Comparison of porcine and human acellular dermal matrix outcomes in wound healing: a deep dive into the evidence
Article information
Abstract
Acellular dermal matrices (ADM) are a novel graft. The goal of this systematic review is to evaluate the evidence behind differences in human and porcine ADM, irrelevant of manufacturing method, and to determine if there is enough of an evidence base to change clinical practice. An extensive literature search was performed through MEDLINE and Embase with search terms defining a population, intervention and outcome. Title and abstract exclusion were performed with other exclusion criteria. In 191 articles were found after exclusion of duplicates, with only 29 remaining following exclusions. Ten studies were found to have level I and II evidence (I=3, II=8), of which two were histopathological, one was an animal model, one was a systematic review, and six were clinical. The remaining studies were reviewed and considered for discussion, but did not hold high enough standards for medical evidence. Strong clinical evidence already exists for the use of human ADM, but questions of access, cost, and ethics require consideration of a xenograft. Histopathologically, evidence suggests minimal long-term differences between human and porcine ADM, although there is a short acute immune response with porcine ADM. Clinically, there is limited difference in outcomes, with a small range in effect of different ADM preparations. Considering the effectiveness of ADM in wound healing, more high-level research with appropriate statistical analysis to facilitate a future meta-analysis is recommended to justify a transition from human to porcine ADM.
INTRODUCTION
While acellular dermal matrices (ADM) can be considered a fairly novel tool in the belt of a plastic and reconstructive surgeon, its impact on the approach to complex clinical situations cannot be understated. Finding a foothold in areas such as head and neck, specifically gingival, breast, abdominal wall and various other areas including burn injuries [1,2], ADM has ingratiated itself as a promising development in a field whose chief goal is to reshape disfigured, aesthetically unsavory or damaged parts of the body. Even though synthetic products have been seen as beneficial, ADM is superior in it being a biological product, thus reducing the risk of rejection in ongoing recovery and beyond [2]. The key feature of ADM compared to prior biological technologies is that it is an allograft or xenograft from processed skin, devoid of cellular components.
The strategy is that the lack of these leads to reduced inflammation since they are the aspect in the immune response to lead to donor rejection [3]. The ultimate goal is for the ADM to be identified as host tissue, and thus should have a minimalist footprint: collagen and extracellular matrix components critical in wound healing. While products have a unique preparation method, AlloDerm being the first commercially described ADM, set the groundwork for its development. Typical steps include decellularization, dehydration, sterilization and incorporation [1].
In this report, a literature review was performed on a multitude of studies that strove to compare human and porcine (allograft and xenograft respectively) preparations of an ADM. There was a gross lack of such comparison studies, yet the importance in determining the difference in efficacy is 2-fold: (1) financial benefit of a xenograft and (2) spiritual and personal desires of patients to avoid allografts.
A systematic review is an essential tool in evidence-based medicine, in order to coalesce existing evidence spread throughout various literature, with a goal to remove conflict and streamline understanding of a medical or clinical problem. A key aspect of this method is reproducibility and thus reliability, particularly in a field with such a limited scope of research.
MATERIALS/PATIENTS AND METHODS
Searches were carried out across MEDLINE and Ovid, with a period of search of Ovid MEDLINE(R) 1946 and Embase Classic+Embase 1947, to January 30, 2019. A list of search terms is given in Table 1. The search was divided into population, intervention and outcomes. Following an extensive exclusion based on title, an abstract scrape was performed. Another exclusion was done by looking at the full text based on whether it is a review or abstract only.
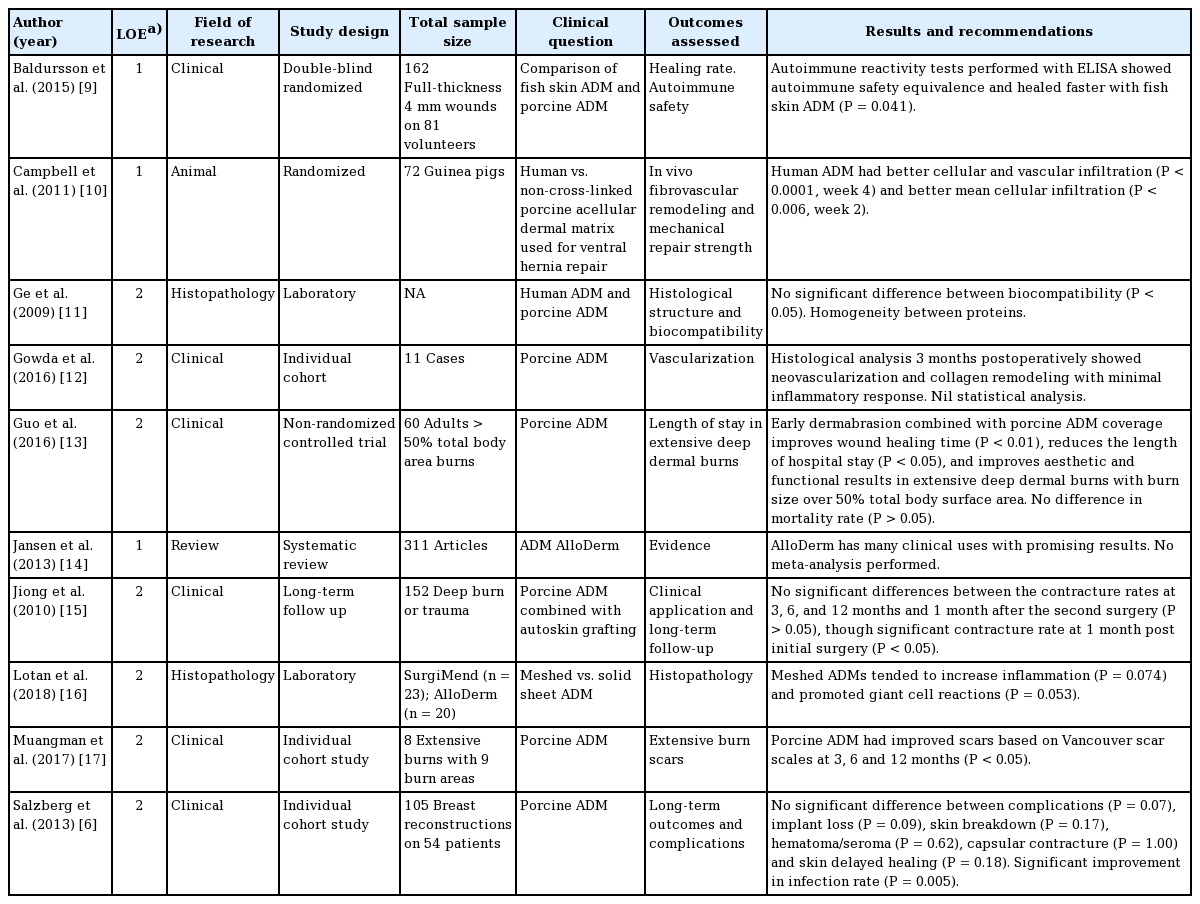
Description of included studies with level 1 and 2 evidence-based on the Oxford 2011 Levels of Evidence
Relevant sources were included based on their study type as well as relevance to the research topic through a bibliographic search and basic searching. There was categorical exclusion from data analysis based on the irrelevance due to lack of comparison of human and porcine models.
RESULTS
A broad search strategy was employed in order to prevent the exclusion of critical papers, particularly due to the lack of a cohesive naming structure in a novel and innovative medical technology. Exclusion by title was used primarily to exclude research that was not of relevance.
The literature search identified 278 studies which were then imported into the software Endnote X8 (Thomson Reuters, Toronto, ON, Canada) for purposes of reference management. Of these, 101 duplicates were removed and 14 additional studies were added through manual searches. A title search was performed to exclude irrelevant studies, resulting in exclusion of 91 studies. Of the remaining 191 studies, abstract review led to the exclusion of 49 resulting in a final 51 studies.
A PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) study was performed which can be seen in Fig. 1. Studies were assessed for quality through reading through the entire text and evaluating the methodologies based on criteria devised by the EQUATOR (Enhancing the QUAlity and Transparency Of health Research) network [4]. This left 29 primary studies to allow for the evaluation of the differences between human and porcine ADM where a table of “Description of included studies” was performed as shown in Table 1 where only level I and II evidence is included based on the Oxford CEBM levels of evidence [5].
DISCUSSION
The systematic review identified a small collection of studies from a broad range of domains with variable overlap. Distinctly, there was a pertinent lack in evidence surrounding the research question of this review. While Salzberg et al. (2013) [6] defined a comparison between Strattice and human ADM, a potential conflict of interest, and narrow scope (specifically for the use of porcine ADM in immediate breast reconstruction) suggests a limited level of relevance. It is however a good defining point for future studies that can compare porcine and human ADM more generally. Complications and outcomes were investigated with an average follow-up period of 3.5 years. It was found that there was nearly a 2-fold increase in the rates of complications (8.6% vs. 3.9%) which presented with a P-value of 0.07, suggesting a lack of statistical significance [6,7]. The exact nature of these calculations is not known to this author, and hence the relevance of the increase in complications should not be understated. Additionally, it is noted that there is 3-fold increase in the rate of implant loss, which was additionally not statistically significant (P = 0.09) [6]. It is noted that as porcine ADM is a xenograft as opposed to an allograft, there is the specific risk of graft rejection, even though all relevant epitopes that cause rejection have been removed in manufacture. Some cases were described as having erythema around the graft, even though there was no histological evidence of graft rejection [6]. The graft did however did not have a homogeneous cellular infiltration and revascularization though there does not seem to be a clinical relevance to this [6,8]. Needless to say, this does require further follow-up to better evaluate.
Histology
While outcomes and clinical relevance of porcine and human ADM are important, a histopathological understanding of the underlying mechanisms can give a new level of understand and evaluation to the comparison. There is not much viable research in the comparison [11,16], however, there is variable evidence in different preparation methods. Specifically, Lotan et al. (2018) noted that meshed ADM models promoted integration better than solid models. Consequently, a more in-depth study was initiated in order to evaluate the relevance of these findings on immediate, implant-based breast reconstruction. The key histological finding was that in a mesh, the underlying cells were better able to populate the matrix itself. Relevant research in the field supports the safety of this preparation as well [11,16,18].
Since the ambition of ADM is to improve wound healing, an understanding of the underlying healing mechanisms of the skin is relevant. Wound healing can be broken into inflammation, proliferation and maturation, with significant overlap between each of these stages. Type III collagen is the first to collect in inflammation, with amounts of it dropping 0, being replaced by type I collagen through proliferation and into maturation. Fibronectin follows a similar but broader trend to type III collagen, reaching completely loss about 9 days following wound creation. Initially various inflammatory mediators control the recovery of the wound, with fibroblasts becoming the main cell of function in proliferation [2,19,20].
Histologically, the goal of ADM is to promote rapid healing with a minimal scar. Previous attempts at using synthetic meshes were unable to provide wound healing units such as the required fibronectin to speed this process up. Due to the acellular nature of the products, there is reduced risk of rejection, but the consistent presence of a foreign body does lead them to infection and extrusion in certain scenarios. It has been noted that in non-crosslinked ADM products, there is faster degradation due to the effects of collagenases, while if there is excessive crosslinking, it may prevent suitable integration (meshed vs. solid ADM preparations) [2,16,21,22].
Uses of ADM
The general application of ADM for wound healing is very broad and varied. Unfortunately, there is limited prospective randomized data comparing the use of ADM to the gold standard of each of the procedures that it is replacing. There are consistently primary studies presenting innovative uses for ADM in surgery, but evidence base for these is too weak for suitable discussion. Common uses include: burns and wounds; abdominal wall procedures; reconstructive breast procedures; cosmetic breast procedures; and head and neck procedures [2].
In the case of burns, the value of an ADM is the ability to provide a matrix for integration of regenerating tissue, particularly in full-thickness wounds, where this natural matrix has been lost. AlloDerm has been shown to have good evidence for use, with some evidence for improved healing efficacy [2,17,23]. The cost of the product has been suggested as a limitation for widespread use, which supports the need to use xenografts [2]. Additionally, there is suitable evidence suggesting that the use of porcine ADM allows for suitable wound healing, reducing hospital stay, and has aesthetic benefits in extensive deep dermal burns over more than 50% total body area. Additionally, it has functional benefits [13]. It was noted that due to the properties of porcine ADM, it is able to support tissue regeneration, fibroblast activity, angiogenesis, and native tissue to regenerate. This study however performed early dermabrasion followed by porcine ADM application for wound closure, with the aim of accelerating wound healing. The benefit of the dermabrasion is to remove potentially devitalized tissue and any layers of dermis that may be colonized by pathogens [13,24].
In a surgery that involves the abdomen, the use of porcine ADM has been compared to human ADM for ventral hernia repair, although only performed on guinea pigs (hence not being a true measure of an allograft against a xenograft as it is effectively two xenografts) [10]. The goal of the study was to determine the early outcomes of the use of these materials with mechanical testing as well as immunohistologic analyses of the cellular and vascular levels. It was noted that both preparations had good host cell infiltration, but this was more significant in human ADM. It has become clear that more research is required in this area. Though there is evidence of effective vascularization following xenograft application in hernia repairs [12].
It has been noted however that allografts have a weaker tensile strength than porcine ADM in hernia repair [2,25,26]. It is apparent that the mesh should act as support for the wound rather than the actual bridge that links wound borders [2,27]. It is critical for surgeons using ADM regardless of manufacture to consider positioning of the ADM.
There is more extensive study in the field of ADM use in breast procedures. First described in 2001, the area has grown significantly for reconstructive as well as cosmetic breast procedures [1]. Specifically, in these cases, the role of the ADM is to act as an internal support to cover the implant permitting single stage reconstruction, with the placement of the final implant at the initial reconstruction [2,28,29]. It has been noted with relatively strong evidence that the use of a porcine ADM (Strattice) provides complication rates and outcomes similar to human ADM. As previously noted however, the complication rates are increased relative to human ADM with the use of porcine ADM, although this did not reach a level of statistical significance (but the relevance of the increase should not be neglected and should be studied further with higher powered studies) [7]. In the field of cosmetic breast procedures, it has been noted that ADM placement has strong natural contours, without major irregularities [2]. A unique application of porcine ADM has been in repair of Fournier’s gangrene. It has been noted that it promotes granulation tissue formation with permits the retention of function and morphology in the perineum and penis [30]. Clearly, there is significant room for investigation in more novel applications of ADM, with the role of porcine ADM not being understated.
Risks
Naturally the risks of usage of porcine ADM overlap with those of human ADM. These typically include infection and rejection risks, as well as failure or dehiscence of the wound. Other risks include delayed healing of the skin and skin breakdown or necrosis. While these are natural risks in human ADM, it has been seen to be slightly yet not statistically significantly increased in breast reconstructions [7]. Interestingly, it was seen that the use of fish ADM was more successful in increased healing rates than porcine ADM, though this is topic of another discussion [9].
As a unique approach to a risk of using ADM, Vedak et al. (2015) [31] noted that a delayed type IV hypersensitivity reaction in porcine ADM use can present as what appears as an infection. It was believed that there would not be a major host inflammatory response to a natural decellularized tissue such as human or porcine ADM, but this case shows that the potential for a hypersensitivity reaction should be considered as a potential diagnosis in postoperative infection cases. In this situation, the patient had to tolerate multiple debridements.
Benefits
The general benefits of ADM for wound healing are well documented and apparent. A natural method to promoting collagen I and III deposition as well as fibronectin, while promoting fibroblast infiltration into a matrix is clear [2,16]. When using porcine ADM as opposed to human ADM, the main benefit is cost-effectiveness. It is noted that for breast reconstructions or cosmetic surgery, the use of human ADM is a major deterrent due to the cost being footed by the patient. Additionally, a multitude of studies note that human ADM is realistically not costeffective, and concurrently porcine ADM is much more appropriate for an already overburdened healthcare system all around the world [1,2,6,32]. Naturally it is imperative to ascertain if there is any risk associated with the use of porcine ADM, which preliminarily seems to be clear.
Future recommendations
Porcine ADM as opposed to human ADM has not been studied extensively when it comes to outcomes and complications. It would be essential to perform more high-level research to formulate an evidence base for its more routine use. This research should present justifiable, reliable and replicable statistical analysis in order to provide opportunity for a meta-analysis to be performed in the future.
Further study could also be performed on more unique variants of ADM such as fish-based ADM which has shown some promising results [9].
CONCLUSIONS
ADM are a novel and highly successful tool for improving wound healing by creating a natural and biological base for wound regeneration through fibroblast invasion and appropriate component deposition. While there is a strong evidence base for human ADM, there is limited research in the comparison with xenografts such as porcine ADM. The benefit in using this would mainly be cost-effectiveness, with human ADM costs being a major deterrent for many patients and healthcare providers. Although there is not enough high-level evidence, preliminarily it is apparent that both an allograft and xenograft ADM can be used interchangeably, with the surgeon not needing to be worried of poorer outcomes or increased complications (although this needs more research). Robust statistical analysis is required in order to facilitate a strong meta-analysis in the future. Further studies would certainly improve patient care and outcomes for patients requiring improved wound repair and regeneration.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization, data curation, formal analysis: EC Saricilar. Methodology, project administration, visualization: EC Saricilar. Writing - original draft: EC Saricilar. Writing - review & editing: EC Saricilar, S Huang.