Congenital Midline Cervical Cleft
Article information
The occurrence of congenital midline cervical cleft (CMCC) is very rare all over the world and has never been reported in Korea. The typical characteristic of CMCC is a longitudinal skin defect on the midline of the anterior neck that has a nipple-like skin tag at the cranial end, a fistula or sinus tract at the caudal end, and atrophic skin in between. It appears anywhere between the mandibular symphysis and the manubrium [1,2]. Surgical removal in early infancy is the choice of treatment in order to prevent neck extension disabilities caused by cicatricial neck contracture that may occur while aging. Complete excision of abnormal tissue and closure with single or multiple Z-plasty is usually required for functional and aesthetic purposes [1,2,3].
This report is about a 13-month-old female with the typical characteristics of CMCC, for whom we performed complete excision, platysmaplasty with Z-plasty, and skin closure with single Z-plasty.
The patient was a 13-month-old girl born by a full-term vaginal delivery and whose initial crying and other activities were normal. No other abnormal finding except a vertical skin defect in the anterior neck region was reported at birth or during growth. At our hospital, we clinically examined the skin lesion on the midline of the anterior neck, noting that it had a nipple-like skin tag at the cranial end, a fistula-like skin lesion at the caudal end, and atrophic skin in between them. Further, it showed a cervical tethering cord formed by the skin lesion (Fig. 1).
Neck magnetic resonance imaging and neck sonography showed a hypoechoic lesion in the subcutaneous layer of the midline of the anterior neck at the suprahyoid level with no definite evidence of a thyroglossal duct cyst or a fistula tract.
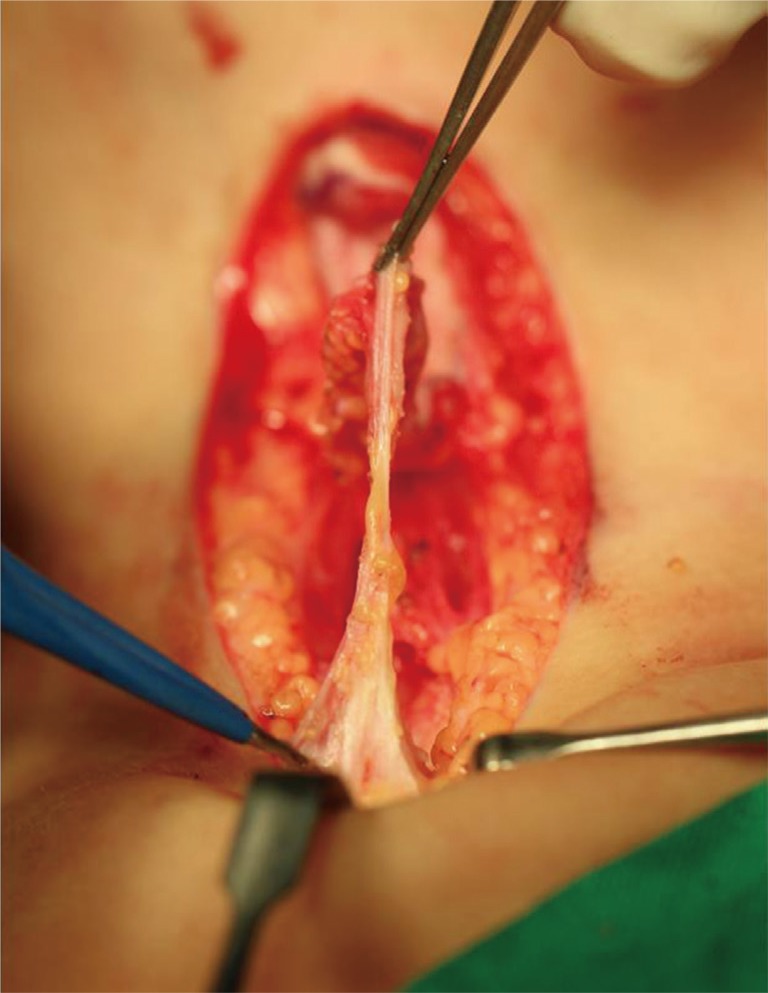
The patient clinically diagnosed with CMCC was placed on the operating table in a supine position under general anesthesia. A fistula opening at the caudal end was checked under the 0.5-cm-long blind end by testing with probe insertion. The cleft and the underlying band-like subcutaneous tissue were completely excised. The cranial end was loosely adhered to the mentalis muscle, and the caudal end was extended with band-like tissue near the manubrium (Fig. 2). After complete excision, platysma flap with Z-plasty and skin closure with single Z-plasty were performed (Figs. 3, 4).
The excised tissue was a 4.0 cm×1.1-cm tube-like tissue with a relatively smooth inner surface. Microscopically, the inner surface was covered with squamous epithelium with irregular thickness and parakeratosis. The subepithelial portion revealed a paucity of skin adnexal tissue and had haphazardly arranged skeletal muscle bundles mixed with fat tissue and seromucinous glandular tissue.
Minimal scarring was expected two months after the surgery (Fig. 5). No limitation of neck extension was expected upon long-term follow-up.
CMCC is very rare, and less than 100 cases of this condition have been reported worldwide. It is reported to occur sporadically, and girls have as high as twice the incidence rate as compared to boys [2,3].
The mechanism of CMCC has not yet been ascertained; however, embryologically defective fusion of the first and the second branchial arches is the most accepted hypothesis [1,2]. It is regarded as a variant of the Tessier median mandibular facial cleft and the type-30 craniofacial cleft [3]. Genetic studies are currently in progress; these studies focus on the mutation in the SIX5 gene and the deletion of the pregnancy-associated plasma protein A (PAPPA) as potential candidates, but an accurate mechanism is still unknown [4].
CMCC has three typical characteristics: 1) a nipple-like skin tag in the cranial portion, 2) a sinus tract or fistula in the caudal portion, and 3) a midline cleft resembling a skin defect in between. Subcutaneous band-like fibrosis usually appears above the platysma plane [1,2,3]. Other head and neck anomalies such as lower lip cleft, cleft tongue, cleft mandible, or hypoplasia of midline neck structures are known to be associated [1,2]. In this case, there are three typical characteristics of CMCC without any other anomalies.
The characteristic pathologic findings are reported as parakeratosis in the skin, the absence of skin appendages, the presence of striated muscle tissues under the skin, and the presence of respiratory epithelium or seromucinous glands [2,3,4]. In this case, the abovementioned histologic findings were conspicuous, but skin adnexal tissues were absent or very focally dispersed.
In the previously reported articles, complete excision of the cleft including the subcutaneous band and skin closure with Z-plasty (single or multiple) have been performed to prevent cicatricial neck contracture and the resulting limitation of neck motion [1,2,3]. In this report, in addition to the above treatment, we performed platysma flap with Z-plasty to prevent midline platysma banding and continuation of scar adhesion. This is expected to produce a functionally and aesthetically better prognosis [5].
Notes
No potential conflict of interest relevant to this article was reported.