The round-the-clock technique for correction of gynecomastia
Article information
Abstract
Background
Gynecomastia is a common condition that can cause severe emotional and physical distress in both young and older men. Patients in whom symptomatic recalcitrant gynecomastia persists for a long time are potential candidates for surgery.
Methods
From January 2014 to January 2016, 15 patients underwent correction of gynecomastia through a single 3-mm incision at our institution. Only patients with true gynecomastia underwent surgery with this new technique. Through the small incision, sharp dissection was performed in a clockwise and counterclockwise direction describing two half-circles. Health-related quality of life and aesthetic outcomes were evaluated using a modified version of the Breast Evaluation Questionnaire (BEQ).
Results
The patients’ average age was 23.5 years (range, 18–28 years), and their average body mass index was 23.2 kg/m2 (range, 19.2–25.3 kg/m2). One case was unilateral and 14 cases were bilateral. The weight of glandular tissue resected from each breast ranged from 80 to 170 g. No excess skin was excised. Bleeding was minimal. The mean operating time was 25 minutes (range, 21–40 minutes). No complications were recorded. All lesions were histologically benign. The patients’ average score was 3.5 (on a 5-point Likert scale) in all domains of the BEQ for themselves and their partners.
Conclusions
In this study, we demonstrated the safety and reliability of a new technique that allows mastectomy through an imperceptible 3-mm incision. We obtained high patient satisfaction scores using our surgical technique, and patients reported considerable improvement in their social, physical, and psychological well-being after surgery.
INTRODUCTION
Gynecomastia is the most common male breast deformity, occurring in up to 65% of adolescents and adult men [1]. It results in benign breast enlargement and is estimated to be bilateral in 50% of cases. This condition may be due to an excess of glandular tissue, fat, or a combination of both [2,3].
Although several factors can underlie this condition, the most frequent cause is idiopathic [1-3]. Indeed, determining the cause of the pathology is very important, as the proper treatment depends on the nature of breast enlargement. Ultrasonography and mammography are useful assessment tools in the diagnostic process. Enlargements characterized only by fat deposits, without glandular proliferation, are classified as pseudogynecomastia, which is also called lipomastia and accounts for most cases of breast enlargement in obese men [4-6]. In these patients, it is possible to decrease the breast prominence by a weight-loss and exercise program as a first-line treatment. Frequently, recurrence in patients affected by gynecomastia results from an imbalance between estradiol and testosterone, and such cases can resolve without surgical intervention. Gynecomastia can occur as a side effect of several drugs, but breast hypertrophy does not always resolve after discontinuation of the medication [7,8]. Pubertal gynecomastia can regress spontaneously, but sometimes it does not do so, resulting in enlargement with fibrosis of the glandular parenchyma and in an unfavorable breast appearance, which can be quite disfiguring and may lead to significant social and psychological impairment [7].
Various classification schemes of gynecomastia have been proposed, incorporating evaluations of the appearance of the breast, severity, and the composition ratio between fat and glandular tissue [4]. The most frequently used classification is based on the tissue components involved in gynecomastia and distinguishes three types: true gynecomastia, when only glandular tissue is the cause of breast enlargement; pseudogynecomastia, which refers to chest lipodystrophy; and mixed gynecomastia, which corresponds to a breast with hypertrophy of both fat and glandular parenchyma. Alternatively, according to the breast size and redundant skin, the grade of severity of gynecomastia can be assessed using the Simon scale [1].
Surgical intervention is recommended in case of recalcitrant gynecomastia, defined as cases that persist for longer than 12 months and do not resolve independently or with medical management. Several approaches have been used to treat gynecomastia, including surgical excision, suction-assisted lipectomy, excision of breast tissue and skin resection, and any combination of those three techniques [1,4,8-11].
Although gynecomastia is a benign condition, it can be physically uncomfortable and it can affect health-related quality of life (HRQOL) [7]. The condition can be associated with psychological trauma and can deeply affect the emotional and social behavior of the patient. In these cases, surgery plays a fundamental role in restoring the male breast appearance. Therefore, it is important to use a less invasive technique that does not alter the shape of the body and does not produce visible scars in patients who have long had problems showing their chest. Liposuction alone may be insufficient, especially in case of glandular hypertrophy, and it may be performed in combination with an incisional technique [3,4]. However, the removal of breast glands with conventional open surgical methods of excision frequently results in prominent and unpleasant scars, nipple asymmetry, excessive flattening, and retraction [2].
Herein, we describe and evaluate a novel surgical technique for treating gynecomastia through a small inferior areolar 3-mm incision, the round-the-clock technique, that provides optimal aesthetic results with minimal scars and a low complication rate.
METHODS
Patients
Fifteen male patients were diagnosed with grade 1 or 2 gynecomastia and underwent surgery through a single 3-mm incision at our institution [5,6]. The study was performed in accordance with the ethical standards of the Declaration of Helsinki and was approved by Institutional Review Board of Sapienza University (IRB No. 196257/24.10.13).
Each patient underwent a full clinical assessment with an endocrinological evaluation comprising blood tests and measurements of estradiol and testosterone levels, according to our Institutional protocol. Patients with a hormonal component were excluded. An ultrasound study was performed preoperatively to evaluate the morphology of the breast and the composition ratio between fat and glandular tissue. Only patients with true gynecomastia underwent surgery with this new technique. As previously reported, the ultrasound criteria used to diagnose true gynecomastia were as follows: non-mass, diffuse increment of the glandular tissue (subareolar anteroposterior mean thickness >1 cm); a nodular, discrete round or oval hypoechoic area in the subareolar region; and a flame-shaped, irregular hypoechoic area with extensions into the surrounding tissue [7,12].
Surgical technique
Patients were evaluated in the supine position to assess the perimeter and extent of the mammary glands. Markings were made with patients in the upright position, enabling a better evaluation of the amount and limits of tissue to be removed. The breast area was marked, after evaluation with the pinch test, along with a surrounding area of 4–5 cm where we performed liposculpture. Surgery was performed under local anesthesia with sedation and the patient was placed with both arms at the sides. We used a solution of local anesthesia with 1:100,000 epinephrine. A 3-mm skin incision was made along the inferior border of the areola at 6 o’clock (Fig. 1A). By lifting the subcutaneous tissue under the nipple–areola flap with a hook, it was possible to access the glandular tissues with a 360° range under direct vision (Fig. 1B-D). Furthermore, this maneuver enabled an intraoperative evaluation of nipple retraction by pulling the flap toward the incision, reducing the likelihood of overzealous tissue removal, which may produce an unpleasant flatness and concavity of the thorax.
Surgical technique
(A) Surgery was performed under local anesthesia and a 3-mm skin incision was made along the inferior line of the areola at 6 o’clock. (B-D) By lifting the subcutaneous tissue under the nipple–areola flap, it was possible to access the glandular tissue with a 360° range under direct vision. Through the small incision, blunt dissection was performed in a clockwise and counterclockwise direction, describing two half-circles. The breast tissue was pulled out, held with a Kocher clamp, and the gland was transected along its length. (E) Two or more pieces were removed with forceps in a half-circle fashion.
Through the small incision, sharp dissection was performed in a clockwise and counterclockwise direction, describing two half-circles. Then, breast tissue was pulled out and held with a Kocher clamp, and the dissection was performed with blunt scissors. The gland was transected along its length, and two or more pieces were removed with forceps in a half-circle fashion (Fig. 1E). The excised breast tissue was sent for histological evaluation. Careful hemostasis of subcutaneous bleeding was performed. Careful sharp dissection is a fundamental aspect of our technique in order to reduce the likelihood of bleeding. Especially in the posterior aspect of the glandular tissue, appropriate dissection can spare the perforating arteries from the pectoralis muscle [13]. Indeed, at this level, where the perforators directly pierce the fascia, the likelihood of damaging them is accompanied by a higher risk of bleeding.
Following excision, liposculpture of the area was performed in order to obtain better skin redraping and to avoid irregularities. Suction-assisted lipectomy was performed after the injection of a wetting solution, consisting of 500 mL of sterile physiologic normal saline, with the addition of 10 mL of 2% lidocaine, 10 mL of 1% ropivacaine, and 1 mL of 1:1,000 epinephrine. We routinely performed superficial liposuction with 3- to 4-mm cannulas in order to optimize skin redraping. No drain was required. The incised skin was closed with 4/0 Monocryl (Ethicon Inc., Cornelia, GA, USA) for subdermal sutures and 4-0 nylon. A pressure dressing was applied until the first follow-up examination.
Follow-up
The patients were followed up at 7 days, 3 weeks, 3 months, and 1 year postoperatively. Demographical, clinical, and surgical data were prospectively collected, including age, body mass index (BMI), type and grade of gynecomastia, amount of tissue excised, and the complication rate.
Evaluation of quality of life and outcomes
To the best of our knowledge, there is no validated outcome assessment questionnaire specific for gynecomastia correction and male breast surgery in general [14]. In a recent study, Ridha et al. [4] assessed the HRQOL and surgical outcomes of patients who underwent surgery for gynecomastia, developing a modified version of the Breast Evaluation Questionnaire (BEQ). The BEQ is a validated 55-item questionnaire for the assessment of patients’ satisfaction with HRQOL outcomes following various breast surgery procedures [15]. The authors changed the gender approach of the questions to make it appropriate for gynecomastia patients. The questionnaire evaluates patients’ comfort with breast/chest size, in dressed and undressed conditions in different settings. Furthermore, patients are asked to score the satisfaction level for themselves and their partners on a 5-point Likert scale.
Following the study of Ridha et al. [4], HRQOL was evaluated using the modified BEQ [4]. Surveys were given directly to patients at the 1-year follow-up clinic visit.
Statistical analysis
Patients’ sociodemographic characteristics, clinical characteristics, and complications were analyzed using descriptive statistics.
RESULTS
From January 2014 to January 2016, 15 patients underwent correction of gynecomastia with our technique. Two patients with a hormonal component were excluded from our case series. The patients’ average age was 23.5 years (range, 18–28 years), and their average BMI was 23.2 kg/m2 (range, 19.2–25.3 kg/m2). The average percentage compositions of glandular tissue and adipose tissue were 78.4%±4.75% and 21.5%±4.75%, respectively.
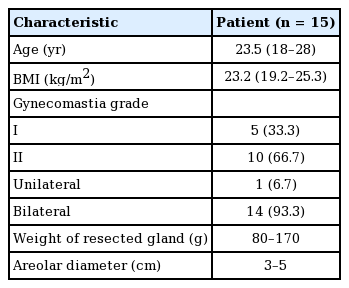
Table 1 presents the characteristics of the patients. One case was unilateral and 14 cases were bilateral. Five cases were grade 1, and 10 were grade 2. The areolar diameter ranged from 3 to 5 cm. The weight of glandular tissue resected from each breast ranged from 80 to 170 g. No excess skin was excised. Bleeding was minimal. The mean operating time was 25 minutes (range, 21–40 minutes), and all the procedures were performed by the same operator at a day hospital. All patients were discharged on the same day of surgery.
All patients were very satisfied with the results. The scars were generally well camouflaged in the areola, and there were no deformities (Figs. 2, 3). No complications were recorded. All lesions were histologically benign.
All the questionnaires were correctly completed. A satisfactory chest contour was obtained in all cases, with no abnormalities, skin redundancy, or recurrence at the 1-year follow-up. The patients’ average score was 3.5±0.6 (range, 2.5–4.7) on a 5-point Likert scale.
DISCUSSION
Gynecomastia is a common condition that can cause severe emotional and physical distress in young and older men. Patients in whom symptomatic recalcitrant gynecomastia lasts for a long time, and who experience psychological trauma or discomfort in social life, are potential candidates for surgery [2-4]. The goal of surgery is to reduce the breast size, while achieving a normal contour, removing fibrous and painful tissue, and restoring a normal masculine body image, with the smallest possible scar [3]. Various surgical approaches have been described, but the choice of surgical technique should be always individualized. Surgeons must carefully consider the degree of the gynecomastia, the glandular tissue-to-fat ratio, and the parenchyma distribution. Traditional surgery (i.e., subcutaneous mastectomy) efficiently removes the enlarged breast through a hemicircumareolar, periareolar, circumareolar, or transareolar incision [3]. Unfortunately, it has been reported that this approach can leave an unpleasant hollow defect in the soft tissue of the chest, yielding cosmetically unsatisfactory results in up to 50% of patients [2,13-17]. Liposuction can correct abnormal and excessive collections of fatty tissue and is associated with few complications, but it is not effective for patients with true gynecomastia who still require open surgery. In a recent study, endoscope-assisted subcutaneous mastectomy was successfully performed using three small incisions, with excellent cosmetic and surgical outcomes [2].
In this study, we demonstrated the safety and reliability of a new technique that allows mastectomy through an imperceptible 3-mm incision. Limiting the extent of the incision as much as possible is an important consideration for these patients, for whom prominent and visible scars might become a new source of shame and self-consciousness, reducing the benefits of surgery.
Our approach uses an endoscopic-like incision, reducing the invasiveness of the procedure and improving the cosmetic outcomes. The method is simple and relies on the ability to excise the enlarged glandular tissue in a round-the-clock fashion, with removal through a 3-mm incision. Hooking the subcutaneous tissue underlying the nipple-areola flap guides the operation in a completely open approach and enables the amount of tissue removal to be evaluated, reducing the likelihood of nipple retraction, which is a frequent complication of the traditional technique.
In our case series, no complications were reported and the blood loss was insignificant. A frequent occurrence in gynecomastia surgery is conspicuous bleeding, often requiring the use of drainage; indeed, an early complication of the traditional technique is hematoma, which sometimes needs to be drained with the patient returning to the operating room. Using our technique, we did not apply drainage and did not report any postoperative bleeding or hematoma. A possible explanation may be that the dissection of the posterior aspect of the glandular tissue was careful and sharp, which might have spared the perforating arteries from the pectoralis muscle. Indeed, blood is supplied to this region primarily by the internal thoracic artery, via its perforating branches, and secondarily by the anterior intercostal arteries and the lateral thoracic artery [13]. It was found that the perforating branches from the internal thoracic artery often coursed relatively parallel to each other in a lateral direction. Then, they ran tortuously either above or below the nipple toward branches from the lateral thoracic artery [13]. Precisely at this level, where the perforators directly pierce the fascia, the likelihood of damaging them is accompanied by a higher hazard of bleeding. In our technique, the breast tissue is gently pulled out and excised in two or more different pieces with blunt dissection.
Patients with pseudogynecomastia can also be treated with our technique, but they additionally need traditional liposuction, not superficial liposuction. Indeed, in pseudogynecomastia, liposuction plays the most effective role in resolving the condition and can also be performed alone. We usually reserve our technique for patients with an estimated percentage of glandular tissue at least 50%.
We obtained high patient satisfaction scores with our surgical technique, and patients reported major improvement in their social, physical, and psychological well-being after surgery. The use of a small incision promoted high levels of satisfaction regarding scarring and the nipple-areolar complex, highlighting the importance of scarring and nipple distortion in gynecomastia patients.
Hammond et al. [18] described a similar technique for gynecomastia that involved a pull-through surgical excision and ultrasonic liposuction. The authors reported a series of patients undergoing resection through a 1-cm incision in the inframammary fold or a periareolar location. In our series, we used only periareolar incisions, and we found that a smaller incision (3 mm) was sufficient to adequately pull out and expose the glandular tissue, improving aesthetic results and patients’ reported outcomes. Through this small incision, blunt dissection was performed in a clockwise and counterclockwise direction, describing two half-circles, and the gland was transected along its length. This procedure follows the physiological disposition of the glandular tissue around the nipple with its peripheral extensions, enabling careful excision and reducing the possibility of sparing residual parenchyma. Conversely, in previous reports, excision was performed by pulling out the tissue and removing it in strands, without following a precise pattern.
Furthermore, in the technique described by Hammond et al. [18], ultrasonic liposuction was applied before excision of the glandular tissue. In our study, liposculpture of the area was performed after the excision, in order to obtain better skin redraping and to avoid irregularities. We believe that liposuction can play a key role in the final step of this procedure, with the goal of minimizing any irregularities [19,20]. After the resection, the surgeon can properly evaluate the stored area of fatty tissue and the presence of any unpleasant, irregular defects. In our opinion, performing liposuction first can hinder the following procedure of precise excision through a small incision. In our technique, careful excision is performed in a clear and avascular plane. We believe that after complete removal of the glandular tissue, the surgeon can properly assess the amount of tissue to remodel. In our experience, late excision after liposuction increases the likelihood of overcorrection and an unpleasant irregularity, which is one of the main pitfalls of surgery for gynecomastia. Moreover, final liposuction can remove any excess fluid and retained fat, reducing fluid collection and the rate of postoperative complications.
Correction of gynecomastia does more than fix a physical problem; it also yields significant improvements in patients’ social and emotional life. Surgery aims to restore a pleasant physical appearance, relieving psychological trauma and increasing self-esteem. Herein, we describe a new surgical approach for gynecomastia that creates an inconspicuous scar and provides excellent surgical, aesthetic, and HRQOL outcomes, while avoiding the usual complications.
Notes
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Sapienza Hospital (IRB No. 196257/24.10.13) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.
Author contribution
Conceptualization: Tarallo M, Ribuffo R. Data curation: Tarallo M, Di Taranto G, Fallico N. Formal analysis: Tarallo M, Di Taranto G, Fallico N. Funding acquisition: Tarallo M, Ribuffo D. Methodology: Tarallo M, Ribuffo D. Project administration: Tarallo M, Ribuffo D. Visualization: Tarallo M, Di Taranto G, Fallico N. Writing - original draft: Di Taranto G, Fallico N, Tarallo M. Writing - review and editing: Tarallo M.