Evaluation of pedicled flaps for type IIIB open fractures of the tibia at a tertiary care center
Article information
Abstract
Background
Soft tissue coverage plays a vital role in replacing the vascularity of the underlying bone in Gustilo type IIIB fractures. The aim of this article was to evaluate the feasibility of local pedicled flaps in type IIIB fractures at a tertiary care center.
Methods
We included all cases of open Gustilo-Anderson type IIIB fractures of the tibia treated with local flap coverage from January 2017 to February 2019. We carried out a retrospective analysis to investigate the relationships of complications, hospital stay, and cost-effectiveness with the choice of flap, infective foci, site and size of the defect, and type of fixation.
Results
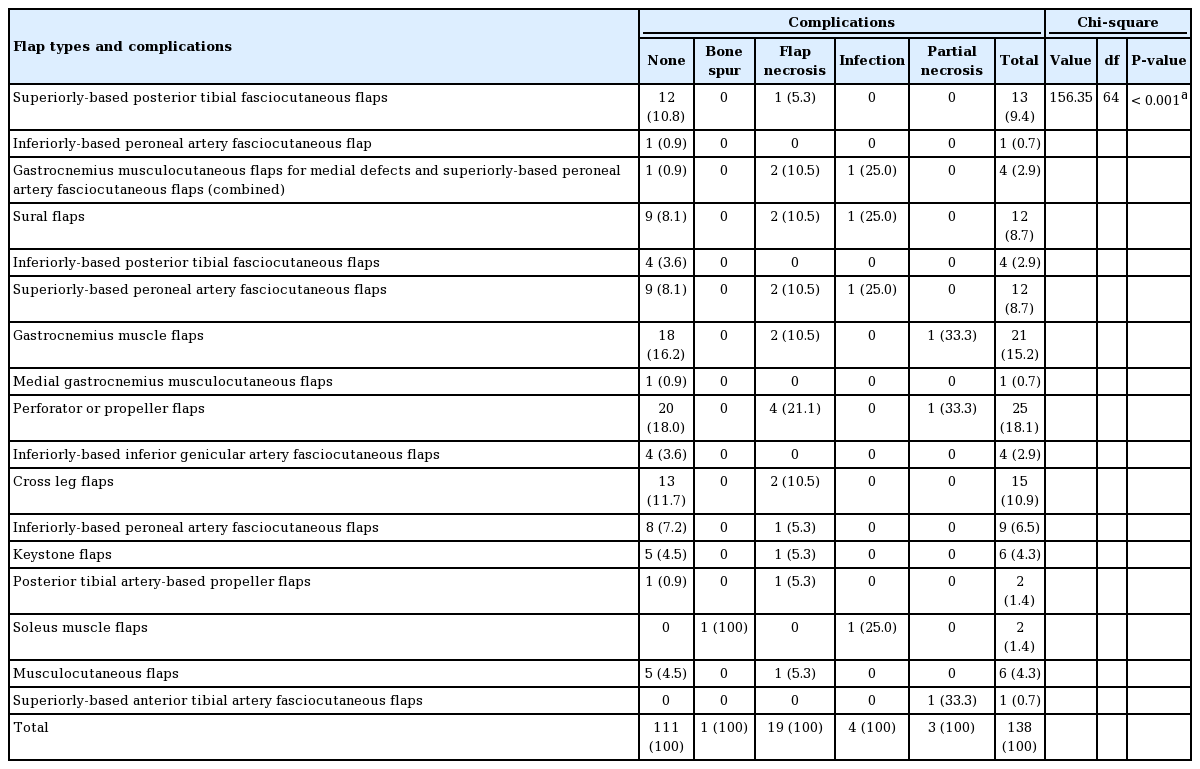
Out of 138 Gustilo type IIIB fractures analyzed in our study, 27 cases had complications, of which 19 (13.76%) involved flap necrosis, four (2.89%) were infections, three (2.17%) involved partial necrosis, and one (0.72%) was related to bone spur development. Flap complications showed a statistically significant association with the perforator flap category (propeller flaps in particular) (P=0.001). Flap necrosis showed a significant positive correlation with cases treated within 3 weeks after trauma (P=0.046). A significant positive correlation was also found between defect size and the duration of hospital stay (P=0.03).
Conclusions
Although local flaps are harvested from the same leg that underwent trauma, their success rate is at least as high as microvascular flaps as reported from other centers. Amidst the local flaps, complications were predominantly associated with perforator flaps.
INTRODUCTION
The recent technological advances experienced by humanity are not without disadvantages, including an increased frequency of high-velocity trauma and industrial accidents, resulting in an increased incidence of open fractures.
Open fractures pose a challenge to the trauma team in terms of loss of soft tissue, loss of bone, the presence of contamination potentially leading to infection, and an elevated incidence of non-union. In view of these anticipated complications, the need for aggressive debridement, adequate fracture fixation, and early flap coverage in reducing morbidity cannot be overemphasized [1]. Achieving those goals is only possible when there is a collective approach involving all trauma team members, including the plastic surgeon and orthopedic surgeon, aiming to save the limb.
For the soft-tissue coverage of defects, either microvascular-free flaps or non-microvascular local flaps are available. There is no clear dictum regarding the choice of flap [2], although non-microvascular local flaps are comparatively easier to perform given the lower requirements in terms of infrastructure and expertise [3].
The main concern regarding local flaps is that reconstructive surgeons are generally sceptical about the survival of local flaps harvested from a traumatic zone [4]. This underscores the need for empirical research to establish the actual feasibility of these flaps in a trauma scenario by analyzing flap complications and assessing the impact of these complications on cost-effectiveness for both the patient and the treating hospital.
METHODS
The study was conducted at the department of orthopedics and plastic surgery at a tertiary care hospital. All cases of open Gustilo-Anderson type IIIB fractures of the tibia that received soft tissue coverage in the form of non-microvascular flaps from January 2017 to February 2019 were included. Written informed consent of the patients was obtained at the time of surgery, when they received an explanation of the type of procedure they would undergo. Cases operated at other centers, primarily for debridement and bony fixation, that were referred to us for soft tissue coverage were also included. A retrospective analysis of these cases was conducted, considering the following factors: (1) time of presentation: acute or chronic (less than 3 weeks or more than 3 weeks after injury); (2) status of the exposed bone cortex: with or without periosteum; (3) soft-tissue defect dimensions ( < 5 cm, 5–10 cm, 10–15 cm, 15–20 cm, and > 20 cm); (4) site of the defect (proximal, middle, or distal third); (5) the area involved (anteromedial, anterolateral, posterolateral, posteromedial, or a combination thereof); (6) type of flap coverage; or (7) complications (partial necrosis, complete necrosis, incidence of infection, and any other complication).
These cases were then tabulated and analyzed using the Pearson chi-square test in SPSS version 23 (IBM Corp., Armonk, NY, USA).
RESULTS
Preoperative analysis
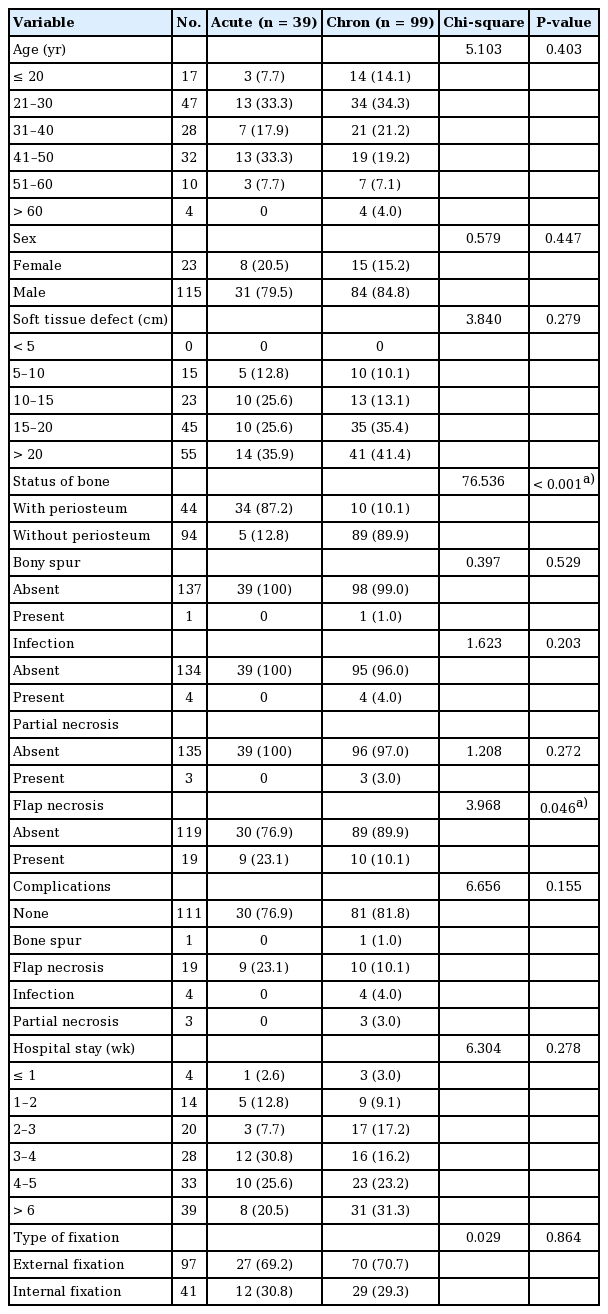
Of the 138 patients who were included in the study, 115 (83.3%) were male and 23 were female (16.7%). Among them, 39 cases presented within 3 weeks after the injury (acute), while the remaining 99 cases presented more than 3 weeks after the injury (chronic).
The age of the patients ranged from 4 to 60 years, with an average of 34.4 years. The distal third of the leg was most commonly involved (46 cases), followed by the middle third (40 cases) and proximal third (39 cases).
According to the site of involvement, the most commonly affected area was distal (anteromedial distal, 14.5%; posteromedial distal, 7.5%), followed in descending order by the proximal zone (anteromedial proximal, 13.8%; posteromedial proximal, 7.5%) and the middle zone (anteromedial middle, 11.6%) (Fig. 1). In addition, In the proximal and middle zones, the posterolateral aspect was least commonly involved.
An island sural flap for a defect in the anteromedial aspect of the distal part of the leg with follow-up photographs. (A) Exposed bone before debridement. (B) Exposed bone after debridement. (C) Surgical planning. (D) Mobilization of the flap. (E) After mobilization. (F, G) One-year follow-up. (H) Four-year follow-up of the patient.
The size of the soft tissue defects was distributed as follows: 5–10 cm (10.9%), 10–15 cm (16.7%), 15–20 cm (32.6%), and > 20 cm (39.9%).
Age, sex, the site of the defect, the size of the defect, and the chronicity of the wound did not have any significant correlations with complications.
Postoperative and intraoperative analysis
Ninety-seven patients (70.3%) underwent external fixation, while 41 patients (29.7%) underwent internal fixation, including plating and intramedullary nailing. In the 97 cases of external fixation, complications were seen in 19 cases (19.5%), while in the 41 cases of internal fixation, eight (19.5) had complications. The association between complications and type of fixation was not found to be statistically significant (P = 0.7).
Out of the total number of cases, 104 (75.36%) underwent fasciocutaneous flaps and 34 (24.64%) underwent muscle or musculocutaneous flaps. Among the fasciocutaneous flaps, perforator flaps (including propeller flaps) were the most predominant variety used (27/104, 25.96%), and gastrocnemius muscle or musculocutaneous flaps were predominant (31/34, 94.11%) in the muscle flap category (Fig. 2).
A soleus flap for a defect in the distal part of the tibia. (A) Wound prepared for flap cover. (B) Soleus rerouted cover the exposed bone. (C) Raw surface left covered with a skin graft.
Among the 104 cases of fasciocutaneous flaps (Fig. 3), 86 cases (82.7%) had no complications and 18 cases (17.3%) had complications. Among the 34 cases of musculocutaneous flaps, 25 cases (73.5%) had no complications and nine cases (26.5%) had complications. Although the difference did not reach statistical significance, musculocutaneous flaps showed a higher percentage of complications (26.5%). However, in a comparison of complications among the different flap groups, a higher percentage of flap necrosis was seen in perforator flaps (including propeller flaps) (Figs. 4, 5) accounting for 21.1% of cases, followed by two cases each for the five other types of flaps. This association was statistically significant (P = 0.001) (Table 1).
The inferior peroneal artery fascia flap was performed for the distal tibia. (A) Primitive wound. (B) Surgical plan. (C) Close-up of view of raw wound. (D, E) Lateral and superior views of the inferior-based peroneal artery fascia flap.
A perforator flap for a defect in the distal tibia. (A) Mobilization of the flap. (B) After mobilization and skin grafting.
A propeller flap for a defect in the lateral aspect of the distal leg. (A) Soft tissue defect. (B) Mobilization of the flap. (C) Surgical dissection and mobilization. (D) Coverage of the exposed none and skin grafting.
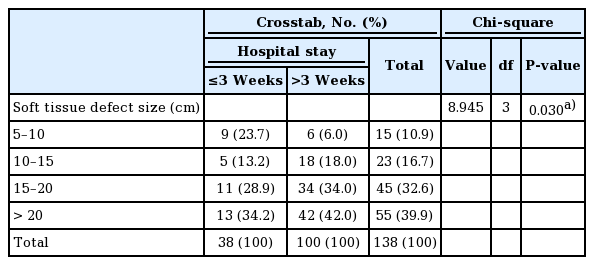
Of the 138 cases, 38 had a hospital stay lasting for < 3 weeks, while 100 had a hospital stay > 3 weeks. In our study, the average duration of the hospital stay for acute and chronic cases was 28.05 ± 13.00 days and 36.37 ± 16.64 days, respectively. We found that the proportion of cases with a hospital stay lasting for > 3 weeks steadily increased—from 6% to 18%, 34%, and 42%—as the size of the soft tissue defects increased from 5–10 cm to 10–15 cm, 15–20 cm, and > 20 cm, respectively, and this relationship was statistically significant (P = 0.030) (Table 2). However, there was no statistically significant correlation between the soft tissue defect size and complications (P = 0.572), or between the choice of flap and the duration of hospital stay (P = 0.390).
Statistical analysis
Correlational analysis using the Pearson chi-square test was performed between the types of flaps, bony fixation, the size of the defect, the site of the defect, age group, and sex and complications to identify factors related to complications. Correlations were also calculated between flap type, defect size, and the length of hospital stay to determine factors influencing the duration of inpatient care.
A significant correlation was found between the type of flap and the complication rate. Perforator flaps had the highest frequency of flap necrosis (21.1%), with a P-value of 0.001 for the correlation. Meanwhile, age, sex, the site of the defect, the size of the defect, the type of bony fixation, and the chronicity of the wound did not have any significant correlations with complications. Complications were also more common in patients who underwent surgery during the acute period (less than 3 weeks following trauma) than in those who underwent surgery later.
DISCUSSION
Lower limb trauma is a rapidly-growing category of injuries worldwide as a result of road traffic and industrial accidents. Reconstructive surgeons are normally involved in lower limb trauma management of Gustilo type IIIB and IIIC injuries. Soft tissue defects are predominantly dealt with using pedicled or free flaps, and the outcomes are variable. The benefits of flap reconstruction in fractures have already been established in several studies [1]. Numerous researchers have tried to identify factors that determine the flap outcomes in fracture patients.
It is imperative that trauma centers that handle these cases make attempts to evaluate the outcome of reconstructions. Doing so will enable the team and the center to improve their decision-making and to make better predictions regarding their patients’ prognoses. It will also help establish a cost-effective model both for the center and for patients. A similar study was conducted at our institution to investigate the factors determining flap complications and the length of hospital stay in these patients. A retrospective study was designed, the data were compiled using patients’ case files, and the results were analyzed. As an initial step, we sought to analyze the existing predisposing factors of flap complications and length of hospital stay.
Factors contributing to flap failure
Prior studies in the literature have identified several factors, including chronicity of presentation, age, comorbidities (e.g., diabetes) hindering wound healing, diabetes, type of fixation, and defect size, as associated with flap failure.
These studies have provided valuable insights into the predictive factors of flap failure; hence, the above-mentioned factors were incorporated in our study.
Age and flap complications
The majority of the cases in our study were in the age group of 21–40 years, which accounted for 54.3% of cases, followed by the age groups of 40–60 years, < 20 years, and > 60 years, which accounted for 30.4%, 12.3%, and 2.9% of cases, respectively. No statistically significant correlation was found between age groups and flap complications (P = 0.523). However, the proportion of complications increased with age. Our finding is comparable with the findings of the study conducted by Ivanov et al. [5], in which the majority of the cases were in the age range of 31–45 years (35%), followed by the age groups of 18–30, 46–60, and > 60 years, which accounted for 34%, 20%, and 7% of cases, respectively. However, a systematic review by de Blacam et al. [2] correlated sural flap complications with predisposing factors and reported that age and venous insufficiency were independent risk factors for flap and wound complications. The study by Innocenti et al. [6] implicated age, flap dimensions, arc of rotation, peripheral vascular disease, and comorbidities such as diabetes as chief factors causing complications in perforator flaps. The study by Lese took into account the Charlson comorbidity index, which considers various comorbidities, and the vascular axis on which the propeller flaps were based [7,8]. They concluded that the use of peroneal artery-based propeller flaps and a Charlson comorbidity index of 2 or greater were definite risk factors.
Sex and flap complications
In our study, 23 cases (16.7%) were female and 115 (83.3%) were male. Three of the 23 female patients (13%) had complications in the form of flap necrosis, while 14 of the 115 male patients (12.2%) had various complications. No statistically significant correlation was found between sex and complications. In the study by Ivanov et al. [5], 15 cases (17.6%) were female and 70 (82.4%) cases were male, which is a comparable ratio to that of our study. In the study conducted by Chua et al. [9], 6.74% of the patients were female patients and 93.36% were male. Neither of those studies compared complications according to sex.
Early and late presentation
We observed that out of 138 cases, 39 had an acute presentation ( < 3 weeks) and 99 had a chronic presentation ( > 3 weeks) (Table 3). Among the 39 cases with an acute presentation, 30 (76.90%) had no complications, while nine (23.10%) had complications in the form of flap necrosis. Among the 99 cases with a chronic presentation, 81 (81.80%) had no complications and 18 (18.20%) had complications. Flap necrosis was significantly more common in the acute cases (23.1%) than in the chronic cases (10.1%), and this difference was statistically significant (P < 0.05). In a study conducted by Kamath et al. [10] that analyzed 151 cases, patients who presented within 10 days, from 10 days to 6 weeks, and at > 6 weeks had complication rates of 26.6%, 73.68%, and 52.6%, respectively [10]. In another study by Chua et al. [9], among 30 early flap coverage cases ( < 72 hours), 15 cases (54%) had no complications and 14 cases (46%) had complications, while among 59 late flap coverage cases ( > 72 hours), 42 had complications. That study suggested that early coverage (within 72 hours) yielded more favorable results in terms of better outcomes, a lower rate of infections, and shorter hospital stays.
Type of flap and complications
In total, 104 cases (75.36%) in our study underwent fasciocutaneous flap coverage and 34 cases (24.64%) underwent musculocutaneous flap coverage. Among the 104 cases of fasciocutaneous flaps, 86 cases (82.7%) had no complications, while 18 cases (17.3%) had complications. Among the 34 cases of musculocutaneous flaps, 25 cases (73.5%) had no complications and nine cases (26.5%) had complications. Although the difference did not reach statistical significance, musculocutaneous flaps showed a higher percentage of complications (26.5%). However, in a comparison of complications among the different flap groups, a higher percentage of flap necrosis was seen in perforator flaps (including propeller flaps), accounting for 21.1% of cases. This association was statistically significant (P = 0.001). The complications can be attributed to the proximity of these perforators to the zone of trauma with probable microscopic intimal damage that was not identified intraoperatively. In addition, perforator-based flaps are more difficult to perform than axial flaps (fasciocutaneous or musculocutaneous) and a refined microscopic technique is required. The complications of bone spur, infection, and partial flap necrosis did not show statistically significant associations with flap type. In a study conducted by Franken et al. [11], when comparing fasciocutaneous flaps and musculocutaneous flaps, fewer postoperative complications were observed in the patients treated with the latter type of flap (47.4% vs. 21.2%, respectively). However, their study did not find a significant correlation between flap type and complications. Li et al. [12] studied flap outcomes in ankle and foot reconstruction. They divided the foot and ankle into anatomically-based sub-regions and evaluated the risk factors that contributed to flap failure. Free flaps were also included in their study. Their study found that the choice of flap was correlated with failure. However, Rodriguez-Collazo et al. [13] reported that there was no significant difference in outcomes between free and pedicled flaps.
Site of defect and complications
In our study, soft tissue defects were found in the proximal third of the leg in 39 cases (Fig. 6), the middle third in 40 cases, and the distal third in 46 cases (Figs. 7-9). In three cases, the middle and distal thirds were involved, and in one case, the proximal and middle thirds were involved. No statistically significant correlation was found between the defect site and complications (P = 0.900). However, the anteromedial distal, anteromedial proximal, and anteromedial middle aspects, which accounted for 55 of the 138 cases, had somewhat more complications than the other sites. This can be partly explained because of the higher frequency of defects at these sites. In a study conducted by Kamath et al. [10], soft tissue defects were predominantly found in the distal third (66 cases), followed by the middle third (45 cases) and the proximal third (33 cases). However, they did not report correlations between the site of soft tissue defects and complications.

A gastrocnemius flap for a defect in the proximal leg. (A) Raw surface after internal fixation. (B) Mobilization of the gastrocnemius muscle. (C) Skin grafting over the flap.
Clinical photographs of follow-up of island sural flap for distal third of leg (A) and superior based medial fasciocutaneous flap (B).

Clinical photographs of follow-up of inferior-based lateral fasciocutaneous flap (A), superior-based medial fasciocutaneous flap (B), and sural flap for ankle defect (C).
Size of defect and complications
In our study, the cases with defect sizes of 5–10 cm, 10–15 cm, 15–20 cm, and > 20 cm had complication rates of 26.6%, 8.6%, 20%, and 21.8% respectively, which was not found to be significant (P = 0.572). This finding is in contrast to a study by Shasti et al. [14] on free flaps, which found a significant correlation between large defect size ( > 200 cm2) and partial/total flap failure (n = 80, P = 0.023). In another study by Koepple et al. [15] on 149 patients, wherein for larger defects muscle-based flaps were used (231 ± 38.6 cm2) and fascio-cutaneous flaps for smaller defects (164 ± 13.7 cm2), partial flap necrosis was generally more common in muscle- based flaps but no difference was observed in cases of defects larger than 300 cm2.
Type of fixation and complications
In our study, 97 cases (70.3%) underwent external fixation and 41 cases (29.7%) underwent internal fixation. Among the 97 cases of external fixation, 19 cases (19.5%) had complications, while among the 41 cases of internal fixation eight cases (19.51%) had complications. However, this did not reflect a statistically significant difference (P = 0.700). In the study of Chua et al. [9], 72 cases (80.89%) underwent external fixation, 16 cases (17.97%) underwent internal fixation, and one case (1.12%) received a slab as the initial fixation. In their study, two of 11 flap failure cases (12.5%) were in intramedullary nailing cases and nine cases (12.5%) were in cases of external fixation; the difference was not statistically significant. In another study by Kamath et al. [10], 82 of 151 cases (54.30%) were managed by external fixation and 69 cases (45.70%) were managed by internal fixation. They did not report complications with respect to different modalities of fracture fixation.
Other patient factors
Although our study was limited to the above-discussed factors, a study conducted at the central hospital of Wuhan, China analyzed cases of anterolateral thigh free flap failures and reported that the mental health of the patient was the factor most closely associated with the outcomes of free flap procedures [16]. To further investigate this factor, it would be worthwhile for further research to investigate correlations between a preoperative psychological assessment and flap complications.
Flap factors
Mishra et al. [17] reported that complications were predominantly observed when latissimus dorsi muscle or musculocutaneous flaps were used to reconstruct small defects, and attributed this tendency to the muscle bulk and kinking of the long pedicle.
Factors contributing to prolongation of the hospital stay
The proportion of cases with a hospital stay lasting for > 3 weeks progressively increased from 6% to 18%, 34%, and 42% as the size of soft tissue defect increased from 5–10 cm to 10–15 cm, 15–20 cm, and > 20 cm, which was a statistically significant relationship (P = 0.030). Pastars et al. [18] reported 153 cases of oral cancer where they removed the tumor and simultaneously placed free flaps on the defect. The average hospital stay was 20.5 days (range, 8–44 days). They observed that the duration of hospital stay was significantly longer (P < 0.05) when the tumor—and hence the defect made after removal of the tumor— was larger.
Although similar studies have been conducted in the past, a noteworthy contribution of this study is that it investigated the relationships of patient-, defect-, and surgeon-related factors with overall complications (including flap necrosis) and hospital stay. Unlike the differential complication rates observed in other studies, such as that by Kamath et al. [10], our study did not find a statistically significant difference between the use of fasciocutaneous flaps and muscle or musculocutaneous flaps. Hence, we are convinced that the choice of flaps to be used in various zones of the leg should depend on further procedures, such as bone exploration or tendon transfers. In cases requiring secondary procedures, it is recommended to use a flap that provides a skin component along with the flap itself (i.e., a fasciocutaneous or musculocutaneous flap) depending on the site of defect.
Major points of this study
The major points derived from this study are as follows: first, age did not show a significant correlation with complications after flap surgery, but the proportion of complications did increase with age. Second, surgery performed within 3 weeks after trauma was associated with a significantly higher risk of complications in local flaps. Third, no significant difference in the complication rate was found between fasciocutaneous flaps and musculocutaneous flaps. Fourth, flap necrosis was observed significantly more frequently in propeller flaps (a type of perforator flap) than in any other flap. Fifth, the size of the defect was not a significant contributor to complications, but it did have an impact on the length of hospital stay. Sixth, no significant difference was found in the complication rate between internal and external fixation.
Conclusion
The timing of the surgical intervention (within 3 weeks from the time of injury) and the use of propeller flaps (a type of perforator flap) for reconstruction was associated with a significantly higher rate of complications. Although age and defect size were not associated with the complication rate, the length of hospital stay was significantly affected by the choice of flap. Furthermore, the authors recommend internal fixation for bone stabilization to promote technical ease for reconstruction purposes, as the type of fixation did not alter the complication rate.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of All India Institute of Medical Sciences (IRB No. AIIMS/IEC/21/211) and performed in accordance with the principles of the Declaration of Helsinki. Written informed consent was obtained.
Patient consent
The patients provided written informed consent for the publication and the use of their images.
Author contribution
Conceptualization: M Dhingra, D Chattopadhyay. Data curation: M Vathulya, M Dhingra, H Nongdamba, VK Dhingra. Formal analysis: M Dhingra, H Nongdamba, A Kapoor. Methodology: D Chattopadhyay, V Mago, P Kandwal. Project administration: VK Dhingra. Writing - original draft: M Vathulya, M Dhingra. Writing - review & editing: M Vathulya, M Dhingra, A Kapoor.