Subunit Principle of Vulvar Reconstruction: Algorithm and Outcomes
Article information
Abstract
Background
Vulvar defects result chiefly from oncologic resection of vulvar tumors. Reconstruction of vulvar defects restores form and function for the purpose of coitus, micturition, and defecation. Many surgical options exist for vulvar reconstruction. The purpose of this article is to present our experience with vulvar reconstruction.
Methods
From 2007 to 2013, 43 women presented to us with vulvar defects for reconstruction. Their mean age at the time of reconstruction was 61.1 years. The most common cause of vulvar defect was from resection of vulvar carcinoma and extramammary Paget's disease of the vulva. Method s of reconstruction ranged from primary closure to skin grafting to the use of pedicled flaps.
Results
The main complications were that of long term hypertrophic and/or unaesthetic scarring of the donor site in 4 patients. Twenty-two patients (51%) were able to resume sexual intercourse. There were no complications of flap loss, wound dehiscence, and urethral stenosis.
Conclusions
We present a subunit algorithmic approach to vulvar reconstruction based on defect location within the vulva, dimension of the defect, and patient age and comorbidity. The gracilis and gluteal fold flaps are particularly versatile and aesthetically suited for reconstruction of a variety of vulvar defects. From an aesthetic viewpoint the gluteal fold flap was superior because of the well-concealed donor scar. We advocate the routine use of these 2 flaps for vulvar reconstruction.
INTRODUCTION
Vulvar defects result chiefly from oncologic resection. Vulvar cancer comprises 5% of all female genital cancers and 1% of all female malignancies. The worldwide incidence of vulvar cancer peaks at 65 to 70 years of age and has been increasing in developed countries [1]. In Singapore, squamous cell carcinoma and vulvar intraepithelial neoplasia are the most common histological types of vulvar cancer [2]. The mainstay of treatment for vulvar cancer is wide surgical resection and radiation if necessary. Extramammary Paget's disease of the vulva (vulvar intraepithelial adenocarcinoma) is another common vulvar tumor treated with wide local excision [3]. Without reconstruction, surgical resection would result in mutilation and poor wound healing of the perineum, delaying delivery of any requisite adjuvant radiotherapy.
Reconstruction aims to restore anatomy and function of the external female genitalia, facilitating preservation of normal body image, sexual function, and micturition and defecation functions. The purpose of this paper is to describe our experience in 43 consecutive patients and to propose an algorithmic approach to vulvar reconstruction based on our experience.
METHODS
Forty-three patients underwent vulvar defect reconstruction between 2007 and 2013. Their mean age at time of surgery was 61.1 years (range, 35 to 83 years). The underlying vulvar conditions are summarized in Table 1. The most common pathological conditions in our series were vulvar carcinoma and extramammary Paget's disease of the vulva (86%).
There were 22 unilateral and 21 bilateral defects (Table 1). Defects were empirically classified as small defects (those which may be closed directly with undermining or with local flaps), medium defects (primary closure of these would lead to severe distortion of the perineum), and large defects (these cannot be closed directly without risk of dehiscence). Among unilateral defects there were 7 small defects (64 to 84 cm2), 10 medium defects (104 to 126 cm2), and 5 large defects (150 to 260 cm2). Among bilateral defects there were 2 medium defects (104 to 144 cm2) and 19 large defects (165 to 440 cm2). Fifty per cent of patients who had large defects required groin node dissection. The mean follow-up period was 30.2 months (range, 24 to 38 months).
The main flaps used (Table 1) included the gracilis flap (n=24), the gluteal fold flap (n=7), the medial thigh flap (n=5), and the vertical rectus abdominis myocutaneous (VRAM) flap (n=3).
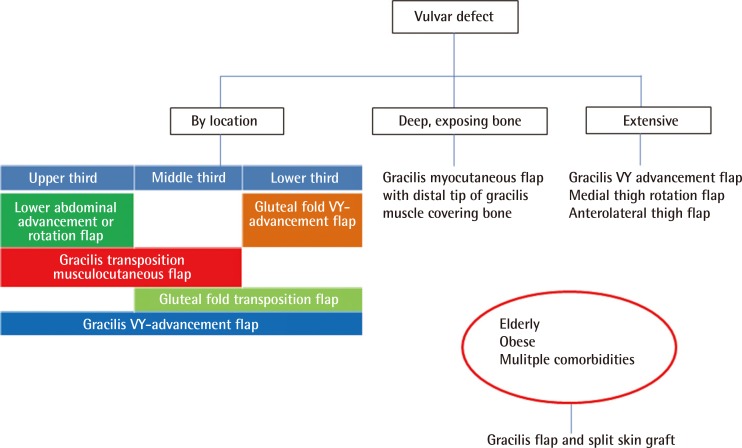
The method of reconstruction and choice of flap depended on the extent and location of the vulvar defect (Fig. 1). From the lithotomy perspective the vulva could be divided into three subunits. The upper third subunit consists of the mons pubis extending into the labia; the middle third is the labia proper; and the lower third consists of the vaginal orifice and perineum. For instance (Fig. 1), gluteal fold transposition flaps comfortably reached the middle third but fell short of the upper third. Likewise, upper third defects were easily covered by abdominal local flaps but these could not reach posteriorly. Other subunits included the vaginal walls and the periurethral area which are deeper.
Surgical technique
Flap elevation techniques for the above flaps are well-established and we raised them in the standard fashion. Special attention was paid to the following: 1) After resection in the lithotomy position with the legs supported by Allen Yellofin stirrups, the patient was repositioned. The stirrups were extended to straighten the knees and the entire lower limbs were free-draped for added mobility (Fig. 2). We ensured the stirrups were hinged in a manner that allowed full adduction at completion of surgery. The lower buttocks were pulled over the edge of the operating table with the patient resting on the upper sacrum if gluteal fold flaps were planned. This saved turning the patient twice. This setup was critical as we gradually adducted the hips in the course of closure to distribute wound tension. We avoided pole stirrups as the hips are unnaturally splayed, widening the wounds. 2) The urinary catheter was temporarily detached and plugged for ease of catheter manipulation during periurethral stitching. 3) When medial thigh flaps were used-gracilis included-the long saphenous vein with its perivascular lymphatics were preserved to minimize the risk of lymphedema. 4) When stitching a deep recess or around the urethra or anus, key stitches were placed and left untied initially. They were then sequentially tied once it was determined that all stitches were evenly distributed. Routinely, vicryl 2/0 and 3/0 were used. For skin grafting deep recesses, we liberally used fibrin glue to secure the skin graft without stitches. 5) Postoperatively the patient was nursed supine with an electric fan to aerate the perineum. She was nursed prone if the defect was predominantly posterior (case 40). Tetracycline 3% ointment was applied to the wounds liberally. For antibiotic prophylaxis, a combination of intravenous rocephine, flagyl, and cloxacillin, or intravenous tazocin alone were used.

Intraoperative positioning for vulvar reconstruction
Intraoperative positioning of patient on Allen Yellofin stirrups. The knees are extended and stirrups hinged in a manner that allows adduction of the hips to reduce tension on the flaps during inset. The buttocks are exposed for the elevation of gluteal fold flaps in this case.
RESULTS
There were no major acute complications such as flap loss, wound dehiscence, and urethral stenosis. Minor complications included celllulitis (n=4) requiring prolonged antibiotic treatment, superficial tip necrosis of the flap (n=3), long term hypertrophic and/or unaesthetic scarring of the donor site (n=4), and anal contracture requiring regular dilatation (case 40). Twenty-two patients (51%) were able to resume sexual intercourse. There were no problems with urination and urine flow in all our patients.
There was no difference in complications rates comparing unilateral and bilateral defect reconstruction. Adjuvant radiotherapy was required in 4 patients and it was commenced after all wounds had healed. There were no local complications of radiation therapy. Six patients died of causes related to metastatic complications of vulvar cancer in the follow-up period. The survival rate of our patients was 86% at a mean follow-up period of 30.2 months.
All patients were generally satisfied with the results of reconstruction. The younger patients who underwent gluteal fold flap reconstruction were particularly appreciative of the hidden gluteal crease scar.
DISCUSSION
The goals of reconstruction include: providing quality skin cover thus minimizing scarring and distortion, restoring the vaginal introitus and vault, and maintaining the central position of the urethral meatus and preventing stenosis.
Good quality reconstruction includes external cover and inner lining. External features that we attempted to recreate include the hair-bearing mons, symmetrical labial folds, and the ano-vaginal partition which prevented faecal passage into the vagina.
Defects of the vaginal wall and any exposed pubic bone will be overgrown with granulation tissue, scar down, and ultimately lead to obliteration of the vault. There must be adequate lining to keep the introitus and vagina patent, thereby allowing maintenance of hygiene and resumption of sexual intercourse for those sexually active [1]. Half of our patients were able to return to sexual activity. Durable skin around the urinary meatus prevents meatal stenosis and distortion allowing normal urinary flow without wetting the inner thigh. Finally, skin cover also facilitates healing and a smooth transition to adjuvant radiotherapy if needed.
We have devised a reconstructive algorithm based on the size, location and depth of the vulvar defect (Fig. 1). Small vulvar defects were amenable to direct closure, skin grafting, and local flaps [4,5,6]. Any concomitant groin dissection would preclude the use of local flaps based on the superficial circumflex, epigastric and external pudendal arteries as these vessels would have been ligated. In this situation undermining and primary closure were preferred to fancy flaps (case 7).
The reconstructive needs in large defects include the need to fill dead space, cover the pubic bone (case 18) (Fig. 3) and line the periurethral area (cases 31, 32, 37). Large medial thigh rotation flaps and VY-advancement flaps fulfilled these needs well. In Paget's disease where reexcision is common because of involved margins, these flaps lent themselves well to repeat surgeries. The medial thigh VY-advancement flap has been described based on a subcutaneous pedicle, but in our experience, the same flap based on the medial femoral circumflex artery afforded better reach because it could be completely mobilized (Figs. 4, 5 showing respectively cases 2 and 34) [7]. A disadvantage of this flap was its tendency to pin-cushion and form hypertrophic borders (30% of cases). The medial thigh rotation flap was an alternative for large defects and although primary closure was always achieved, the result was a long curvilinear scar (cases 20, 40, 41). In both instances we preserved the great saphenous vein with a cuff of adipose tissue to prevent lymphedema. We have used the anterolateral thigh flap (case 38) for extensive vulvar cancer but needed to skin graft the lateral thigh donor site.
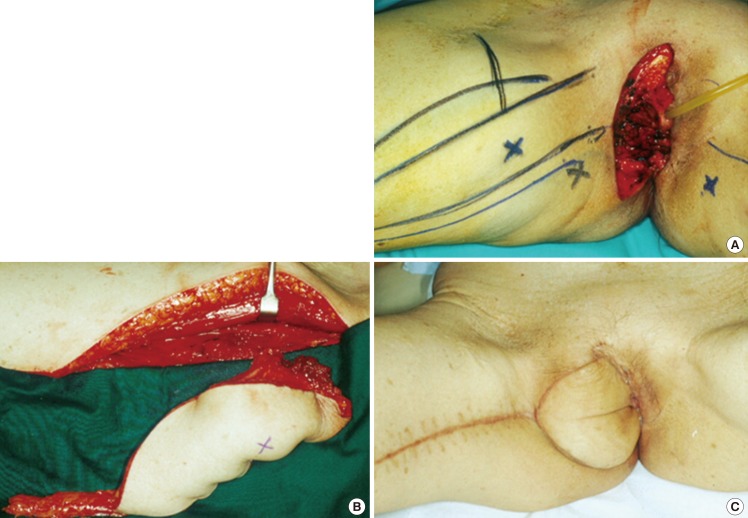
A case of myocutaneous gracilis transposition flap
Right vulvar squamous cell cancer in a 61-year-old (case 18). (A) Hemivulvectomy defect with pubic bone exposed and dead space to fill. (B) Right myocutaneous gracilis flap with its slender distal muscular end. (C) Flap was transposed and inset with distal muscle filling deep bony cavity; donor site was closed primarily; the result shown at one year postoperatively.
A case of myocutaneous gracilis transposition flap
Vulvar cancer in a 74-year-old (case 2). (A) Vulvectomy defect. (B) Left myocutaneous gracilis flap. (C) Flap was transposed and inset into defect and donor site was closed primarily; the result shown at one year postoperatively.

A case of bilateral gracilis VY-advancement flaps
Paget's disease of the vulva in a 60-year-old (case 36). Bilateral gracilis VY-advancement flap reconstruction one year postoperatively showing a patent well-centered urethral meatus as a result of careful periurethral inset of the flaps.
Outer vaginal wall defects were easily covered with the superficial portion of the above flaps. However with deep vaginal vault defects exposing the pubic bone, the medial thigh skin was too bulky to fit in, let alone stitch. Instead, the distal slender portion of the gracilis muscle was used with skin grafts overlaid for lining (case 18) (Fig. 3) [8,9]. We used fibrin glue to secure the skin graft as it was impossible to stitch in a deep recess.
The VRAM flap (case 22) (Fig. 6) was used in a case of radical vulvectomy with pubic ostectomy for sarcoma. In planning the surgery we persuaded the colorectal surgeon to site the end-colostomy on the right side (and not the usual left) so that we could use the ipsilateral VRAM flap for better reach. Ordinarily the VRAM flap is not used because of its bulkiness. Additionally it risked abdominal hernia formation because the flap is pivoted where the posterior rectus sheath is deficient. However we used the flap in this case for added volume [10].

A case of vertical rectus myocutaneous flap
Post-reconstruction with left vertical rectus myocutaneous flap at 6 months follow-up in a 45-year-old patient who had sarcoma (case 22). Note colostomy was sited to the right (instead of usual left) to facilitate optimal wound coverage with an ipsilateral rectus flap.
The urethra meatus was involved and partially resected in 6 (29%) of our 21 cases with extramammary Paget's disease. Three cases were surfaced with unilateral flaps and the rest were with bilateral flaps. The flap edge chosen had to be well-vascularized and thin, and periurethral inset was done meticulously with interrupted vicryl 3/0 sutures. If reconstruction was done with paired bilateral flaps, we took care to ensure that the meatus was circumferentially lined.
From an aesthetic viewpoint the gluteal fold flap (Figs. 7, 8 showing respectively cases 11 and 24) was superior because of the well-concealed donor scar [11,12]. However its reach was limited to the lower and middle thirds of the vulva. The gluteal fold flap was designed as a transposition or VY-advancement flap. For upper third defects, we preferred the gracilis myocutaneous transposition flap which left a short linear medial thigh scar (case 2) (Fig. 4). We had minimal complications with the gracilis and gluteal fold flaps (Table 1) and recommend their routine use as workhorse flaps for vulvar reconstruction.

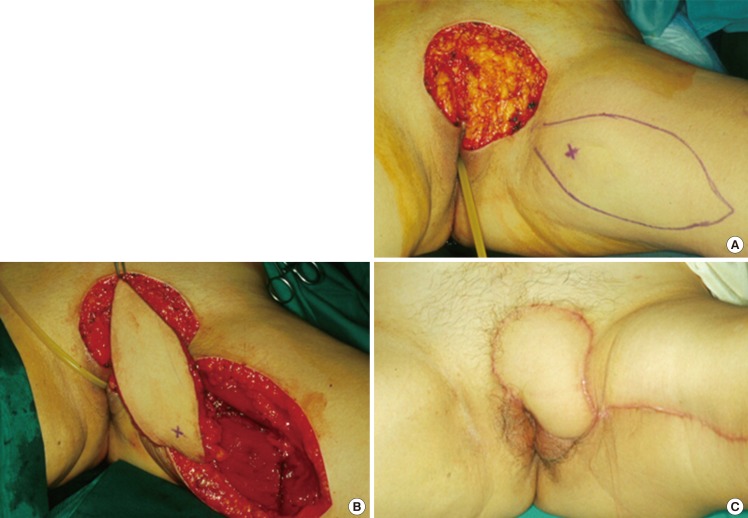
A case of gluteal fold transposition flap
Paget's disease of the right vulva in a 63-year-old (case 11). (A) Vulvectomy defect with perforators dopplered. (B) Right gluteal fold flap. (C) Flap was transposed and inset into defect and donor site was closed primarily; the result shown at one year postoperatively with a well-concealed donor-site in the gluteal crease.

A case of bilateral gluteal fold VY-advancement flaps
Post-reconstruction with bilateral gluteal fold VY-advancement flaps at 1 year follow-up in a 51-year-old patient (case 24) who had bilateral Paget's disease of the vulva.
Despite our elaborate reconstructive algorithm, the patients' age, body mass index, and comorbidities were taken into account. 60% of our patients were elderly (60 years and above) with multiple comorbidities such as ischemic heart disease and diabetes mellitus. Also 20% of our patients were severely obese. In these patients we preferred the gracilis muscle flap and skin grafting which was speedy, technically less demanding, and devoid of donor site morbidity (case 17) (Fig. 9).
Notes
No potential conflict of interest relevant to this article was reported.