Nasal airway function after Le Fort I osteotomy with maxillary impaction: A prospective study using the Nasal Obstruction Symptom Evaluation scale
Article information
Abstract
Background
This study evaluated changes in nasal airway function following Le Fort I osteotomy with maxillary impaction according to the Nasal Obstruction Symptom Evaluation (NOSE) scale.
Methods
This cohort study included 13 patients who underwent Le Fort I osteotomy with maxillary impaction. Nasal airway function was evaluated based on the NOSE scale preoperatively and at 3 months postoperatively. The change in the NOSE score was calculated as the preoperative score minus the postoperative score. If the normality assumptions for changes in the NOSE score were not met, a nonparametric test (the Wilcoxon signed-rank test) was used. Differences in NOSE score changes according to patient characteristics and surgical factors were evaluated using the Kruskal-Wallis test and the Mann-Whitney test.
Results
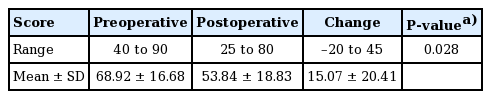
Patients ranged in age from 18 to 29 years (mean±standard deviation [SD], 23.00±3.87 years). Three were men and 10 were women. Eleven patients (84%) had an acquired dentofacial deformity with skeletal class III malocclusion. The preoperative NOSE scores ranged from 40 to 90 (mean±SD, 68.92±16.68), and the postoperative NOSE scores ranged from 25 to 80 (53.84±18.83). The cohort as a whole showed significant improvement in nasal airway function following maxillary impaction (P=0.028). Eleven patients (84%) had either improved (n=8) or unchanged (n=3) postoperative NOSE scores. However, nasal airway function deteriorated in two patients. Patient characteristics and surgical factors were not correlated with preoperative or postoperative NOSE scores.
Conclusions
Nasal airway function as evaluated using the NOSE scale improved after maxillary impaction.
INTRODUCTION
Orthognathic surgery is a common elective procedure for improving facial function (occlusion, mastication, speech) and aesthetics. Le Fort I osteotomy is a popular technique for this type of surgery, as it allows the maxilla to be moved in any direction required for the purpose of the operation. However, in certain cases, such as total impaction where the maxilla is moved as a whole, or posterior impaction where it is rotated clockwise, the operation can result in narrowing of the nasal airways, sometimes causing interference between the inferior turbinate and nasal floor. In addition, superior movement of the maxilla may cause a proportional decrease in nasal airflow due to an increase in the resistance of the nasal airway as the intranasal dimension decreases.
Several studies have evaluated changes in nasal airway function following maxillary mobilization using objective methods such as acoustic rhinometry and anterior rhinomanometry [1-3]. In addition, it was found that even when maxillary impaction was conducted, there was no nasal airway compromise in most cases [3,4].
However, these methods tend to give results that are poorly correlated with subjective symptoms; furthermore, they are unable to detect functional nasal airway obstruction in a considerable proportion of patients [5,6]. In view of this, Stewart et al. [7] developed the Nasal Obstruction Symptom Evaluation (NOSE) scale for evaluating subjective symptoms reported by patients. The scale has been shown to be a valid disease-specific measure of quality of life for evaluating nasal airway obstruction [6-8].
This prospective study used the NOSE scale to evaluate changes in nasal airway function following maxillary impaction performed using Le Fort I osteotomy.
METHODS
Patient selection and data collection
This study included patients who underwent maxillary impaction by Le Fort I osteotomy at our craniofacial surgery center between September 2017 and February 2020. Patients were excluded if they had previously undergone partial inferior turbinectomy, used a nasal inhaler (which can affect the thickness of the nasal mucosa), had polyps or a nasal skeletal deformity, had adenoid hyperplasia or turbinate enlargement, or had developed an acute upper respiratory infection within 4 weeks after enrollment. Data were collected on patients’ age, sex, body mass index (BMI), and smoking status; the condition to be surgically corrected and the class of occlusion; the presence of relevant comorbidities, such as asthma, obstructive sleep apnea, or allergic rhinitis; and whether complications arose, either during orthognathic surgery or postoperatively due to inferior turbinectomy. The types of orthognathic surgical procedures performed, the degree and direction of maxillary movement, and whether inferior turbinectomy was performed were also noted.
All the surgical procedures were performed by a single surgeon (JHC). Before each operation, the surgeon established surgical treatment objectives via thorough analytic model surgery in consultation with experienced orthodontists. We essentially followed McNamara analysis for diagnosis and presurgical planning, but we always considered the soft tissue profile and upper airway, and in some cases, modifications were needed. In addition, we tried to make the angle of the Frankfort horizontal plane to the A-B plane between 81° and 83° because we believe this range corresponds to the class I facial profile. Coronal computed tomographic scans and cephalometric radiographs (panoramic, lateral, and posteroanterior) were taken 2 weeks before surgery. The preoperative coronal scans were used to measure the distance between nasal floor and inferior turbinate on each side of the nose (mucosa to mucosa at the level of the maxillary first molar), and the lower of the two values was used to help estimate the expected postoperative narrowing of the nasal airways and the risk of interference between the two aforementioned structures. If, during planning, this distance was found to be less than or equal to the degree of maxillary impaction required for correction of canting (calculated using mean values for both sides of the face), inferior turbinectomy was performed to resolve the expected interference. Moreover, in order to prevent the development of nasal septal deviation during maxillary impaction and to exclude its effects on the nasal airway, we only conducted resection and removal of the septum (cartilage and bone) to the extent that no physical interference occurred during maxillary impaction.
Surgical technique
Le Fort I osteotomy was performed according to conventional protocol. A mucosal incision was made and subperiosteal dissection was performed around the pyriform aperture, followed by subperiosteal elevation. After full elevation and protection of the maxillary periosteum, osteotomy was performed with a reciprocating saw and a straight osteotome.
Prior to maxillary osteotomy, careful dissection was performed between the nasal mucosa and maxilla. Down-fracture and full mobilization of the maxilla were performed, with the nasal mucosa being preserved intact. If necessary, inferior turbinectomy was conducted after maxillary mobilization to prevent interference that might result from the distance between nasal floor and inferior turbinate being less than or equal to the degree of maxillary impaction. A bilateral linear incision was made at the nasal floor mucosa to expose the turbinate. Both the mucosa and turbinate bone were resected. The turbinate tissue, including bone, was clamped with straight Kelly forceps, and the mucosa and bone were excised together with Mayo scissors (Fig. 1). After resection, hemostasis was performed with electrocautery and wound repair was completed. For the nasal septum, as described above, the cartilaginous and bony septum were resected only to the extent that there was no physical interference with the movement of the maxilla.
Inferior turbinectomy during the maxillary impaction
(A) Inferior turbinectomy after down-fracture of the maxilla. Inferior turbinectomy was conducted to prevent interference, which might occur if the distance between nasal floor and inferior turbinate was less than the degree of maxillary impaction. (B) Resected inferior turbinate tissue including bone. The turbinate tissue including bone was clamped with straight Kelly forceps, and the mucosa and bone were excised together with Mayo scissors. Rt, right; Lt, left.
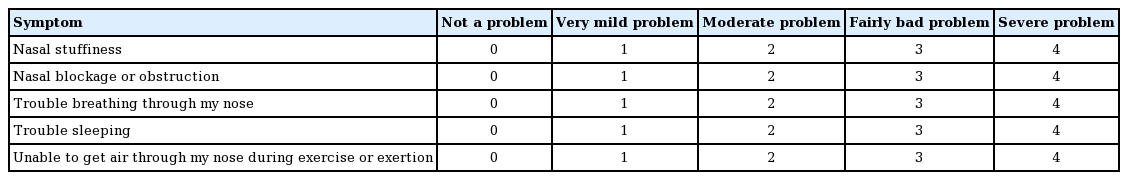
NOSE scale
The NOSE scale is a simple questionnaire utilized to evaluate nasal airway function. It comprises five self-assessment questions with potential answers ranging from 0 (not a problem) to 4 (severe problem); the maximum score is 20 (Table 1). The patients in our study answered the NOSE scale preoperatively and 3 months postoperatively. Raw scores were multiplied by 5 to convert them to weighted scores (0–100), with higher scores indicating more severe nasal airway obstruction. To reduce bias, all patients were interviewed by the same investigator, who was not an operating surgeon. The change in the NOSE score was calculated as the preoperative score minus the postoperative score, and was used as a measure of improvement in nasal airway function.
The Kolmogorov-Smirnov and Shapiro-Wilk tests were used to evaluate the normality assumption for changes in the NOSE score. If the normality assumption was confirmed, the significance of the change was analyzed with the paired t-test. If the normality assumptions were not met, a nonparametric test (the Wilcoxon signed-rank test) was used. Differences in NOSE score changes with regard to patient characteristics and surgical factors were evaluated using the Kruskal-Wallis test and the Mann-Whitney test. A P-value <0.05 was considered to indicate statistical significance. In addition, a statistical analysis was performed to exclude the effects of the type of surgical procedure (inferior turbinectomy or genioplasty) on NOSE score changes. The Mann-Whitney test was used to evaluate whether the NOSE score change differed significantly according to whether inferior turbinectomy or genioplasty was performed.
All data were analyzed using SPSS version 21.0 for Windows (IBM Corp., Armonk, NY, USA). This study was conducted in accordance with the Declaration of Helsinki. All patients were provided with a description of the study prior to surgery, and informed consent was obtained for inclusion in the study. Myongji Hospital Institutional Review Board reviewed the protocol and approved this study (IRB number: MJH2020-05-007).
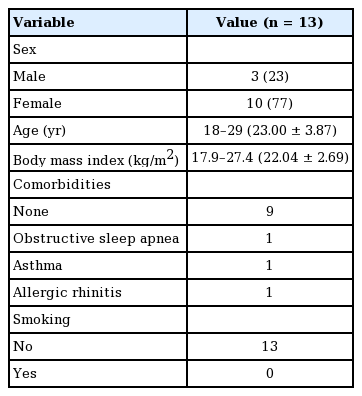
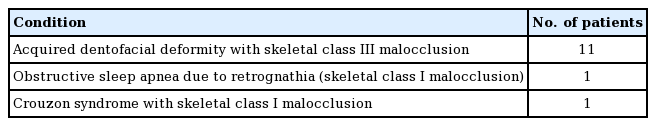
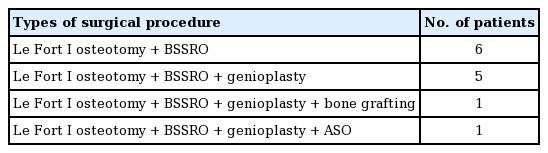
RESULTS
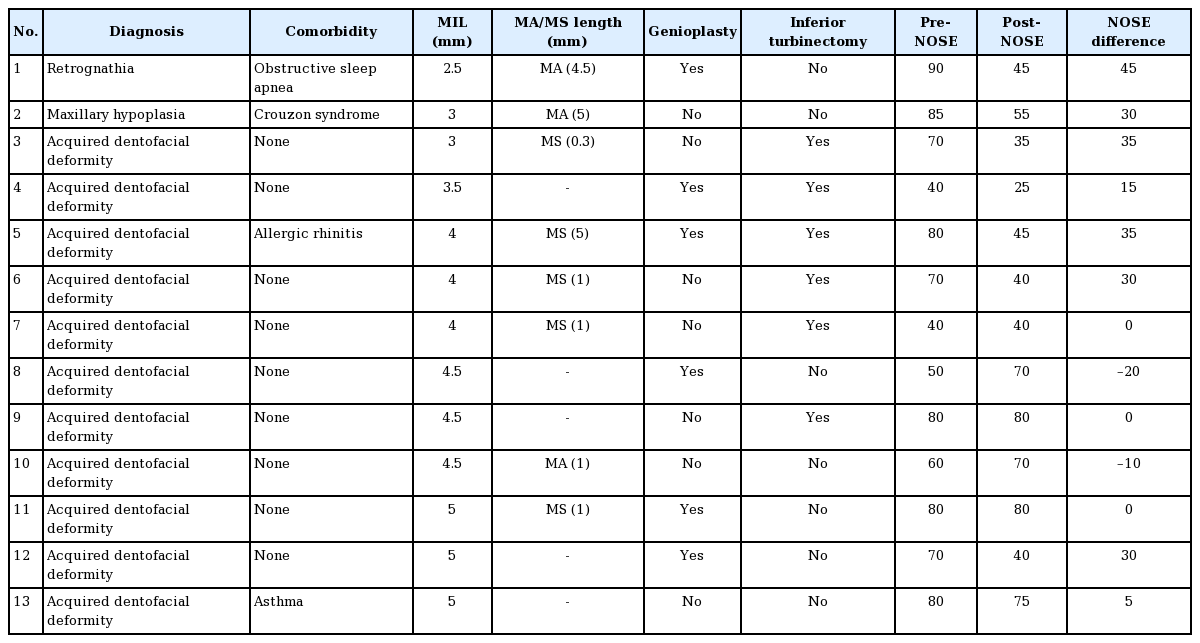
In total, 13 patients met the selection criteria. Patients’ age ranged from 18 to 29 years (mean±standard deviation [SD], 23.00±3.87 years). Three (23%) were men, and 10 (77%) were women. Their BMI ranged from 17.9 to 27.4 kg/m2 (mean± SD, 22.04±2.69 kg/m2). Comorbidities included allergic rhinitis (n=1), asthma (n=1), and obstructive sleep apnea (n=1) (Table 2). For 11 patients (84%), the condition to be corrected by surgery was acquired dentofacial deformity with skeletal class III malocclusion, while one patient (8%) had obstructive sleep apnea with retrognathia, and one patient (8%) had Crouzon syndrome (Table 3). All patients underwent Le Fort I osteotomy and bilateral sagittal split ramus osteotomy of the mandible. For six patients, these were the only orthognathic procedures performed; the other patients underwent additional procedures such as genioplasty, bone grafting, and anterior segmental osteotomy of the maxilla (Table 4).
With regard to anteroposterior repositioning of the maxilla, maxillary setback was performed in five patients (38%; range, 0.3–5.0 mm; mean±SD, 1.66±1.89 mm) and maxillary advancement in three patients (23%; range, 1.0–4.5 mm; mean± SD, 3.50±2.17 mm); the other five patients (38%) had neither.
In six patients (46%), the distance between nasal floor and inferior turbinate (range, 2.5–5.0 mm; mean±SD, 4.03±0.82 mm) was less than or equal to the degree of maxillary impaction (range, 2.3–7.1 mm; mean±SD, 4.78±1.72 mm), and they underwent inferior turbinectomy to resolve the interference (Fig. 2).
Preoperative and postoperative computed tomography scans
Preoperative (A) and postoperative (B) coronal views show the reduced turbinates (blue arrows) and maintained nasal airway. The patency of the nasal airway was maintained by performing inferior turbinectomy to prevent physical interference between the inferior turbinate and palatal bone.
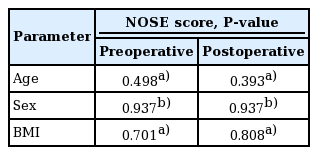
The preoperative weighted NOSE scores ranged from 40 to 90 (mean±SD, 68.92±16.68), while the postoperative weighted NOSE scores ranged from 25 to 80 (mean±SD, 53.84±18.83). After maxillary impaction, the cohort as a whole showed significant improvement in nasal airway function (P=0.028 using the Wilcoxon signed-rank test) (Table 5), with the change in weighted NOSE score difference ranging from –20 to 45 (mean±SD, 15.07±20.41). Eleven patients (84%) had either a lower NOSE score after surgery (n=8) or no change (n=3). However, nasal airway function deteriorated after surgery, as shown by higher weighted NOSE scores after surgery; one patient’s score rose by 10, and the other’s by 20. Most parameters we examined, including age, sex, and BMI, were not correlated with preoperative or postoperative NOSE scores (Table 6). A statistical analysis of the effects of surgical procedures, including inferior turbinectomy and genioplasty, on NOSE score changes showed no statistically significant results (inferior turbinectomy: P=0.534, genioplasty: P=0.445 using the Mann-Whitney test). Detailed data for all patients are presented in Table 7.
DISCUSSION
In this study, we used the NOSE scale to evaluate changes in nasal airway function following maxillary impaction. Previous studies in this field have evaluated these changes using objective methods such as acoustic rhinometry and anterior rhinomanometry, finding that maxillary impaction was associated with improvements in nasal airway resistance and flow [1-3]. In a cohort study of 52 patients who underwent maxillary impaction, almost three-fourths showed reduced nasal airway resistance and unchanged or improved airflow [3]. Nevertheless, because the results obtained using these objective methods are poorly correlated with patients’ subjective symptoms, we hypothesized that using the NOSE scale would reveal worsened nasal airway function after maxillary impaction. However, contrary to our expectations, the NOSE scale gave results consistent with those given by the objective methods, with patients generally having improved or stable nasal airway function after maxillary impaction.
Maxillary mobilization by Le Fort I osteotomy is commonly used to correct congenital or acquired dentofacial deformities, and many studies have been published on its effects on nasal airway function. Haarmann et al. [9] studied patients who underwent Le Fort I osteotomy with concomitant nasal surgery (resection of the inferior turbinate, contouring of the pyriform aperture, correction of the nasal septum) and found that nasal airway function improved regardless of whether maxillary positioning was advanced, inferior, or impacted. Like most studies before ours, Haarmann et al. [9] used acoustic rhinometry and anterior rhinomanometry as tools for evaluating changes in nasal airway function and structure; specifically, the cross-sectional area of the nasal cavity, airflow, and nasal airway resistance were measured using these objective methods. However, these measures do not correlate well with subjective symptoms of nasal obstruction reported by patients [6,7]. Williams et al. [10] used the NOSE scale to evaluate nasal airway function before and after maxillary surgery in 50 patients, of whom 92% had maxillary advancement (median, 4 mm; interquartile range, 3–5 mm); of these patients, 80% had unchanged or improved NOSE scores without additional nasal surgery. In our study of patients who underwent maxillary impaction, 84% of patients had unchanged or improved NOSE scores, consistent with Williams et al.
Le Fort I osteotomy allows the maxilla to be repositioned in any direction, and when the bone is repositioned, it affects the adjacent soft tissue [11]. Reduced resistance and increased flow in the nasal airway after maxillary movement are due in large part to the nasal valve area, which is bounded by the floor of the nose, the soft fibro-fatty tissue covering the pyriform aperture, the caudal ends of the lateral cartilage, and the nasal septum. This teardrop-shaped area is the narrowest part of the nasal passage; thus, it accounts for a large portion of airflow resistance, and even small changes in its volume cause large changes in airflow [12,13]. After maxillary repositioning, the structure of the external nose also changes in a way favorable to nasal airflow. Acoustic rhinometry has shown that the base of the nasal valve becomes wider as the alar base width increases, with airway resistance decreasing and flow increasing due to the opening effect [10]. Applying an alar cinch suture before maxillary wound repair can also contribute to increased flow by changing the shape of the external nares from slit to ovoid [14]. These facts help explain our findings that nasal airway function improved in patients with maxillary impaction.
In maxillary impaction, physical interference may occur between the palatal bone and the inferior turbinate and internal nasal septum. This is corrected through additional procedures such as inferior turbinectomy and septoplasty, which may also increase nasal airflow [9]. Approximately 80% of nasal airflow passes around the inferior turbinates, which filter, warm, and humidify the nasal airway. Inferior turbinectomy can change the entire nasal flow pattern, resulting in better ventilation of the nasal cavity [15]. Several studies have been conducted on the benefits of simultaneous maxillary surgery and nasal surgery. In 2016, Posnick et al. [16] evaluated 262 patients simultaneously undergoing maxillary surgery and intranasal procedures (such as septoplasty and volume reduction of the inferior turbinate) and found not only a significant benefit in alleviating chronic obstruction symptoms but also a minimal complication rate, with a mean reduction of 57 points in weighted NOSE scores. However, in our study, no statistically significant difference was found in NOSE score changes depending on whether or not inferior turbinectomy was performed. This is not consistent with the results of the study by Posnick et al. We believe that inferior turbinectomy may aid nasal airway patency in patients undergoing maxillary impaction. In addition, the authors believe that further studies are needed to investigate the usefulness of routinely performing inferior turbinectomy to improve nasal airway function when maxillary impaction is conducted in patients with high preoperative NOSE scores.
A rare complication of inferior turbinectomy is empty nose syndrome, which can result from excessive turbinate tissue resection. Empty nose syndrome is associated with decreased regrowth of the sensory nerves, and patients complain of difficulty breathing despite the absence of any prominent obstruction of the nasal airway [17]. Excessive turbinate tissue resection may also result in intraoperative or postoperative heavy bleeding and chronic nasal crusting [18]. In this study, no complications due to turbinectomy were observed during the postoperative follow-up period, which is consistent with previous studies [16-18].
In the Wisconsin Sleep Cohort Study, Young et al. [19,20] reported that nasal congestion was associated with both habitual snoring and obstructive sleep apnea. Orthognathic surgery has proven useful in the surgical treatment of obstructive sleep apnea, and the fact that our patient with obstructive sleep apnea had a NOSE score improvement of 45 points after surgery would seem to validate the effectiveness of this procedure.
The close association between chronic nasal obstruction and maxillary growth has been studied since the early 1900s. Chronic nasal obstruction and lack of nasal breathing are known to adversely affect dentofacial and craniofacial development. As the tongue and mandibles are located at a lower position due to mouth breathing, the tone of the facial muscles decreases, and nasal airflow decreases due to the anatomical obstruction [21,22]. Common physical characteristics in individuals with obstructed nasal airways, such as a narrow and posteriorly positioned mandible and a hypoplastic maxilla associated with an open bite, may be a result of this disordered breathing and the abnormal tone and stimulation of facial muscles [23,24]. McNamara [25] proposed physiological mechanisms for the link between upper respiratory tract obstruction and associated neuromuscular abnormalities of the bone, soft tissue, and craniofacial and dental structures. These observations are supported by our study, in which 84% of patients had skeletal class III malocclusion, and the mean preoperative NOSE score was poor (68.92±16.68).
As this study involved relatively few patients, our results may have limited generalizability to clinical practice. Nevertheless, this is the first study that used the NOSE scale to evaluate nasal airway function preoperatively and postoperatively in patients who underwent orthognathic surgery with maxillary impaction.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Myongji Hospital (IRB No. MJH2020-05-007) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.
Author contribution
Conceptualization: all authors. Data curation: HS Kim, JH Son, JH Chung. Formal analysis: HS Kim, JH Son. Methodology: HS Kim, JH Son. Project administration: HS Kim, JH Son. Visualization: HS Kim, JH Son, JH Chung, J Choi, JY Yang. Writing - original draft: HS Kim, JH Son, KS Kim. Writing - review & editing: all authors.