Effects of hyperbaric oxygen on graft survival outcomes in composite grafting for amputated fingertip injury
Article information
Abstract
Background
Fingertip injuries are the most common type of traumatic injury treated at emergency departments and require prompt and adequate interventions for favorable wound survival outcomes. Hyperbaric oxygen (HBO2) therapy is well known for its many positive effects on wound healing. We hypothesized that treatment with HBO2 would improve the graft survival outcomes of amputated fingertip injuries treated with composite grafts.
Methods
This retrospective observational study included fingertip amputations that were treated between January 2013 and December 2017. A conventional group and an HBO2 therapy group were statistically compared to evaluate the effect of HBO2 treatment. Graft survival was categorized as either success or failure.
Results
Among 55 cases (digits), 34 digits were conventionally treated, while 21 digits were treated with HBO2. No statistically significant differences were observed between the groups with regard to general characteristics. Among patients with guillotine-type injuries, the composite graft success rate was statistically significantly higher in the group that received HBO2 therapy than in the conventional group (P=0.0337). Overall, the HBO2 group also demonstrated a statistically significantly shorter healing time than the conventional group (P=0.0075). As such, HBO2 treatment facilitates composite graft survival in cases of fingertip injury.
Conclusions
HBO2 treatment was associated with an increased composite graft survival rate in guillotine-type fingertip injuries and reduced the time required for grafts to heal.
INTRODUCTION
Among the various traumatic injuries treated at emergency departments, fingertip injuries are the most common and require prompt and adequate intervention for favorable outcomes [1]. We defined the fingertip as the portion of the digit distal to the insertion of the flexor and extensor tendons on the distal phalanx [2]. For amputated fingertip injuries, microsurgical replantation of the amputated fingertip to the stump is needed to achieve satisfactory recovery with regard to the length and function of the injured finger [3]. However, microanastomosis of the fingertip amputation distal to the germinal matrix of the nail is difficult and requires an experienced microsurgeon. In cases of crush injury in particular, the injured vessels of the fingertip are not suitable for microanastomosis [4,5]. Without early microanastomosis, the expected outcome is not favorable. Therefore, a composite graft with the distal stump can be a treatment option. Composite grafting of the fingertip is affected by plasma imbibition and vascular inosculation through the cut edges, and its success rate is associated with delicate surgical procedures and postoperative care [6]. To improve the survival outcomes of composite grafts, many adjuvant methods can be used [7-11].
Hyperbaric oxygen (HBO2) therapy is well known for its many positive effects on wound healing [12]. Previous animal studies have shown that the application of HBO2 to composite grafts in rats and rabbits increased graft survival [13,14]. Systemic HBO2 treatment increases oxygen diffusion, improves the condition of ischemia-reperfusion injuries, and stimulates angiogenesis [12]. For compromised flaps and grafts, HBO2 is typically applied at 2.0–2.5 atmospheres absolute (ATA) for 90- to 120-minute periods twice daily [15]. For split-thickness skin grafts, the application of HBO2 before and after surgery can improve the survival rate [16]. Many trials have been designed to verify the effect of hyperbaric therapy on composite grafts in animal studies. However, few clinical comparison studies have been conducted to analyze the effect of systemic HBO2 on composite grafts in humans. This study was conducted to evaluate the effect of systemic HBO2 on composite graft survival in cases of amputated fingertip injury.
METHODS
Study design and setting
In this retrospective observational study, we reviewed patients of all ages who were treated between January 2013 and December 2017 with composite grafting for fingertip amputations distal to the germinal matrix with microsurgically non-replantable distal amputated fingertips. We identified 55 consecutive patients with amputated fingertips who were admitted for surgical repair and adjunct treatments. The HBO2 therapy center in Korea is newly established [17]. Our institution opened this center with one multiplace chamber, in which six patients can be treated in one session, in October 2015. Patients treated prior to October 2015 received conventional adjunct treatments only, and consenting patients treated after the opening of the center received HBO2 in addition to the conventional adjunct therapies.
Electronic medical records, X-ray films, clinical photographs of the wounds, and demographic information were reviewed and recorded. We collected information regarding patient age, sex, medical history of hypertension and diabetes, smoking history, the specific digit involved, the level of the injury (or Allen classification), the geometry and mechanism of the injury, the time to surgery, the time from the injury to the first HBO2 treatment, the total number of HBO2 treatment sessions, and the healing time. The outcome analysis included only injuries with Allen classifications of types I, II, and III, the last of which involves distal phalanx fracture [18]. We categorized the mechanism of injury into either guillotine (clean-cut) or crush injury. A third subcategory, sawing injury, was represented as well, but we excluded it from the outcome analysis due to the small number of cases. We classified the geometry of the injury into four subgroups: dorsal oblique, volar oblique, lateral oblique, and transverse [7].
This study protocol was approved by the Institutional Review Board of Wonju Severance Christian Hospital (IRB No. CR-319010). Since this study was retrospective and observational, patient records and information were anonymously collected prior to analysis. Thus, the requirement for informed consent was waived.
Surgical management
When a patient visited the emergency department, an emergency physician evaluated the wound and properly irrigated the area, then notified a board-certified plastic and reconstructive surgeon who had completed a hand surgery fellowship. The same surgical technique was used for all patients. Before the procedure, the surgeon evaluated all amputations under a microscope or loupe to plan for microanastomosis. All amputated parts and digital stumps were cleaned and debrided under general anesthetic or brachial plexus/digital block. Under the microscope or loupe, debris and devitalized tissue were removed before composite grafting. Bleeding was meticulously controlled, after which the composite graft was placed using the amputated tip and sutured with 5-0 nylon sutures. The margin of the composite graft was accurately sutured with a simple or vertical mattress suture under loupe magnification. If the nail plate was present, it was temporarily removed to allow nail bed repair. After nail bed repair, the whole nail was placed back into the nail fold and sutured with 4-0 nylon.
Postoperative management
All patients were admitted for 7 days from the completion of the composite graft and treated with intravenous empirical antibiotics and prostaglandin E (alprostadil alpha-cyclodextrin). No ice was applied for cooling after the composite graft. The reattached fingertip was treated with antibiotic ointment (oxytetracycline hydrochloride and polymyxin B sulfate) and, in a non-traumatic procedure, was wrapped in non-adherent hydrocolloid dressing (Physiotulle; Coloplast, Peterborough, UK) to maintain a moist environment. For patients in the HBO2 group, the treatment was applied as soon as possible after surgery, with initial compression to 2.8 ATA and 100% O2 applied for 45 minutes. After 45 minutes at 2.8 ATA, the injuries were decompressed to 2.0 ATA within 5 minutes and given a 5-minute air break (no oxygen). After the air break, patients were treated at 2.0 ATA for 55 minutes, after which the protocol was terminated (Fig. 1).
Application of the HBO2 protocol
The hyperbaric oxygen (HBO2) treatment was applied with initial compression to 2.8 atmospheres absolute (ATA) and 100% O2 administered for 45 minutes. After 45 minutes at 2.8 ATA, injuries were decompressed to 2.0 ATA within 5 minutes and given a 5-minute air break (no oxygen). After the air break, patients were treated at 2.0 ATA for 55 minutes, after which the protocol was terminated. PT, patient; OPT, optional.
Definition of the outcome
After composite grafting, the surgeon assessed the outcomes over the course of 8 weeks. In each case, the outcome was categorized as either success or failure. A graft was defined as successful if it completely healed within 8 weeks (Fig. 2), while failure was defined as a lack of complete healing over that time period (Fig. 3). We also classified cases that could not be healed with secondary intention and required additional procedures, such as stump revision and flap surgery, as failure. We described the healing time as the time (in weeks) required for graft survival after surgery.

Example of success
(A) Preoperative photo of a patient who was injured in a lateral oblique pattern. (B) Immediate postoperative photo; a pale color was observed. (C) Two weeks after the operation, the fingertip had recovered to gain a pinkish color after revascularization was completed.
Example of failure
(A) Preoperative photo of a patient who was injured in a volar pattern. (B) Immediate postoperative photo; a pale color was observed, and the distal phalangeal bone fracture was fixed with K-wire. (C) Two weeks after the operation, total necrosis was observed. This case was judged as graft failure, as it required additional procedure(s) such as debridement.
Statistical analysis
A biomedical statistician analyzed the collected data. Proper statistical methods were determined according to the properties of the variables. Categorical variables were statistically analyzed using the chi-square test and the Fisher exact test, while continuous variables were statistically analyzed using the two-sample t-test. Since the normality assumption did not apply to healing time, a non-parametric test (the Wilcoxon signed-rank test) was used. A P-value of <0.05 was considered to indicate statistical significance. SAS 9.4 software (SAS Institute Inc., Cary, NC, USA) was used for the statistical analyses in this study.
RESULTS
Descriptive statistics for the two groups
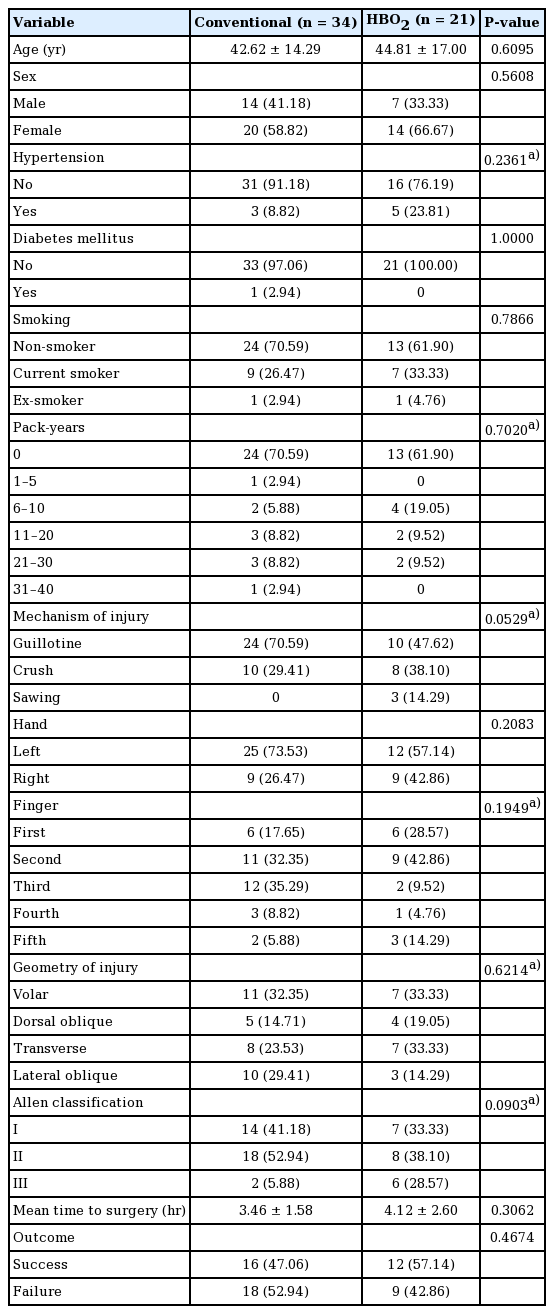
Among the 55 digits that we reviewed, 34 digits were conventionally treated, while 21 digits were treated with HBO2 (Table 1). The two groups had no statistically significant differences with regard to age, sex, hypertension, diabetes, or smoking history. The Allen classification and mean time to surgery similarly showed no significant differences between groups (Table 2). Fingertip injuries of the left hand were more frequent than those of the right side. The most frequently injured finger was the third (middle) finger in the conventional group and the second (index) finger in the HBO2 group. Regarding the injury geometry and mechanism, in both groups, volar oblique injuries were prevalent, and guillotine injuries were more frequent than crush injuries. The mean time from injury to composite graft was 3.46 hours in the conventional group and 4.12 hours in the HBO2 group, but this difference was not statistically significant.
Composite graft outcome analysis
The graft success rate was higher in the HBO2 group (57.1%) than in the conventional group (47.1%). However, no statistically significant difference was observed with regard to the overall graft success outcomes (Table 1). We analyzed the graft outcomes according to the mechanism of injury. Guillotine injuries were associated with a statistically significantly higher rate of success in the HBO2 group than in the conventional group (P= 0.0337), while crush injuries showed poor results in both groups (Table 3). Overall, within the HBO2 group, the time from injury to the first HBO2 treatment received and the total number of HBO2 sessions were not found to be statistically related to the outcome (Table 4).
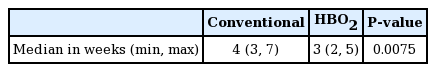
Healing time analysis
The HBO2 group had a shorter healing time than the conventional group, with median healing times of 3 weeks (range, 2–5 weeks) and 4 weeks (range, 3–7 weeks), respectively; this difference was statistically significant (P=0.0075) (Table 5).
DISCUSSION
In this study, we evaluated the clinical effect of HBO2 therapy on composite graft survival in cases of fingertip injury. Fifty-five fingertip injuries treated with composite grafting were included in the analysis. These composite graft cases included 28 cases of graft success (50.9%) and 27 cases of failure (49.1%). Age, sex, hypertension, diabetes mellitus, smoking history, the mechanism of the injury, and the geometry of the injury were reviewed as baseline characteristics. The conventional and HBO2 groups showed no statistically significant differences in these baseline characteristics.
HBO2 treatment involves the administration of a high concentration of oxygen in a high-pressure environment, with the patient breathing 100% oxygen at a pressure of 1.4 atmospheres or higher [19]. HBO2 can be applied at pressures of 2.0–3.0 ATA for periods of 1 to 4 hours. The arterial PO2 becomes elevated to 1,000–1,500 mmHg due to dissolved oxygen in the plasma. At the tissue and cellular levels, hyperoxygenation promotes angiogenesis and improves post-ischemic tissue survival. Increasing the applied pressure increases the PO2 of the tissue, which is beneficial for wound healing [20].
Most oxygen transported through the blood is carried in the form of oxyhemoglobin; specifically, 20 mL of oxygen is attached to hemoglobin per 100 mL of blood at standard atmospheric pressure. In contrast, only 0.3 mL of oxygen is dissolved in the plasma per 100 mL of blood. If the atmospheric pressure is raised to 3.0 atmospheres, the partial pressure of arterial oxygen reaches 2,200 mmHg. The dissolved plasma oxygen level increases from 0.3 mL to 5.4 mL, which is about 18 times the level at standard atmospheric pressure. This elevated partial pressure of oxygen can provide enough oxygen to maintain basal metabolic function without normal hemoglobin, which is the principle of HBO2 treatment [12].
In addition to hyperoxygenation, as a secondary mechanism, HBO2 promotes tissue regeneration and neovascularization in skin grafts and flaps [16]. The effect of HBO2 on skin grafts and flaps is thought to improve wound oxygen tension, fibroblast function (collagen synthesis), and vascularization [15]. Large amounts of animal data and multiple serials of clinical case reports have been published regarding the effectiveness of HBO2 in skin grafts, composite grafts, and flap ischemia. Even though many studies have discussed the efficacy of HBO2 in grafts and flaps, comparative clinical studies of HBO2 are rare, as it is challenging to collect identical cases to compare. Evaluating the effect of HBO2 alone is also difficult due to the challenges associated with obtaining patient consent to observe the flap or graft without additional adjunct therapy.
Before conducting the data analysis, we hypothesized that HBO2 would be effective in the treatment of fingertip injury. We also expected that HBO2 treatment would be more beneficial for crush injuries than for guillotine injuries. Generally, the survival of a composite graft after a crush injury is more difficult to attain [21]. Thus, we compared the success rate according to HBO2 treatment status for guillotine and crush injuries. For both the conventional and HBO2 groups, guillotine injuries were associated with a significantly higher proportion of successful outcomes than crush injuries (Table 3). The results also showed that HBO2 treatment increased the graft survival rate in patients with guillotine-type fingertip injuries. However, in the crush injury group, HBO2 therapy did not significantly affect graft outcomes. Considering the mechanism by which HBO2 increases graft survival by promoting angiogenesis caused by hyperoxygenation, we hypothesized that the crushed amputation was unsuitable for angiogenesis or neovascularization. Therefore, crush fingertip injuries treated with composite grafts do not appear to be an appropriate indication for HBO2 treatment.
Another outcome that we considered was healing time. The HBO2 group showed a median healing time of 3 weeks, while the median healing period for the conventional group was 4 weeks. This difference in healing time was statistically significant, with a statistical power (1–β) of 85.5%. The shorter healing time in the HBO2 group could be related to faster restoration of the function of the injured finger and a reduction in the number of clinic visits.
This study had a few limitations. First, it was retrospective in nature. The outcomes were reviewed only through images and the descriptions in the electrical medical records. Some data were missing, and not all information on necessary parameters could be obtained. Second, the statistical analysis was limited. This study included only patients from a short period, and information was collected from a single center representing only one region. To overcome the limitation of the small sample size, we collected the data consecutively. Lastly, during the study period, we only had one multiplace chamber, so we could not differentiate the HBO2 treatment protocol by indication; rather, we had to apply a single treatment protocol for every patient. Differences in the applied pressure and the number of HBO2 treatments per day may affect the wound survival outcome. Future studies may be used to develop an optimal treatment protocol.
HBO2 treatment effectively facilitates composite graft survival in guillotine-type fingertip injuries. HBO2 can also decrease the time required for the composite graft to heal. HBO2 therapy appears to increase survival rate and improve healing time in fingertip injuries treated with composite grafting, and it is considered to be adequate to perform in cases of guillotine injury, where the cutting surface is relatively clean. However, the effect may not be significant in cases of crush injury, so we expect that additional adjuvant therapy or another reconstruction plan will be required. Additionally, future randomized controlled trials with adequate sample sizes may be needed.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Wonju Severance Christian Hospital (IRB No. CR319010) and performed in accordance with the principles of the Declaration of Helsinki.
Patient consent
The patients provided written informed consent for the publication and the use of their images.
Author contribution
Conceptualization: J Kim. Data curation: JS Moon. Formal analysis: JS Moon. Methodology: JW Heo. Writing - original draft: Y Lee, JW Heo. Writing - review & editing: SW Kim.