic result and reduces the area and extent of the flap skin encompassed by a pigmented scar at the flap-native skin boundary.
However, the NAC outline may not always be preserved. This may be due to oncological considerations such as the need for increased access to complete the mastectomy by performing a traditional elliptical incision or when the viability of the native breast skin envelope around the NAC is equivocal and requires further trimming. The post-reconstruction result is an unfavorable "circle-within-a-circle" appearance following nipple reconstruction because the NAC tends to stand out on the reconstructed skin paddle (Fig. 1). We also routinely excise the biopsy scar with a margin of 5 mm. In all cases, histological examination has shown these scar tissues to be tumor-free.
Techniques for nipple reconstruction
The NAC in Asian women typically has a pigmented appearance. Nipple reconstruction is thus performed using either a modification of the C-V flap technique [12]-after the elevation and suturing together of dermal flaps to produce a cylindrical form, de-epithelization of this construct and the surrounding neo-areola is performed prior to grafting with skin (split or full thickness) and subsequent tattooing as necessary-or contralateral nipple sharing [13] with split-thickness skin grafts. Donor sites for such skin harvest are obtained from the pigmented areas of the groin, perineum, or anoderm.
RESULTS
Incisions used for skin-sparing mastectomy by the resection surgeon included the peri-areolar design (n=124, 44%), peri-areolar design with a second distant skin paddle (n=39, 14%), "racquet handle" (n=21, 7.5%), and peri-areolar with adjacent skin excision (n=42, 14%). The traditional elliptical incision and other variants where the NAC outline was not preserved were performed in the remaining 55 patients for the reasons outlined above.
Modalities for reconstruction included a pedicled TRAM flap (n=113), muscle-sparing free TRAM flap (n=31), DIEP flap (n=9), SIEA flap (n=1), VRAM flap (n=1, as the patient had a previous caesarian section through a lower midline abdominal incision), myocutaneous LD flap (n=101), and LD flap with implant (n=25). The average postoperative follow-up was 44.7 months, and complications (Table 1) included hematoma (n=6), partial flap necrosis (n=7), seroma (n=2), and infection (n=1); there was one case of total flap loss but all of the other flaps survived. There were also 12 cases of mastectomy skin envelope necrosis that required further debridement and skin grafting of the mastectomy envelope (Table 2).
Data from our institution indicate that the recurrence rate of breast cancer from the use of these skin-sparing mastectomies is 3.6%. This is comparable to the results reported in the literature, which range from 3.5% to 19% [14,15,16].
DISCUSSION
The postoperative aesthetic result is the key to patient perception and ultimately, acceptance of skin-sparing mastectomy and immediate breast reconstruction. Such an approach has the distinct advantage of simultaneously achieving two disparate but intimate goals of surgical therapy for breast cancer-oncological clearance and improved cosmesis. Resection of the malignant lesion and all breast parenchyma including any previous open biopsy scar(s) is achieved; the original skin envelope of the breast is also preserved, as much as possible, to allow for the reconstitution of the breast mound with the best possible aesthetic result. Understandably, the major concern with this technique is the risk of cancer recurrence. Increasingly though, the evidence supports the oncological safety of such an approach [14,15,16] as concurred by our institution's recurrence rate of 3.6%. As such, a key principle in the design of incisions used during such skin-sparing mastectomies is to minimize the amount of native skin envelope resected and to ensure that this is performed with particular attention to the anticipated aesthetic outcome following reconstruction.
Our algorithm is a result of several considerations unique to our patient population. First, Asian skin has a tendency towards a higher incidence of hypertrophic scarring and keloids [17]. Hence, any additional extension of the mastectomy incision beyond the NAC would become highly visible as exemplified by the elliptical design, which results in relatively poor cosmesis as the donor skin tends to be markedly hypopigmented as opposed to the skin from the native breast envelope after autologous tissue reconstruction. Coupled with its pigmented appearance, reconstitution of the NAC outline, as much as possible, is paramount for ensuring a favorable aesthetic result after surgery in our patients. Second, our experience is that Asian skin tends to be less stretchable and leads to increased tension during wound closure with the resultant increased risk of poor scarring. Third, the rate of immediate breast reconstruction following skin-sparing mastectomy is already low to begin with (approximately 20%) [18], and most of our patients are particularly reluctant to undergo secondary procedures for further augmentation and correction due to personal preferences and cultural considerations. It is thus imperative that we can achieve the desired aesthetic outcome in as few procedures as possible.
A major concern with regard to skin-sparing mastectomy and immediate breast reconstruction is the risk of mastectomy skin envelope necrosis. Our reported figure of 4.2% (12/281) is comparable to that of the current literature, which ranges from 4% to 14% [10,19,20]. We believe that this risk is lowered in free TRAM reconstruction as compared to the pedicled TRAM due to a more robust blood supply available to the mastectomy skin flaps because the need to create a tunnel is avoided [21]. This was demonstrated by the success of our series with only 2 cases of mastectomy skin envelope necrosis (out of 12 in total) noted in the free-flap (muscle-sparing TRAM, DIEP, and SIEA) subgroup of patients. Other flap-related complications such as hematoma, infection, and seroma were all within rates comparable with those reported in the existing literature [21].
Following successful breast reconstruction, 68 patients (24%) underwent nipple reconstruction using the techniques described previously. The skin paddle on which the new NAC is to be created tended to be slightly larger than the contralateral NAC to relieve tension during wound closure. However, this may also lead to the "circle-within-a-circle" result following nipple reconstruction, as described previously (Fig. 1). We have thus devised a method to correct this less than desirable appearance during a secondary setting. The area of hypopigmented skin is excised, and the surrounding native breast envelope is undermined. This is followed by a peri-areolar closure with purse-string stitching in a cartwheel fashion similar to that described by Benelli (Fig. 6) [22].
Method for correction of the "circle-within-a-circle" deformity
Secondary correction of the "circle-within-a-circle" deformity: (A) preoperative view, (B) postoperative view demonstrating the new nipple-areolar complex (NAC), which is able to match the size and position of the contralateral NAC optimally, and (C) intraoperative view; after the area of hypopigmented skin paddle is excised, the native skin envelope is undermined and the use of purse-string stitching in a cartwheel pattern for peri-areolar closure.
Recently, Carlson [10] described four types of skin-sparing mastectomy incisions in the Western population. These incisions were similar to ours except for the modified Wise pattern incision recommended for contralateral breast reduction. Kinoshita et al. [23] have also reported a similar approach for Asian patients, which included regular skin-sparing mastectomies, nipple-sparing mastectomies, and implant reconstruction cases. Our present algorithm focuses on flap reconstruction after skin-sparing mastectomies and the aesthetic outcomes following nipple reconstruction in the Southeast Asian setting.
Notes
No potential conflict of interest relevant to this article was reported.

