Early wound healing of the hard-palate mucosal harvest site using artificial dermis fixation by a transparent plate
Article information
Abstract
Background
There are currently no guidelines for the postoperative wound management of the hard-palate donor site in cases involving mucosal harvesting. This study describes our experiences with the use of an artificial dermis for early epithelialization and transparent plate fixation in cases involving hard-palate mucosal harvesting.
Methods
A transparent palatal plate was custom-fabricated using a thermoplastic resin board. After mucosal harvesting, an alginic acid-containing wound dressing (Sorbsan) was applied to the donor site, which was then covered with the plate. After confirming hemostasis, the dressing was changed to artificial dermis a few days later, and the plate was fixed to the artificial dermis. The size of the mucosal defect ranged from 8×25 to 20×40 mm.
Results
Plate fixation was adequate, with no postoperative slippage or infection of the artificial dermis. There was no pain at the harvest site, but a slight sense of incongruity during eating was reported. Although the fabrication and application of the palatal plate required extra steps before and after harvesting, the combination of the artificial dermis and palatal plate was found to be very useful for protecting the mucosal harvest site, and resulted in decreased pain and earlier epithelialization.
Conclusions
The combination of artificial dermis and a transparent palatal plate for wound management at the hard-palate mucosal donor site resolved some of the limitations of conventional methods.
INTRODUCTION
The hard palate mucosa is used for reconstruction of the mucosal side of the eyelids. However, there is no consensus regarding postoperative wound management of the donor site. As direct closure of the harvest site is impossible in almost all cases, secondary treatment is necessary for wound management in the presence of persisting symptoms, such as postoperative bleeding and pain with oral intake. To overcome these problems, some previous studies reported the use of obturators to protect the donor site [1,2]. However, we encountered a case in which only a plate was used, thereby requiring long-term epithelialization. Therefore, we aimed to describe our proposed combined technique of using both a transparent plate and artificial dermis, along with details of representative cases.
METHODS
Patients
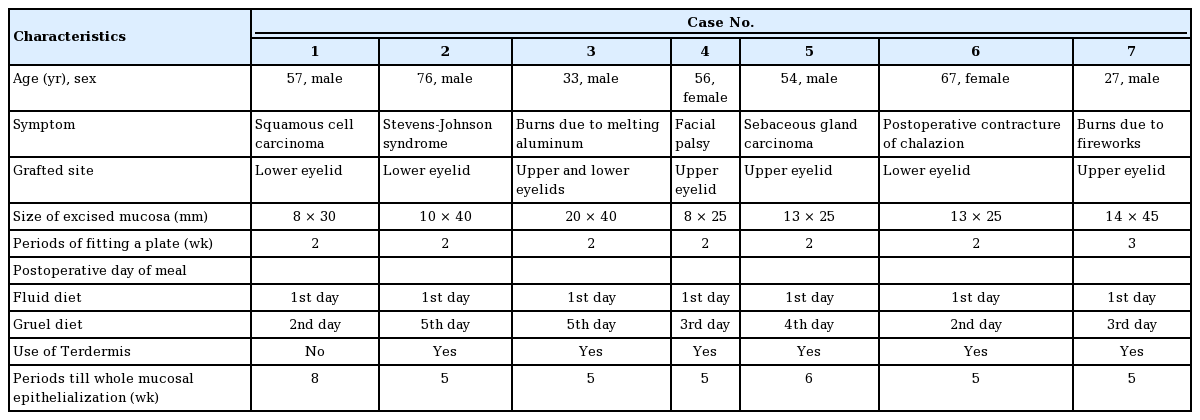
Our analysis was based on the clinical outcomes of seven patients who underwent harvesting of mucosa from the hard palate for reconstruction of the mucosal side of the eyelids. Our study group included five men and two women, with a mean age of 52.9 years. The indications for reconstruction were as follows: one case of squamous cell carcinoma, one case of sebaceous gland carcinoma, one case of Stevens-Johnson syndrome, two cases of burn injury, one case of facial paralysis, and one case of postoperative contracture. In all cases, the contracted tissue in the eyelid was first resected, with the mucosa subsequently grafted onto the defect (Table 1). Artificial dermis was used in six cases, but not in one case.
A retrospective review of patients’ medical records and pictures was conducted. The study was performed in accordance with the principles of the Declaration of Helsinki. All patients in this study provided written (signed) informed consent for the use of preoperative, intraoperative, and postoperative data for academic presentations without disclosure of their personal information.
Operative technique
A transparent, 1-mm-thick palatal plate was formed using thermoplastic resin (Erkodent, Pfalzgrafenweiler, Germany) based on the patient’s maxillary impression obtained prior to surgery (Fig. 1). After mucosal harvesting, the site was cauterized to achieve hemostasis, and an epinephrine gauze packing was applied to the defect for pressure hemostasis. Once hemostasis was achieved, an alginic acid-containing wound dressing (Sorbsan; Aspen Surgical Products, Caledonia, MI, USA) was applied to the harvest site and held in place via compression by the palatal plate. In six cases, the dressing was changed to an artificial dermis (Terudermis; Olympus Terumo Biomaterials Corp., Tokyo, Japan), which was maintained in place again by the plate after 2–3 days. The patients wore the palatal plate continuously for the first postoperative week. After the initial week, the patients were allowed to remove the plate to clean their mouth, with the plate replaced thereafter. Oral cleaning was performed by the patients themselves with no intervention by a dental hygienist, such as by gargling with water after a meal. The plate was used for 2 weeks after surgery. With the palatal plate in place, oral intake of fluids was initiated on postoperative day 1, and gruel intake was initiated on postoperative days 2 to 5, as tolerated.
RESULTS
The size of the mucosal defect at the harvest site ranged from 8×25 mm to 20×40 mm, and the grafted mucosa survived in all cases. The plate was adequately fixed, with no postoperative slippage. The plate did not cause pain, and patients only reported a slight sense of incongruity while eating. There was no incidence of infection (Table 1). Patients were asked to keep the plate in place continuously during postoperative week 1 and then for a subsequent week, during which they were allowed to remove the plate to clean the oral cavity. Since the plate was made based on the patient’s maxillary impression, fixation of the plate was done well. The group that used artificial dermis showed epithelialization within 6 weeks after surgery, while patient without artificial dermis took 8 weeks to attain epithelialization, and there was no contracture in the hard palate.
Representative case
This patient was a 78-year-old man with contracture of the conjunctiva and entropion of the right lower eyelid due to Stevens-Johnson syndrome. Several surgical procedures had been performed to correct the contracture without a curative outcome. Consequently, we proceeded with resection of the contracted eyelid tissue, followed by grafting of the hard palate mucosa. To provide sufficient coverage of the defect, a 10×40 mm area of the hard palate mucosa was harvested. After harvesting, a Sorbsan wound dressing was applied immediately, held in place by compression from the palatal plate, and was changed on postoperative day 2 to Terudermis, which was also held in place by the plate (Fig. 2). Oral fluid intake was initiated on postoperative day 1, with gruel intake started on postoperative day 5. On postoperative day 9, the patient was allowed to remove the palatal plate for gargling. The plate was maintained in place for 14 days after surgery, at which point the patient no longer reported pain. Epithelialization of the hard palate was completed at postoperative week 5 and no contracture was found, and the mucosa at the donor site had completely healed, with no complications, at about 8 months after surgery (Fig. 3).
Preoperative and intraoperative photos. (A, B) Entropion of the right lower eyelid, secondary to Stevens-Johnson syndrome. (C, D) Harvesting of a 10×40 mm area of the mucosa from the hard palate, followed by application of an artificial dermis to the harvest site. (E, F) Resection of the contracted tissue of the lower eyelid, followed by transplantation of the mucosal graft to the defect of the lower eyelid.
DISCUSSION
In this study, we described the combination of a transparent plate and artificial dermis, which led to early epithelialization of the donor site, reduced the risk of postoperative bleeding, protected the harvest site, and allowed earlier oral intake, all without increasing the risk of infection, and consequently improved the surgical outcomes of hard-palate mucosal harvesting. With this combined technique, we obtained good results without complications. Harvested mucosa from the hard palate is used for eyelid reconstruction [1-8], as well as for reconstruction of tracheal cartilage [9] and nasal mucosa [10]. However, there is no consensus on wound management at the donor site. Several methods have been used for this purpose, including the use of obturators to protect the donor site [1,2], fixation of artificial dermis using a tie-over dressing [3], waiting for epithelialization of the raw surface [10], and application of a hemostatic dressing [6].
Prior to the development of our palatal plate, we applied artificial dermis to the donor site, with fixation using silicone gauze with superglue (Aron Alpha; Toagosei Co., Tokyo, Japan) as a conventional method in our hospital to obtain early epithelialization and reduce donor site pain. However, obtaining hemostasis was challenging in these procedures because of difficulties in achieving pressure hemostasis, and this method was often associated with pain during oral intake; nevertheless, it was better than epithelialization of the raw surface. Other limitations included slippage of the silicone gauze and inability to observe the wound directly; furthermore, early detection of signs of infection is difficult.
We thought that the palatal plate had some advantages over the conventional methods. Using our palatal plate, we were able to achieve sufficient compression of the harvest site to obtain hemostasis. The application of Sorbsan was also advantageous for hemostasis and reduced the risk of bleeding. This technique provided sufficient protection of the harvest site for early oral intake because it reduced donor site pain. Previously, we did not use Terudermis, and it took 8 weeks to obtain epithelialization. Thereafter, by combining our conventional method and this plate obturator technique, we could attain good wound management. In short, changing Sorbsan to Terduermis supported early epithelialization within 6 weeks after surgery and prevented scarring and contracture at the donor site. Moreover, because the plate was transparent, it was possible to visualize the donor site without removing the plate, allowing sustained compression to reduce the risk of postoperative infection. Because of the protection afforded by the plate, oral intake could be initiated on postoperative day 1, without fear of infection caused by contamination from the diet. In addition, the plate was fixed well, so there was no slippage of the plate during eating. There was no incidence of infection in our series of seven cases. We allowed patients to remove the plate and gargle by themselves starting 1 week after the operation, but there was no slippage of the Terudermis, showing that the artificial dermis was well fixed. Moreover, patients were able to easily change the plate by themselves. This convenience is also an advantage of our method.
Although the fabrication and fitting of the palatal plate required an extra step before the procedure and fixation of the plate was less stable in patients with few (or no) teeth, compared to the conventional methods, the postoperative benefits of decreased pain, early oral intake, and ease of wound observation support the use of our transparent palatal plate.
This study is limited by its small sample size; however, the combined use of an artificial dermis and transplant plate clearly facilitated wound management. Our transparent palatal plate for wound management of the mucosal donor site of the hard palate resolves some of the limitations of conventional methods. It provides sufficient compression to obtain early hemostasis and protection for early oral intake, without causing pain or infection. Therefore, we propose that our technique is an effective wound management method for hard-palate donor sites.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The Institutional Review Board (IRB) approval was exempted by the IRB of the Tokyo Dental College Ichikawa General Hospital because it was the small case study. Informed consent was obtained.
Patient consent
The patient provided written informed consent for the publication and the use of his images.
Author contribution
Conceptualization: I Tanaka, S Sakai, T Yamauchi. Data curation: all authors. Formal analysis: I Tanaka. Funding acquisition: I Tanaka. Methodology: all authors. Project administration: all authors. Visualization: Y Suzuki, T Yamauchi. Writing - original draft: Y Suzuki, S Sakai. Writing - review & editing: Y Suzuki, I Tanaka, T Yamauchi.