Anterolateral thigh free flaps and radial forearm free flaps in head and neck reconstruction: A 20-year analysis from a single institution
Article information
Abstract
Background
Reconstruction after removal of a malignant tumor in the head and neck region is crucial for restoring tissue integrity, function, and aesthetics. We retrospectively analyzed patients who underwent intraoral reconstruction surgery using radial forearm free flaps (RFFF) and anterolateral thigh free flaps (ALT) at a single institution to provide more information supporting the choice of a reconstruction method after removal of head and neck cancer.
Methods
The charts of 708 patients who underwent head and neck reconstruction between 1998 and 2018 at the Department of Plastic and Reconstructive Surgery at our institution were retrospectively reviewed. Patients’ age, sex, and history of radiation therapy, diabetes mellitus, and smoking were retrieved. The primary cancer site, types of defects, and complications were investigated.
Results
Overall, 473 and 95 patients underwent reconstruction surgery with RFFF and ALT, respectively. RFFF was more often used in patients with cancers of the pharynx, larynx, esophagus, or tonsil, while ALT was more frequently used in patients with cancers of the mouth floor with tonsil or tongue involvement. The proportion of patients undergoing ALT increased gradually. Flap failure and donor site morbidities did not show significant differences between the two groups.
Conclusions
RFFF and ALT flaps resulted in similar outcomes in terms of flap survival and donor site morbidity. ALT can be an option for head and neck reconstruction surgery in patients with large and complex defects or for young patients who want to hide their donor site scars.
INTRODUCTION
Head and neck cancer is a common disease, with a reported crude incidence rate of 6.9 per 100,000 and mortality rate of 2.4 per 100,000 in Korea in 2016 [1]. Advanced disease is found in two-thirds of patients with squamous cell carcinoma of the head and neck upon presentation [2], and the resection of malignant tumors can result in large and complex defects. Covering these defects is crucial for restoring tissue integrity, function, and aesthetics.
Considering the size, location, and shape of the defects, microsurgical free tissue transfer has emerged as the method of choice for head and neck reconstruction [3].
The radial forearm free flap (RFFF) was first described in 1947 by Longmire [4]. The first case where RFFF was used in the oral cavity was reported in 1976 by Panje et al. [5]. For small defects such as a hemi-tongue, patients who underwent reconstruction using RFFF showed better scores in the retraction, swallowing, chewing, and speech domains [6]. The advantages of RFFF include its thinness, versatility, and long constant pedicle of a large caliber. However, the flap is limited in size and leaves a visible scar, in addition to scar contracture on the forearm in some cases. In contrast, the anterolateral thigh free flap (ALT) was first introduced in 1983 by Baek [7]. Since then, the ALT has been used in various regions such as the upper and lower extremities and the trunk [8]. In addition to other sites, Koshima et al. [9] reported 22 cases of head and neck reconstruction with ALT. Demirkan et al. [10] reported using ALT for head and neck reconstruction in 59 cases. Even though ALT has variations in its vascular pedicle [11], it is easy to harvest and produces optimal results at both the donor site and at the recipient site, thereby providing an ideal reconstructive option [12].
The purpose of this study was to retrospectively analyze intraoral reconstruction surgery using RFFF and ALT at a single institution. The patients’ demographics, primary cancer site, and defect type were investigated. By comparing the indications and the number of cases or surgical complications between the two types of flaps, we hope to provide further information to surgeons who are deciding on a reconstruction modality for defects of the head and neck.
METHODS
A retrospective review was conducted of the charts of 708 patients who underwent head and neck reconstruction between 1998 and 2018 at the Department of Plastic and Reconstructive Surgery, Severance Hospital, Yonsei University, Seoul, Korea. This study was approved by the Institutional Review Board of Severance Hospital (IRB No. 4-2020-0448).
All reconstruction methods used for head and neck reconstruction between 1998 and 2018 at our institution were investigated. Only primary surgery was included. Data regarding age, sex, and history of radiation therapy, diabetes mellitus, and smoking were retrieved for patients who underwent head and neck reconstruction surgery with RFFF and ALT. The t-test and chi-square test were used to investigate whether there were statistically significant differences in the variables between the two groups. The primary malignant tumor location was investigated and classified as the maxilla or mandible; larynx or esophagus; pharynx; tonsil; and mouth floor, buccal mucosa, or tongue. The distribution of primary cancer sites was compared to determine whether there was a preference for a specific type of flap for a specific cancer site. In addition, oropharyngeal defects were classified into six zones, as reported previously [13]. Zone 1 defects only involved the mouth floor or buccal mucosa; zone 2 defects affected the tongue; zone 3 defects involved the mouth floor and part of the tongue; zone 4 defects involved the mouth floor, part of the tongue, and tonsil; zone 5 defects involved the mouth floor, part of the tongue, tonsil, and soft palate; and zone 6 defects involved the pharyngeal wall. The distribution of defect types was also compared between the two groups to verify the tendency for a certain type of flap to be chosen for a certain type of defect. The investigation period was divided into four intervals of 4–5 years each. The total number of cases of head and neck reconstruction with RFFF and ALT was counted. The ratio of reconstructions using RFFF and ALT was investigated to determine whether there was a specific trend in the choice of reconstruction modality. All perioperative complications related to the reconstruction surgery were retrieved and compared. Univariate statistical analysis was performed using the chi-square test, Fisher exact test, and t-test. The Mantel-Haenszel chi-square test was performed to analyze chronological trends. In the interpretation of results, P-values <0.05 were considered to indicate statistical significance. Statistical analyses were performed using SPSS version 25 (IBM Corp., Armonk, NY, USA).
RESULTS
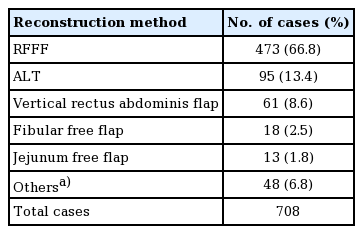
A total of 708 head and neck reconstructions were performed between 1998 and 2018 (Table 1). The most common method of reconstruction was RFFF, which was performed in 473 patients (66.8%). Additionally, 95 patients (13.4%) underwent reconstruction with an ALT, 61 patients (8.6%) with a vertical rectus abdominis muscle flap, 18 patients (2.5%) with a fibular free flap, and 13 patients (1.8%) with a jejunum free flap.
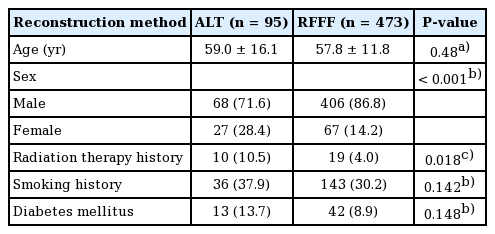
The demographics of the two groups were also compared (Table 2). The proportion of patients with a history of radiation therapy was higher in the ALT group than in the RFFF group (10.5% vs. 4.0%) The sex distribution was different between the two groups: the proportion of women was higher in the ALT group than in the RFFF group (28.4% vs. 14.2%). Other variables such as age, history of diabetes mellitus, or history of smoking did not show statistically significant differences between the two groups.
The primary cancer site was investigated in both groups (Table 3). RFFF was used more often in patients with cancers of the pharynx (14.2%), larynx and esophagus (14.8%), or tonsil (21.8%), while ALT was used more frequently in patients with cancers of the mouth floor and buccal mucosa (25.3%) or tongue (40%). Cancers of the tongue or mouth floor and buccal mucosa usually leave large and complicated defects that require complex-shaped microsurgical free tissue transfer for reconstruction.
Since the tongue was the most common primary cancer site in both groups (40% and 31.3%, respectively), a subgroup analysis was performed. The age distribution was compared between the two groups. The proportion of patients aged between 20 and 49 was higher in the ALT group than in the RFFF group (18.4% vs. 5.4%, respectively) (Table 4).
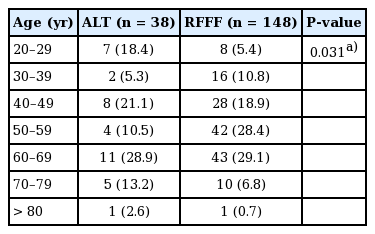
Comparison of the age distribution of patients with primary cancer of the tongue between the two groups
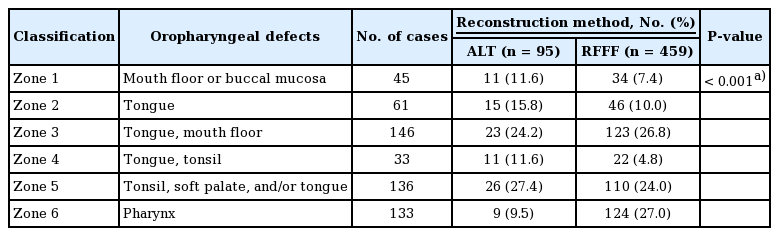
The oropharyngeal defect types after removal of the primary cancer were also compared between the two groups (Table 5). The distribution of defects between the two groups was statistically significantly different (P<0.001). ALT was more often used for relatively large defects in zone 2 (tongue), zone 4 (tongue and tonsil), and zone 5 (tonsil and soft palate or tongue), while RFFF was used more frequently for defects in zone 6 (pharynx).
The investigation period between 1998 and 2018 was divided into four intervals. The total number of patients who underwent reconstructive surgery with ALT and RFFF, as well as the ratio of the number of ALT cases to the number of RFF cases, were investigated (Table 6). The ratio of the number of ALT cases to RFFF cases increased gradually (P<0.001). In addition, the total number of ALT cases steadily increased over time. Between 2014 and 2018, the total number of reconstructions with RFFF and ALT (41 cases) decreased dramatically compared with the earlier period (between 2009 and 2013; 159 cases).

Total number of cases and changes in the ratio of number of cases of RFFF and ALT for each time period
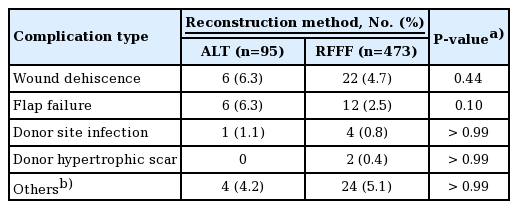
Finally, all perioperative complications related to reconstruction surgery were investigated (Table 7). The flap failure rate was not significantly different between the two groups (6.3% vs. 2.5%, P=0.10). The rates of donor site morbidities such as wound dehiscence (6.3% vs. 4.7%, P=0.44), infection (1.1% vs. 0.8%, P>0.99), or hypertrophic scarring (0% vs. 0.4%, P>0.99) were similar in both groups. Other complications, such as fistula, flap bulkiness, and submental abscess, did not show statistically significant differences between the two groups.
DISCUSSION
Reconstruction surgery after resection of a malignant tumor in the head and neck region is challenging and has a higher rate of flap failure and complications than reconstruction procedures in other locations. The selection of an appropriate flap considering the restoration of integrity, form, and function is a crucial aspect of obtaining optimal long-term outcomes [14]. Wei et al. [8] reported 672 cases of ALT for reconstruction of the head and neck, upper extremity, lower extremity, and trunk and suggested that ALT is a versatile soft tissue flap, the thickness and volume of which can be adjusted based on the extent of the defect. In our study, the ratio of reconstructions with ALT to RFFF increased gradually. This occurred due to a better understanding of the versatile indications and advantages of ALT. In addition, the total number of reconstructions decreased dramatically between 2014 and 2018. This change took place because one of the surgeons in the Otolaryngology Department started performing head and neck reconstruction surgery.
During the past 20 years, ALT was used in various sites to repair oropharyngeal defects. Tongue and tonsil cancers accounted for more than half of the cases; these are characterized by complicated defects, including defects of the mouth floor and soft palate (zones 4 or 5), making it difficult to select and design flaps. As ALT can provide soft tissue with sufficient volume and in versatile shapes, it was used often for relatively large defects, such as those in zone 4 (tongue and tonsil).
RFFF has the advantages of thinness, pliability, reliability of survival, and a long pedicle. For this reason, RFFF is useful option for covering a flat or cylindrical shape. The results of our study are consistent with these points, as RFFF was more often used in reconstruction of the pharyngeal wall, esophagus, or larynx, which are sites that require a thin and plastic flap for reconstruction.
The most important goal of reconstruction surgery is to cover the defect and to restore tissue integrity and function, if possible. In addition to the stable integration of a microsurgical free tissue transfer to the defect site, donor site morbidity is another aspect that surgeons should consider to enhance patients’ quality of life after surgery. Even though the use of an acellular dermal matrix in a forearm defect after RFFF harvest can improve skin elasticity and moisture [15], it still leaves a conspicuous scar that is visible on the forearm. Furthermore, split-thickness skin grafts from the forearm can result in restriction of range of motion and disability because dense scars form on the skin and graft–tendon adhesions may develop [16]. Aggressive hand therapy or ablative fractional resurfacing with a laser can improve scarring, but the scar is still visible and can affect the quality of life, especially in young patients. In contrast, primary repair of the donor site is usually possible with ALT, and the scar can be hidden under one’s clothes. Huang et al. [17] compared donor site morbidity in 41 patients who underwent tongue reconstruction with RFFF and a thinned anterolateral thigh cutaneous flap. They concluded that RFFF resulted in a conspicuous, unattractive scar with pain, numbness, and sacrifice of a radial artery, while most reconstructive procedures with ALT resulted in only a linear scar without loss of function. At our institution, the ALT group had a higher proportion of patients who received reconstruction of the tongue and whose age was between 20 and 49 years. Although the absolute number of patients who underwent tongue reconstruction with RFFF exceeded the number of patients who underwent tongue reconstruction with ALT, differences in the proportion of ages might reflect a preference for choosing ALT in young patients.
With respect to donor site morbidity, one report concluded that the incidence of wound dehiscence was lower in patients who underwent reconstructive surgery with ALT than with RFFF [18]. Hanasono et al. [19] reported relatively low incidence rates of donor site morbidity in patients who underwent reconstructive surgery with ALT (seroma, 5%; wound dehiscence, 2%; hematoma, 1%; infection, 1%; and neuroma, 1%). Townley et al. [20] reported reduced sensitivity at the donor site in patients who underwent reconstructive surgery with ALT, but pathogenic scars were rare and the contractile function of the quadriceps was intact. In this study, there was no statistically significant difference in the flap failure rate or donor site-related complications between the ALT and RFFF groups.
The strengths of this study include the large size of the groups and the long duration of the study (20 years). There have been similar reports regarding the comparison between RFFF and ALT; however, few studies had such large patient cohorts or long study periods. Furthermore, a subgroup analysis was performed in the tongue reconstruction group by age. This study also had a few limitations. First, the ratio of patients who received radiation therapy was significantly different between the two groups. In addition, information on perioperative transfusions and operative time could not be retrieved.
To conclude, RFFF is a useful modality for the reconstruction of flat or cylindrical-shaped defects, while ALT can be considered as another option in head and neck reconstruction surgery since its flap failure rate and complication rate are similar to those of RFFF. However, ALT has the advantage of causing minimal scarring and functional impairment.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Severance Hospital (IRB No.4-2020-0448) and performed in accordance with the principles of the Declaration of Helsinki. Informed consent from participants was waived.
Author contribution
Conceptualization: JW Hong, WJ Lee. Data curation: S Yang, JW Hong, IS Yoon, DH Lew, TS Roh. Formal analysis: S Yang, IS Yoon, WJ Lee. Project administration: DH Lew, TS Roh, WJ Lee. Writing - original draft: S Yang. Writing - review & editing: WJ Lee.