The Clinical Course of Reverse-flow Anterolateral Thigh Flap: Need to Prepare for Venous Congestion and Salvage Operation
Article information
Recently, the reverse-flow (distally based) anterolateral thigh flap has been used for soft tissue reconstruction around the knee [1-5], and it has several advantages such as a long pedicle, a sufficient amount of tissue, possible composite transfer with fascia lata and minimal donor site morbidity [1]. However, this flap has a risk of venous congestion from the reverse blood flow and resistance of the venous valves [2-4]. This might cause the development of flap failure. In the cases of flap-threatening venous congestion after the reconstruction of an oncologic defect of the knee with reverse-flow anterolateral thigh island flap, the authors performed venous supercharge using the greater saphenous vein with a reliable vessel diameter and salvaged the flap successfully. We present the clinical considerations in the salvage of a venous congested reverse-flow anterolateral thigh flap and the clinical course of this flap with a literature review.
A 54-year-old male patient presented with a mass of 7×6 cm on the left knee. Biopsy of the lesion revealed a myxofibrosarcoma. The distant metastasis was not detected in preoperative evaluation. After wide excision of the malignancy, a soft tissue defect with a dimension of 8×8 cm over the left knee was noted (Fig. 1). We planned for the reconstruction the composite defect using a distally based anterolateral thigh island flap.

After wide excision of the myxofibrosarcoma, a soft tissue defect with a dimension of 8×8 cm over the left knee was noted.
The perforators were detected with a hand held Doppler probe preoperatively. The anterolateral thigh island flap including a musculocutaneous perforator was elevated and the descending branch of the lateral circumflex femoral vessel was dissected distally. The descending branch contained two venae comitantes. Two valve areas were observed at the pedicle between the flap and the descending branch. We clamped the pedicle proximally to assess the retrograde flow into the flap. After observation for the flap circulation, the pedicle was ligated proximally. Venous engorgement was detected at the area proximal to the venous valve before the flap insetting. The pedicle measured 16 cm in length, with the pivot point located 7 cm above the patella. A split-thickness skin graft was performed to the closure of the donor-site without any tension. The refilling of the flap was relatively rapid immediately postoperatively; however, the venous congestion was not significant.
Venous congestion of the flap developed slowly postoperatively at 10 hours, and worsened at 15 hours, threatening the survival of the flap; a reoperation was thus performed. A thrombus had formed at the proximal site of the venous valve and obstructed the venous drainage. After opening the ligated proximal venous end, we removed the thrombus and planned venous supercharge.
The greater saphenous vein was detected at the medial side of the knee, and dissected 30 cm in length to reach the proximal venous end of the descending branch of the lateral circumflex femoral vessel. The venous supercharge was performed through the anastomosis of the greater saphenous vein and the vena comitans of the descending branch of the lateral circumflex femoral artery (Fig. 2). The diameter of the greater saphenous vein was 2 mm. After the venous supercharge, the congestion of the flap was improved and the flap survived. Partial necrosis developed in the distal part of the flap. The necrotic tissue was debrided and covered with minor wound revision (Fig. 3).
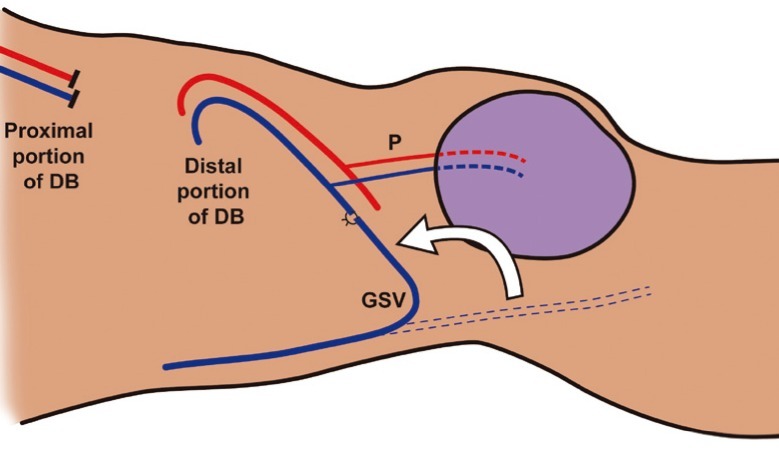
The scheme of the venous supercharge of the distally based anterolateral thigh island flap using the greater saphenous vein. DB, the descending branch of the lateral circumflex femoral vessel; P, the perforator to the anterolateral thigh island flap; GSV, the greater saphenous vein.
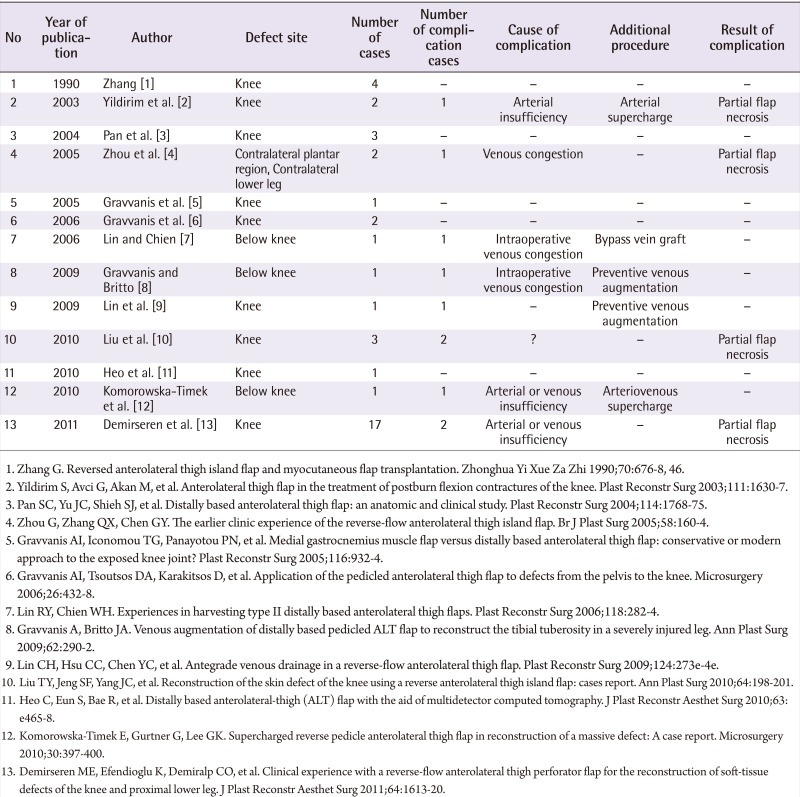
Through a review of the literature of cases of reverse-flow anterolateral thigh flap (Appendix), we find that the flap has a noticeable clinical course (Fig. 4). If the perforators do not arise from the descending branch of the lateral circumflex femoral artery, the flap should be raised as a free flap or a bifurcation of the transverse and descending branch of lateral circumflex femoral vessel should be included or a bypass vein graft used [1,2].
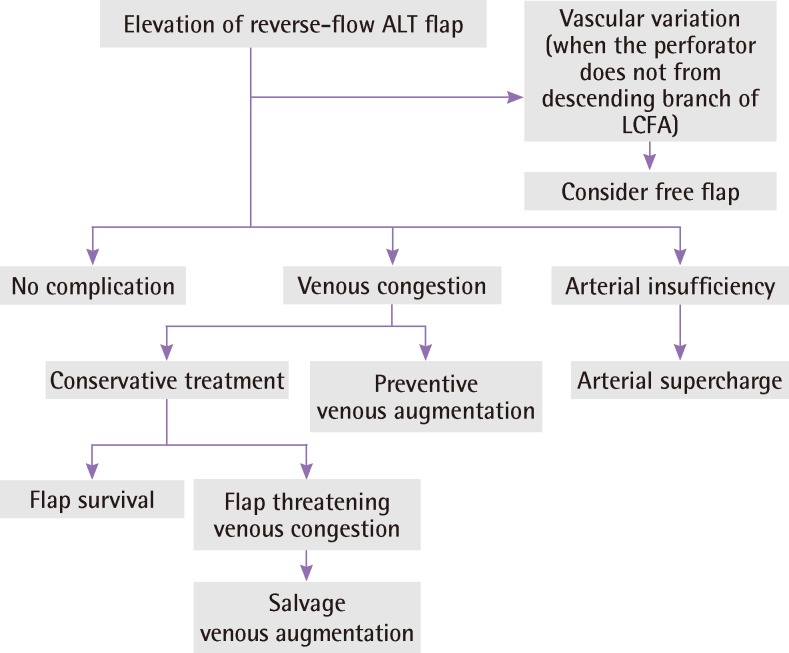
The clinical course of reverse-flow anterolateral thigh flap. ALT, anterolateral thigh; LCFA, lateral circumflex femoral artery.
In a large number of cases, this flap had no complications [1,5]. Two cases of necrosis of partial flap among 17 cases were reported by Demirseren et al. [5], while no vascular complications in 3 cases were noted by Pan et al. [1] who claimed that the flap is safe and reliable.
However, the reverse-flow anterolateral thigh flap has a risk of venous congestion because of the reverse blood flow and resistance of the venous valves [2,3]. The authors believe that the kinking and tension of the pedicle after the flap insetting were also possible causes of venous congestion. Some previous reported cases of venous congestion have been resolved with conservative treatment, but we experienced flap-threatening venous congestion, salvaged by venous supercharge using the greater saphenous vein.
It is crucial to make a proper decision when venous congestion develops during or after a reverse-flow anterolateral flap operation. If the venous congestion occurs directly after the temporary clamping of the proximal portion of the pedicle, some alternatives which can save the flap are available, such as venous augmentation [3,4], vein graft for bypass [2], or free flap [1]. However, if the venous congestion occurs insidiously, as in this case, there is a need for close monitoring of the flap. Furthermore, if the venous congestion is severe enough to threaten the survival of the flap, reoperation needs to be performed. We believe that the venous engorgement between the venous valve and the flap is an indicator of the potential need for supercharge in the reverse-flow anterolateral thigh flap of slowly developed venous congestion according to our clinical experience.
The reverse-flow anterolateral thigh flap could be worthwhile method in the soft tissue reconstruction around the knee through a consideration of the clinical course and preparation for venous congestion and salvage operation.
Notes
No potential conflict of interest relevant to this article was reported.
Appendices
Appendix
Cases of reverse-flow anterolateral thigh flap in the literature