Algorithmic approach to the lymphatic leak after vascular reconstruction: a systematic review
Article information
Abstract
Background
To date, there are no consensus guidelines for management of lymphatic leak in groin vascular reconstruction patients. The goal of this study is to review the relevant literature to determine alternatives for treatment and to design an evidence-based algorithm to minimize cost and morbidity and maximize efficacy.
Methods
A systematic review of the literature was conducted per Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol. Two independent reviewers applied agreed-upon inclusion and exclusion criteria to eligible records. Studies that included patients who underwent groin dissection for oncologic diagnoses and level 5 data were excluded. Interventions were then categorized by efficacy using predetermined criteria.
Results
Our search yielded 333 records, of which eight studies were included. In four studies, the success of lymphatic ligation ranged from 75% to 100%, with average days to resolution ranging from 0 to 9. Conservative management in the form of elevation, compression, and bedrest may prolong time to resolution of lymphatic leak (14–24 days) and therefore cost.
Conclusions
The majority of patients should be offered early operative intervention in the form of lymphatic ligation with or without a primary muscle flap. If the patient is not an operative candidate, a trial of conservative management should be attempted before other nonsurgical interventions.
INTRODUCTION
Lymphatic leak is a serious complication of vascular surgery that incurs significant cost to the healthcare system and morbidity to the patient [1-5]. Disruption of lymphatic channels during vascular surgery and failure of subsequent healing may result in persistent leakage, presenting as lymphocele or lymphocutaneous fistula, and may occur in as many as 18% of arterial interventions [6]. A variety of factors have also been identified that may predispose patients to lymphatic leak including surgical procedure and graft type, incision techniques, as well as patient demographics [3,5,7]. As a result, patients who develop postvascular dissection lymphatic leak have delayed wound healing, are at greater risk of infection and graft rejection, and spend more time in the hospital, thereby increasing the cost of care [2,5,6].
First-line interventions of lymphatic leak currently include both surgical strategies–primary muscle flaps, lymphatic ligation, and suction drain placement [8-11]–and nonoperative strategies–bed rest, elevation, compression, prophylactic antibiotics, vacuum assisted closure therapy, and glue embolization [9,12-14]. There are data to support each of these strategies, however, there is no consensus regarding how to expeditiously resolve lymphatic complications.
The goal of this systematic review is to develop an evidencebased, cost-conscious, algorithmic approach to management of lymphatic leak after groin dissection for vascular reconstruction.
METHODS
Literature search
A systematic review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement. The literature database was extracted by searching the Scopus, PubMed, and Cochrane Library databases on November 11, 2019. The search phrases used were combinations of “lymphatic leak,” “lymphorrhea,” “lymphocele,” “groin surgery,” “axillofemoral bypass,” “femoral artery surgery,” “femoral endarterectomy,” and “femoral-popliteal bypass.” The studies included were English articles published between 1968 and 2018.
Studies included were randomized-controlled trials, cohort studies, case-control studies, and case series that pertain to the incidence, diagnosis, or treatment of lymphatic complications (i.e., lymphatic leak or lymphocele) after open groin dissections for the purpose of vascular reconstruction. We excluded studies with level five data (i.e., case reports, discussions, or expert opinion), studies including data on groin dissection for indications other than vascular reconstruction, studies involving endovascular interventions or saphenous vein harvest, and studies that reported data only on lymphoceles without reporting data on lymphatic leak.
Data collection and quality of recommendation assessment
Studies that met inclusion and exclusion criteria were then assessed by three independent reviewers. Data collected were year of publication, study design, level of evidence, number of patients, treatment modality, success rate of treatment described, and average days to successful treatment.
To evaluate strength of treatment recommendation, interventions described in the articles were categorized by efficacy. Success rate, days to resolution, level of evidence, consensus recommendation, and number of patients studied were used to compare studies. The treatment modalities that were supported by higher level evidence, were consensus recommendations from selected articles, and included robustly powered studies were given the designation of “efficacious.” These interventions were considered first-line treatments in the algorithm. To compare first-line treatments, the treatment with the lowest days to resolution and highest percent efficacy was favored. Treatment modalities that were supported by lower level evidence, were subject to conflicting recommendations in the selected articles, or were supported by low-powered studies were given the designation of “mixed efficacy.” Interventions with mixed efficacy were suggested as second-line treatments.
RESULTS
Literature search and study selection
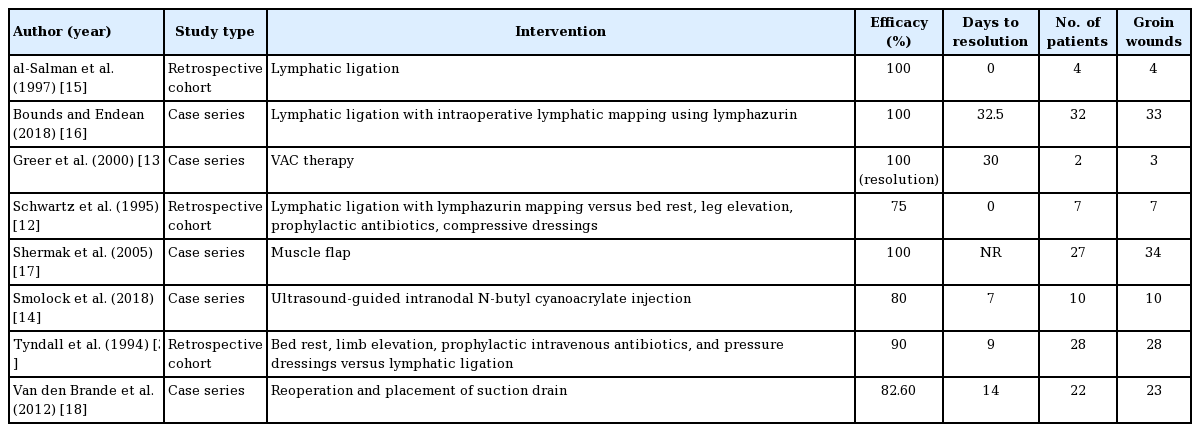
Our literature search yielded 333 total records, and 219 were remaining after deduplication. These 219 records were screened by title and abstract for relevance, yielding 38 records eligible for full-text review. Of these 38 records, eight met inclusion and exclusion criteria and were included in the study (Fig. 1). Three retrospective cohort studies [3,12,15], and five case series [13, 14, 16-18] were included (Table 1).
Diagram of our included articles. Our query yielded 333 records, which after deduplication included 219 unique records. After screening for title and abstract by two independent reviewers, 38 records were read in full. After applying full inclusion and exclusion criteria, eight articles were included in our final review.
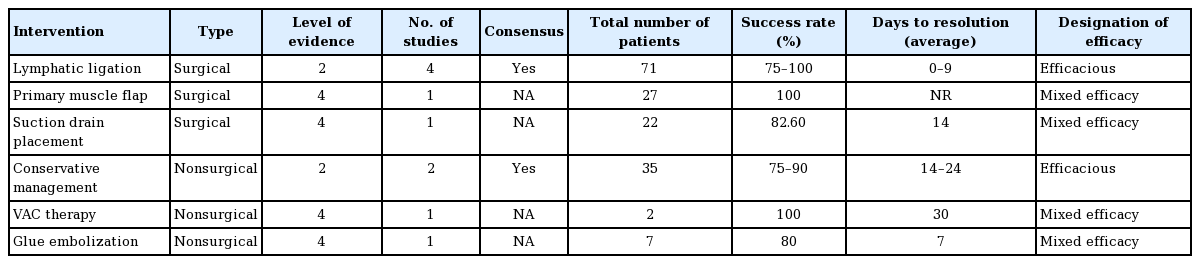
Interventions and strength of recommendation
Lymphatic ligation was found to be effective in the treatment of lymphatic leak in a total of four studies with a success rate of 75% to 100% and a range of average days to resolution of 0 to 9 [3,12,15,16]. The studies that supported treatment with lymphatic ligation comprised level 2 through 4 evidence and no studies found lymphatic ligation to be unsuccessful. Additionally, the total number of patients studied for lymphatic ligation was 71, which was the highest for all interventions. For these reasons, lymphatic ligation was categorized as “efficacious” and considered a first-line surgical treatment option (Table 2).
Conservative management, which consisted of bedrest, elevation, compression, and prophylactic antibiotics, was found to be effective in two studies with a success rate of 75% to 90% and a range of average range of days to resolution of 14 to 24 [3,12]. These studies were comprised of level 2 through 4 evidence and included 35 patients. Therefore, conservative management was designated as “efficacious” and considered the first-line nonsurgical treatment option in the algorithm. One study retrospectively compared early lymphatic ligation to conservative management, and days to resolution was 9 ± 3 days for the operative group versus 24 ± 3 days in the nonoperative group (P < 0.01) [3,12]. Therefore, early operative intervention was favored over conservative management in the algorithm.
In one level 4 study including 22 patients, suction drain placement without lymphatic ligation was effective in 82.6% of patients with an average time to resolution of 14 days [18]. When compared to lymphatic ligation, there are fewer patients studied and lower quality evidence. For these reasons, suction drain placement was assigned “mixed efficacy” and lymphatic ligation was favored in the algorithm.
In a case series of 34 groin lymphatic complications, sartorius, gracilis, rectus abdominis, and rectus femoris muscle flaps were used both with and without with lymphatic ligation [17]. No days to resolution was reported, but this study demonstrated 100% resolution of lymphatic leak and lymphocele. Another level 2, retrospective cohort study of 58 patients demonstrated that prophylactic muscle flaps decreased the incidence of infection and wound breakdown in all patients undergoing open groin surgery [8]. This reduction in infection and wound breakdown (70% absolute risk reduction [ARR] and 42.4% ARR, P < 0.001, respectively) was highest in patients with risk factors like smoking, obesity, re-operative groins, and prosthetic graft material [8]. Patients who required salvage muscle flaps for groin complications were more likely to have two of the aforementioned risk factors (P = 0.0004) [8]. There was no time to resolution reported. Primary muscle flap was supported by a single case series and considered a treatment with “mixed efficacy.”
One small level 4 study found that vacuum assisted closure therapy was successful in two patients after an average of 30 days of treatment [13]. Interventional radiology glue embolization was found to be 80% successful in a 10-patient, level 4 study after a trial of failed conservative therapy. The time to resolution was an average of 7 days [14]. These interventions are supported by a single, small study with low-level evidence and were assigned “mixed efficacy.”
DISCUSSION
These treatment modalities were synthesized into an algorithm to optimize efficacy and minimize morbidity. The first decision point in the algorithm is whether the patient should be treated operatively or non-operatively. In one retrospective, single-center study that compared operative versus nonoperative management for lymphatic leaks, lymphatic leaks that were managed with lymphatic ligation with intraoperative lymphatic mapping at the time of diagnosis resolved on average 13 days sooner than those that were treated conservatively (P < 0.01) [3]. These results were corroborated in another, smaller retrospective study that demonstrated shorter hospital stay, fewer recurrences, and lower complication rates with lymphatic ligation aided by isosulfan blue [12]. For this reason, we recommend that most patients who are of acceptable anesthetic risk should undergo lymphatic ligation at the time of diagnosis instead of conservative management (Fig. 2).
The evidence-based algorithm. The algorithm was designed to minimize morbidity and cost while maximizing efficacy in the management of the lymph leak patient. The majority of patients should receive early operative intervention, but a few, select patients without risk factors associated with lymphatic leak–aortobifemoral bypass graft, preoperative length of stay >1 day, or re-operative groin–would benefit from conservative management.
Although primary muscle flap was considered a treatment with “mixed efficacy,” we recommend that a sartorius flap be included to augment lymphatic ligation. In a case series of 34 groin lymphatic complications, sartorius, gracilis, rectus abdominis, and rectus femoris muscle flaps were used in conjunction with lymphatic ligation in 22 of the 34 complication sites. None of the patients who underwent flap surgery had recurrence of lymphocele or lymphatic leak after 1 year [17]. Additionally, flap biopsies were taken 1 year after the index operation in one of the patients. The transposed muscle demonstrated a significant increase in lymphatic channels, suggesting that the muscle itself becomes a vessel for lymphatic shunting [17]. A retrospective cohort study of 68 open groin operations also found that patients with two of the following risk factors: smoking, obesity, re-operative groins, and synthetic graft material, were associated with necessitating muscle flap salvage of their reconstruction [8]. While there are no studies that demonstrate that lymphatic ligation with primary muscle flap is superior to lymphatic ligation alone, we recommend primary sartorius flap at the time of lymphatic ligation because it is a low-morbidity operation that has been shown to decrease the risk for infection [8] and may reduce the risk of persistent lymphatic leak (Fig. 2).
While early operative intervention demonstrated a shorter time to resolution when compared to nonsurgical management, nonsurgical management was shown to be effective in the management of lymphatic leak, and some patients did not require a second operation to heal. This is an important consideration as reoperation on a reconstructed groin is not without risk and morbidity. There are no studies that demonstrate clear predictors of failure of conservative therapy in the literature. However, certain surgical and demographic risk factors predispose patients to lymphatic leak. In a retrospective study that included 2,679 groin dissections, procedure-related incidence of groin lymphatic complications were found to be significantly higher in redo operations and aortobifemoral bypass (ABFB) [3]. In a prospective study of 120 ABFB patients, patient factors like smoking, obesity, renal disease, and diabetes were not found to be associated with groin lymphatic complications. However, a preoperative length of stay greater than 1 day was associated with incisional complications of the groin (odds ratio, 3.94) [5]. Patients with these aforementioned risk factors–ABFB, redo operations, and preoperative length of stay greater than 1 day–should be considered high-risk for lymphatic leak. One limitation of this study is the inclusion of only open groin dissections for vascular reconstruction. We appreciate that the results of this study may not be applicable to endovascular surgery, or to saphenous vein harvest, in the setting of cardiac bypass surgery. These factors do not directly predict failure of nonsurgical management, but they may act as a surrogate to determine which patients require early operative invention to heal their lymphatic leak (Fig. 2).
Another important factor that affects who would be appropriate for a trial of nonoperative management is the risk of serious infection. It has been established that synthetic grafts significantly increase the risk of infection involving the arterial reconstruction when compared to autogenous vein grafts, endarterectomies, and arterial allografts [19]. We recommend against conservative management in patients with synthetic graft material as there is an unacceptable risk for infection involving the reconstruction (Fig. 2).
The concept of prophylactic muscle flaps for high-risk patients has been described [8]. Larger and more rigorous studies are needed to determine which patients might benefit from prophylactic muscle flaps, at the time of vascular reconstruction to prevent subsequent lymphatic leak. Additionally, there have been reports of microsurgical lymphaticovenous shunting in the treatment of lymphatic leak after lymph node excision in the groin [20]. This technically demanding operation shows promise to be a future treatment of lymphatic leak post-vascular reconstruction of the groin.
The available data support that early operative intervention in the form of lymphatic ligation with simultaneous muscle flap is the most efficacious and cost-effective treatment for lymphatic leak. If the patient is not an operative candidate, we recommend a 3-week trial of conservative management–bedrest, elevation, prophylactic antibiotics, and pressure dressing. If the lymphatic leak is not resolved at the end of the trial, procedural adjuncts like interventional radiology embolization may be utilized. It is also acceptable to attempt conservative management to reduce the morbidity associated with reoperation in patients without prosthetic material and who do possess risk factors associated with prolonged lymphatic leak. Due to its low incidence, it is difficult to identify the predictors of lymphatic complications. With the help of this algorithm, the reader may use evidencebased guidelines to minimize morbidity and cost while considering treatment efficacy and predictability of resolution in the lymphatic leak patient.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization: PJ Nicksic, HS Nayar, BF Michelottii. Methodology: PJ Nicksic, KM Condit, HS Nayar. Writing - original draft: PJ Nicksic, KM Condit. Writing - review & editing: PJ Nicksic, BF Michelottii.