How to approach orthognathic surgery in patients who refuse blood transfusion
Article information
Abstract
Background
Some patients who need surgery refuse a blood transfusion because of their religious beliefs or concerns about blood-borne infections. In recent years, bloodless surgery has been performed successfully in many procedures, and is therefore of increasing interest in orthognathic surgery.
Methods
Ten Jehovah’s Witnesses who visited our bloodless surgery center for orthognathic surgery participated in this study. To maintain hemoglobin (Hb) levels above 10 g/dL before surgery, recombinant erythropoietin (rEPO) was subcutaneously administered and iron supplements were intravenously administered. During surgery, acute normovolemic hemodilution (ANH) and induced hypotensive anesthesia were used. To elevate the Hb levels to >10 g/dL after surgery, a similar method to the preoperative approach was used.
Results
The 10 patients comprised three men and seven women. Their average Hb level at the first visit was 11.1 g/dL. With treatment according to our protocol, the average preoperative Hb level rose to 12.01 g/dL, and the average Hb level on postoperative day 1 was 10.01 g/dL. No patients needed a blood transfusion, and all patients were discharged without any complications.
Conclusions
This study presents a way to manage patients who refuse blood transfusions while undergoing orthognathic surgery. rEPO and iron supplementation were used to maintain Hb levels above 10 g/dL. During surgery, blood loss was minimized by a meticulous procedure and induced hypotensive anesthesia, and intravascular volume was maintained by ANH. Our practical approach to orthognathic surgery for Jehovah’s Witnesses can be applied to the management of all patients who refuse blood transfusions.
INTRODUCTION
In recent years, there has been a growing demand for bloodless surgery in many surgical fields, including general surgery, arthroplasty, and even oncologic surgery. In the past, blood transfusions were often necessary in these surgical procedures because of excessive bleeding. However, a major concern is posed by patients who need surgery, but—because of religious beliefs or concerns regarding the blood-borne transmission of pathogens (e.g., HIV)—refuse transfusions. Recent developments in medication, surgical techniques, and instrumentation have reduced both the risks of bleeding and the operation time. With these developments, bloodless surgery has been performed successfully in many procedures [1-3].
Orthognathic surgery is widely used to correct three-dimensional facial deformities, but there is a risk of excessive bleeding because of the complicated vascularity of the maxillofacial region [4]. Excessive blood loss can be potentially fatal and can necessitate a blood transfusion [5]. However, developments in medication, surgical techniques, and instrumentation have improved the outcomes and reduced the risks of bimaxillary surgery. Bloodless surgery has also been developed to the point that it can be used in orthognathic surgery.
Our bloodless surgery center has successfully performed many surgical procedures without transfusions, and we have applied this method to Jehovah’s Witness patients, who never consent to blood transfusions because of their religious beliefs. This practical approach to orthognathic surgery in Jehovah’s Witnesses can be applied to the management of all patients who refuse blood transfusion.
METHODS
The study involved 13 patients who visited our non-blood transfusion treatment center and underwent orthognathic surgery from January 1, 2013 to March 31, 2016. The possible need for transfusion due to massive bleeding loss after orthognathic surgery was explained to them. They all refused blood transfusion based on their beliefs as Jehovah’s Witnesses. In cases where heavy blood loss is expected during surgery in patients who have not consented to receive a blood transfusion, the operation can be performed according to the guidelines established at our bloodless surgery center (Fig. 1).
Guidelines for patients who refused blood transfusion
Patients received subcutaneous (SC) administration of recombinant erythropoietin (rEPO) (4,000 U, darbepoetin) and intravenous (IV) administration of one dose of iron supplementation (Venoferrum; ferric hydroxide sucrose complex, 100 mg).
Patients with heart or lung diseases were excluded based on a thorough medical history. For patients who were taking hemorrhagic drugs (nonsteroidal anti-inflammatory drugs, aspirin, anticoagulant, steroids, herbal medicine, etc.), it was checked whether the drugs could be discontinued for a certain period of time. If the drugs could not be discontinued, the patients were excluded. Of the 13 patients, 10 were enrolled in this study.
The ethics committee of Soonchunhyang University Bucheon Hospital (IRB No. 2020-05-042) approved the protocol of this study.
Preparation before surgery
Hemoglobin (Hb) levels were checked when a person who requested orthognathic surgery without blood transfusion first visited our bloodless surgery center. To manage their Hb levels, subcutaneous administration of recombinant erythropoietin (rEPO; darbepoetin alfa, 4,000 U) and intravenous iron supplementation (Venoferrum; ferric hydroxide sucrose complex, 100 mg) were used. Our goal before surgery was to ensure that the patient’s Hb level was at least 10 g/dL to withstand intraoperative and postoperative bleeding.
Therefore, we started different treatments depending on whether the patient’s Hb exceeded 10 g/dL (Fig. 1). If the Hb level exceeded 10 g/dL, 4,000 U of rEPO was administered subcutaneously and 100 mg of iron supplementation was administered intravenously once prior to surgery. After 1 week, patients underwent surgery. If the Hb level was ≤10 g/dL prior to surgery, repeated treatments were required to increase the Hb level to more than 10 g/dL. To do so, 4,000 U of rEPO was administered subcutaneously three times weekly, and 100 mg of iron was administered intravenously daily. Hb levels were checked at 1-week intervals. When the Hb level exceeded 10 g/dL, surgery was performed 1 week later.
Intraoperative management
During surgery, acute normovolemic hemodilution (ANH) was used. At the start of surgery, the ratio of fluid to blood collected for hemodilution was planned to be between 1.5 and 2:1. After the patient was anesthetized, two units of blood (600 mL) was collected immediately, and 1,000 mL of crystalloid fluid was intravenously administered to maintain a systolic blood pressure above 90 mmHg. All collected blood was stored at room temperature and was infused to the patient after surgery. In all cases, the collected blood was kept within a closed circuit because of the religious beliefs of the patient.
Induced hypotensive anesthesia was also used in cooperation with an anesthesiologist. Vasodilators and blood pressure–lowering agents were administered by the anesthesiologist, but cardiac output was maintained even at low blood pressure. The anesthesiology team maintained a systolic blood pressure of 80–90 mmHg or a mean arterial pressure of 50–60 mmHg in patients with normal blood pressure, in preparation for sudden hemorrhage or shock.
Postoperative management
Postoperative management can be divided into two major categories. First, it was necessary to compensate for the decrease in Hb caused by intraoperative bleeding, and second, it was necessary to stop the subsequent bleeding quickly. After orthognathic surgery, Hb levels tend to decrease because of extensive bleeding, so rEPO and iron were used starting the day after surgery to compensate for the decrease. Specifically, 4,000 U rEPO was administered subcutaneously and 100 mg of iron supplementation was administered intravenously. The patient’s Hb level was checked on postoperative day (POD) 1 and every 2 days thereafter until it reached 10 g/dL or more (Fig. 1). If the Hb level was ≤10 g/dL on POD 3, rEPO and iron were administered. If the Hb level continued to be less than 10 g/dL, rEPO and iron were administered again. If the Hb level was >10 g/dL on POD 3 or 5, observations were made without rEPO and iron. Furthermore, tranexamic acid was used to stop the bleeding. After surgery, 1,000 mg of tranexamic acid was administered intravenously. From POD 1 to POD 3, 1,000 to 2,000 mg of tranexamic acid was administered depending on the amount and color of the drainage. After POD 3, if there was no bleeding tendency, tranexamic acid was discontinued.
Case
A 21-year old female patient was hospitalized with a class III malocclusion (Fig. 2). Her preoperative Hb level was 11.9 g/dL (hematocrit [Hct], 35.8 vol%). The possible need for transfusion due to massive bleeding loss after two-jaw surgery was explained to her. She strongly refused blood transfusion as a Jehovah’s Witness. Starting a week before surgery, rEPO and iron supplementation were administered once as detailed above. The patient’s Hb level immediately prior to surgery was 12.3 g/dL (Hct, 37.1 vol%). The day prior to surgery, the patient signed a Medical and Liability Release Form, which freed the hospital of legal repercussions in the event of problems arising from the lack of blood transfusion. After general anesthesia was established, two units (600 mL) were extracted by ANH. At 3 hours postoperatively, the patient’s Hb level was 9.4 g/dL. Bleeding at the surgical site was minimized using electrocautery and a meticulous surgical procedure. Five hours after surgery, the Hb level had dropped to 8.5 g/dL. The extracted blood was transfused within a closed circuit. The total blood loss during the operation was about 700 mL. The morning after surgery, the patient’s Hb level was 10.4 g/dL. The patient was cared for according to our hospital’s postoperative protocol. She was stable, with no critical changes to vital signs including systolic blood pressure, and experienced no postoperative complications. On the day of discharge, the Hb level was 10.7 g/dL (Hct, 32.2 vol%).
Preoperative and 4-month postoperative findings
A patient who underwent LeFort I osteotomy, BSSRO, and reduction genioplasty. (A) Preoperative photographic finding (anteroposterior view). (B) Preoperative photographic finding (lateral view). (C) Preoperative photographic finding (intraoral view). (D) Preoperative lateral cephalogram. (E) Postoperative photographic finding (anteroposterior view). (F) Postoperative photographic finding (lateral view). (G) Postoperative photographic finding (intraoral view). (H) Postoperative lateral cephalogram. BSSRO, bilateral sagittal split ramus osteotomy.
RESULTS
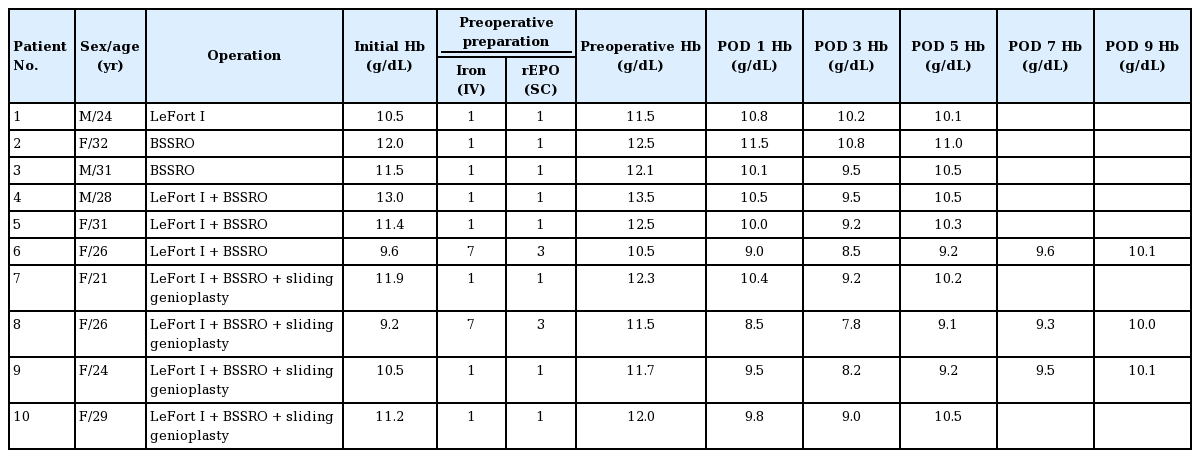
Ten patients underwent orthognathic surgery without transfusion, of whom three were men and seven were women. Their mean age was 27.2 years (range, 21–32 years). They underwent the following surgical procedures: one patient received a LeFort I procedure, two patients underwent bilateral sagittal split ramus osteotomy, three patients underwent a two-jaw procedure, and four patients simultaneously underwent two-jaw and genioplasty procedures (Table 1).
Eight patients had Hb levels >10 g/dL (mean, 11.5 g/dL; range, 10.5–13.0 g/dL) when they visited our bloodless surgery center. They were treated with rEPO and iron supplementation once before surgery. After our protocol, their mean Hb level increased to 12.3 g/dL (range, 11.5–13.5 g/dL) (Fig. 1). On the day after surgery, it decreased to 10.3 g/dL (range, 9.5–11.5 g/dL). On the third day after surgery, it continued to decrease, reaching 9.5 g/dL (range, 8.2–10.8 g/dL). Six patients with Hb levels less than 10 g/dL were treated again with rEPO and iron supplementation. Two patients with levels greater than 10 g/dL were discharged. On the fifth day after surgery, their Hb level increased (Fig. 3). The mean Hb of the remaining six patients was 10.2 g/dL (range, 9.2–10.5 g/dL).
Temporal patterns of hemoglobin levels
After implementing our preoperative protocol, the mean hemoglobin level increased to 12.3 g/dL. On the third day after surgery, the lowest levels were found. By fifth day after surgery, hemoglobin levels showed a tendency to increase. POD, postoperative day; BSSRO, bilateral sagittal split ramus osteotomy.
Two patients had Hb levels <10 g/dL when they first visited our bloodless surgery center. Their Hb were 9.6 and 9.2 g/dL, respectively. They were treated with rEPO and iron supplementation once. After 1 week, their Hb levels were found to be 10.1 and 10.2 g/dL, respectively (Table 1). Because their Hb levels were over 10 g/dL, after one more treatment with rEPO and iron supplementation, we planned surgery for 1 week after the last administration. Their preoperative Hb levels increased to 10.5 and 11.5 g/dL, respectively. Their Hb levels decreased until POD 3 and increased afterwards. However, their Hb levels remained under 10 g/dL until POD 7, and they therefore received rEPO and iron supplementation four times (immediately after surgery and on POD 3, 5, and 7). On POD 9, their Hb levels were 10 g/dL or more and rEPO and iron were no longer administered.
Patients were discharged when their Hb level increased to 10 or more. Seven patients were discharged on POD 5 and two were discharged on POD 9. Transfusions were not required in any patients and complications were not observed.
DISCUSSION
Blood transfusions are the norm in cases of orthognathic surgery that involve massive bleeding. For the past 10 years, our hospital has successfully provided various bloodless surgical procedures to Jehovah’s Witness patients and other patients who refuse blood transfusion. Our experiences have been positive.
Efforts have been made in the field of orthognathic surgery to measure, prevent, and predict blood loss. Pineiro-Aguilar et al. [6] conducted a systematic review of blood loss based on 17 studies, and the average intraoperative blood loss volume was 436.11±207.89 mL. Blood loss requiring blood transfusion was observed in 13 patients. Ueki et al. [7] measured blood loss during orthognathic surgery in 62 patients, and reported that 216.6±143.3 mL of blood was lost in sagittal split ramus osteotomy procedures, while 343.6±179.9 mL of blood was lost when sagittal split ramus osteotomy was performed together with LeFort I osteotomy. In studies of factors affecting blood loss [8,9], higher levels of blood loss were found in procedures with a longer operation time, bimaxillary surgery or LeFort I osteotomy, patients with a relatively low body mass index, and cases involving iliac bone grafting or genioplasty. In some cases [10], blood loss exceeded 2,000 mL. The use of tranexamic acid to prevent blood loss in orthognathic surgery [11] and the use of thromboelastography to predict blood loss [12] are efforts to reduce complications from bleeding and to minimize the need for blood transfusion. Therefore, as in our study, preparing for intraoperative blood loss by checking preoperative Hb levels and augmenting Hb if necessary is an appropriate method for patients who refuse transfusion.
In this study, the temporal pattern of Hb was measured from before surgery to various postoperative time points, and the mean values are presented according to the type of surgery (Fig. 3). In all graphs, the lowest Hb level was shown on POD 3, with a decrease of 2.8 g/dL compared to the preoperative Hb levels. Considering that healthy adults need to receive blood transfusions when their Hb level is lower than 7 g/dL, patient 8 would have been highly likely to need a transfusion if it had not been for the preoperative treatment because her Hb level was 7.8 g/dL on POD 3. Thus, checking postoperative Hb levels during follow-up and identifying trends in postoperative Hb increases can be an important factor in postoperative management.
Adherence to several aspects of the protocol is necessary. First, careful preoperative planning is crucial for successful outcomes. Prior to surgery, any risk factors that can exacerbate the patient’s condition due to bleeding must be minimized. It must be determined whether the patient is taking medication that could increase bleeding risk during surgery; examples include aspirin, nonsteroidal anti-inflammatory drugs, anti-coagulants, and anti-platelet agents. When possible, these medications should be stopped. Moreover, to adequately prepare for expected bleeding, the Hb level should be adequately raised before surgery. Preparing a method that can compensate for post-surgical hemorrhage is critical. In general, to support hematopoiesis, folic acid, vitamin B12, iron supplements, and/or rEPO can be applied. Shander and Javidroozi [13] reported that agents that promote hematopoiesis or hemostasis are acceptable to most Jehovah’s Witnesses.
Hb levels can also be effectively raised prior to surgery using rEPO and iron supplements. By stimulating erythropoiesis, EPO can produce the equivalent of 1 U of blood per week [14-16]. Lin et al. [17] and Bacuzzi et al. [18] reported that iron significantly reduced the need for blood transfusion in combination with EPO. Using rEPO and iron, we successfully improved patients’ Hb before orthognathic surgery. Patients’ average Hb level increased from 11.1 g/dL before surgery to 12.0 g/dL after approximately 7 days (Fig. 3). However, EPO has the known side effects of headaches and increased blood pressure. Dixon and Smalley [19] and Ball and Winstead [20] reported that this medication should not be administered to patients with high blood pressure that cannot be treated or to patients who are hypersensitive to medications. Therefore, such patients require particular care regarding the use of EPO.
The second relevant aspect is the intraoperative technique. Loss of blood during surgery must be minimized. Induced hypotension anesthesia can reduce bleeding by lowering the hydrostatic pressure of damaged vessels. Meticulous surgical technique is required to decrease intraoperative blood loss. This includes incorporating careful hemostasis methods, including using electrocautery, argon beam-enhanced dissectors, and ultrasonic coagulator dissectors (harmonic scalpels). Administering an appropriate anti-hemorrhagic agent can also be helpful for minimizing hemorrhage. Vitamin K as a coagulation factor and fibrinogen breakdown inhibitors, such as tranexamic acid and epsilon aminocaproic acid, can be used [21,22].
Other methods that can be used during surgery include ANH and autologous blood transfusion. ANH is a process of removing blood from the patient prior to surgery and maintaining intravascular volume by replacement with crystalloids and colloids [23]. Marsh and Bevan [24] reported that removed blood can be transfused when necessary, and if it is contained within a closed circuit, doing so may be acceptable to Jehovah’s Witness patients. However, patients with ischemic heart disease should be excluded because physiological compensation for the acute blood loss by an accompanying increase in cardiac output is possible. For this reason, three of the 13 initial patients were excluded from our study. Autologous blood transfusion methods could not be used in our surgical procedure because of the clean contaminated area.
The final aspect is postoperative patient management. After surgery, the average Hb level decreased from 12.0 g/dL to 9.1 g/dL on POD 3, but recovered quickly to 10 g/dL on POD 5. The bloodless surgery protocol we have devised alleviates the decrease in Hb levels caused by blood loss.
Even for orthognathic surgery, during which a significant amount of hemorrhaging is generally expected, loss of blood can be prevented through precautionary care using this approach. Also, reducing the operation time and amount of blood loss by putting together a skilled surgical team can be helpful. To avoid complications and risks related to transfusion, the methods used in our bloodless surgery center can be a novel choice for patients wishing to receive orthognathic surgery without transfusion.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Soonchunhyang University Bucheon Hospital (IRB No. 2020- 05-042) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consents were obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.
Author contribution
Data curation: SH Lee, DG Kim. Methodology: HS Shin. Project administration: HS Shin. Writing - original draft: SH Lee, DG Kim. Writing - review & editing: SH Lee, HS Shin.