Evaluation and treatment of facial feminization surgery: part I. forehead, orbits, eyebrows, eyes, and nose
Article information
Abstract
Facial feminization surgery (FFS) incorporates aesthetic and craniofacial surgical principles and techniques to feminize masculine facial features and facilitate gender transitioning. A detailed understanding of the defining male and female facial characteristics is essential for success. In this first part of a two-part series, we discuss key aspects of the general preoperative consultation that should be considered when evaluating the prospective facial feminization patient. Assessment of the forehead, orbits, hairline, eyebrows, eyes, and nose and the associated procedures, including scalp advancement, supraorbital rim reduction, setback of the anterior table of the frontal sinus, rhinoplasty, and soft tissue modifications of the upper and midface are discussed. In the second part of this series, bony manipulation of the midface, mandible, and chin, as well as soft tissue modification of the nasolabial complex and chondrolaryngoplasty are discussed. Finally, a review of the literature on patient-reported outcomes in this population following FFS is provided.
INTRODUCTION
Facial gender confirmation surgery, commonly known as feminization surgery, incorporates aesthetic and craniofacial surgical principles and techniques to feminize masculine facial features and facilitate gender transitioning. The prioritization of facial feminization surgery (FFS) over other forms of gender reassignment surgery among transgender individuals reflects the important role it plays in gender dysphoria [1,2]. Studies such as those by Ainsworth and Spiegel [3], and more recently by Morrison et al. [4], have revealed its positive effects on mental health-related quality of life. Objective studies of public perception have also demonstrated significant differences in gender appearance from FFS beyond what hormone or non-surgical therapy can provide [5]. Though a majority of transgender individuals desire surgical transitioning, only 25% have access to do so [6]. Increasing awareness, scientific information sharing, and formal training in the field [7,8] will drive surgical innovation and patient advocacy to improve outcomes and address the unmet healthcare needs in this population.
FFS encompasses a broad range of procedures unique to transgender patients. In this review, we present an in-depth analysis of the current literature on FFS. This first section of a two-part series describes the preoperative evaluation process and focuses on management of the hairline, forehead, orbits, eyebrows, eyes, and nose.
GENERAL PREOPERATIVE EVALUATION
The World Professional Association for Transgender Health Standards of Care version 7 considers chest and genital surgery as medically necessary, but lacks set guidelines for the clinical evaluation and management of patients who wish to undergo FFS [9]. At our institution, patients undergoing FFS require preoperative evaluation by a multidisciplinary gender health team. The diagnosis of gender dysphoria is first determined by a gender health specialist or mental health provider. As gender dysphoria is highly individualized, the timing of medical and surgical transition varies among patients; some choose to undergo hormonal therapy for many years prior to FFS while others choose to have FFS as their first intervention in transitioning. Letters of support for FFS from a mental health provider as well as from the patient’s primary care physician or gender health specialist, albeit not explicitly required for insurance approval, are frequently used to demonstrate the medical necessity of FFS for the patient. Preoperative clearance by a primary care provider is typically desired.
At the time of consultation, a discussion about the patient’s ideal features and goals as well as the risks, benefits, expectations, and limitations of surgery must be carried out [10]. A thorough physical examination should be performed, including assessment of facial anthropometrics, ascertaining baseline neuromuscular function, and obtaining standardized preoperative photographs. It is important to remember that many of the “standard” measurements reported in the literature are based on Caucasian profiles and therefore ethnicity and age should be taken into consideration during the planning phase [11].
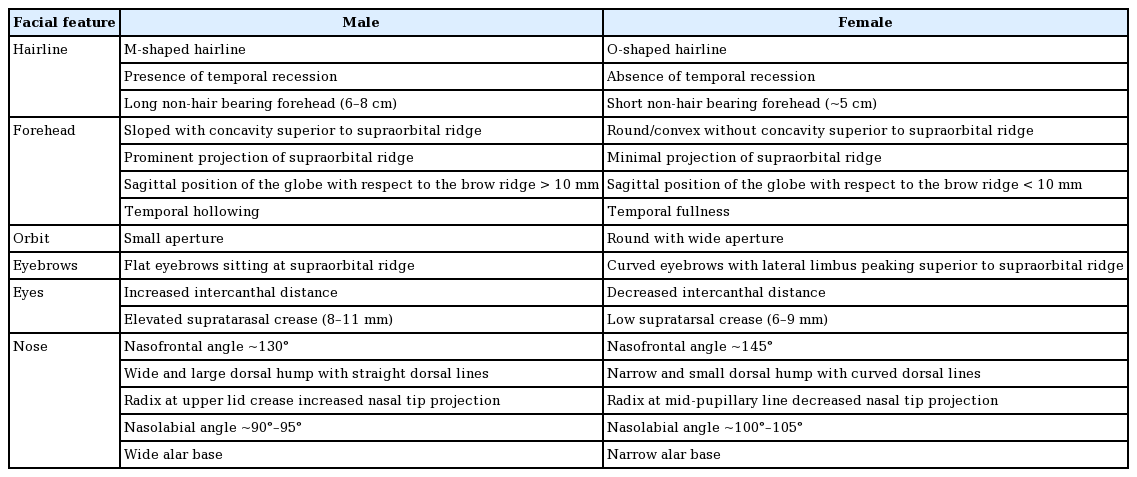
For individuals requiring bony manipulation, a fine-cut, non-contrast craniofacial computed tomography scan from the vertex to the hyoid bone is helpful to map the bony framework. Virtual surgical planning may further assist with craniofacial anatomical mapping by developing prefabricated cutting guides and models that facilitate planning, reduce operating time, and improve outcomes [12-14]. Recently, our group published a method of simplification of FFS via modeling on a reference female skull [12]. The key anthropomorphic differences between the upper two-thirds of the male and female faces are outlined in Table 1 and Fig. 1.
FOREHEAD AND ORBITS
Clinical evaluation
The clinical exam of the forehead begins with the hairline. While the male hairline typically has a characteristic M-shape secondary to male-pattern hair loss, the female hairline is often rounded. The mean length of the non-hair-bearing forehead for males is approximately 6.6 cm compared to 5 cm in females [15].
On lateral view, the male forehead tends to slope flatly down to a prominence at the superior orbital ridge. On sagittal view, the orbit is typically measured at 10 mm (or more) posterior to the superior orbital ridge. In contrast, the female forehead is flat or slightly convex with the orbit less than 10 mm posterior to the superior orbital ridge on sagittal view [15]. Additionally, the female orbit is round with a wider aperture than the male, producing a softer appearance [16,17]. Gender differences in the forehead soft tissue are also apparent, as females tend to have less temporal hollowing compared to males [18]. Dimensions of the frontal sinus and thickness of the anterior table can be determined from preoperative computed tomography scans prior to surgery. Forehead morphology and recommended management can be classified according to Ousterhout (Fig. 2) [15].
Forehead classification according to Ousterhout [15]. (A) Type I forehead morphology (8%–9%) is characterized by a mild to moderate projection of the brow, thickened layer of bone anterior to the frontal sinus, and possible absence of the frontal sinuses. The desired contour is achieved with burring alone. (B) Type II (8%–9%) forehead morphology includes mild to moderate projection of the brow, a thin anterior table of the frontal sinus, and a possible area of concavity superior to the supraorbital rim. Treatment options include burring of frontal bossing (but special care to not enter the frontal sinus) or augmentation of the concavity. (C) Type III (82%) forehead morphology includes an excessive anterior projection of the brows and treatment consists of osteotomy and setback of anterior table of the frontal sinus. (D) Type IV (1%) forehead morphology is characterized by a severely diminutive forehead and treatment requires augmentation of the entire forehead.
Hairline advancement, frontal bone reduction, and orbit manipulation
Hairline advancement and frontal bone reduction is generally performed simultaneously, though both procedures have significant variations according to surgeon preference. In the process of altering the frontal bone, the orbit is also manipulated to achieve a more feminine appearance.
When indicated, hairline advancement reduces the length of the non-hair-bearing forehead through a pretrichial coronal incision extending posteriorly in the temporal scalp and inferiorly down to the post-auricular region [19]. The dissection proceeds posteriorly in either a subgaleal or subperiosteal plane to the occiput in order to maximally advance the scalp. Galeotomies and intraoperative tissue expansion can be utilized to gain further advancement, although care must be taken to preserve the scalp vascular plexus in the subcutaneous connective tissue layer. Anterior dissection is also performed to expose the frontal bone just distal to the nasofrontal junction, superior orbital rims, and zygomaticofrontal sutures. Care must be taken to avoid injury to the frontal branch of the facial nerve lying superficial to the deep temporal fascia during the dissection over the temporal scalp.
Other techniques to modify the hairline include simultaneous hair transplantation with forehead reconstruction using two modified coronal approaches [20,21]. There are some differing opinions with respect to the timing of hair transplantation, with some groups recommending immediate transplantation [20] and others suggesting that deferred hair transplantation improves engraftment rates [22] and results in fewer complications [19,23]. Although some argue that hair transplantation is superior to hairline lowering surgery [20], a consensus has not been reached.
In the absence of any need for hairline lowering, a typical bicoronal incision is performed. Regardless of incision design, management of the frontal bone is often based off the standardized approach described by Ousterhout’s classification (Fig. 2) [15]. Group I foreheads (8%–9% of patients) have mild brow bossing, thus burring alone is sufficient for correction. Group II foreheads (8%–9%) have moderate forehead and brow bossing with characteristic flattening superiorly. These patients require a combination of burring with augmentation of the flattened portion with autologous or allogenic substances. Group III foreheads (82%) have moderate to severe forehead and brow bossing, requiring an osteotomy of the anterior table of the forehead and setback, in addition to burring of the superior orbital rim (Fig. 3) [3]. Lastly, group IV foreheads (1%) [24] are characterized by such a slope that setback cannot achieve the necessary contour. Thus, augmentation with autogenous bone or with alloplastic materials, such as methylmethacrylate, polyethylene, or hydroxyapatite cement, is needed to establish forehead convexity [15,25-27]. In the senior author’s (JCL) experience, 90% of patients require frontal bone osteotomy and setback.
Type III anterior table of the frontal sinus setback. In the majority of patients, the type III forehead operation as described by Ousterhout will be necessary. In this operation, the anterior table of the frontal sinus is osteotomized and reshaped on the backtable to flatten the contour (black arrow). Simultaneously, the frontal bone is contoured and the superior orbital rims are reduced laterally to the zygomaticofrontal suture. Medially, the radix is reduced to ensure a smooth transition between the frontal bone and the nose. Following completion of frontal bone contouring, the anterior table is replaced and stabilized with titanium plates and screws in its new setback position.
Temples and soft tissue
Temporal fossa augmentation can be achieved with either hyaluronic acid fillers, autologous fat, or implants [28]. Patients may also elect for myectomies of the galea-frontalis, procerus, and corrugator muscles to further reduce wrinkling of the forehead, minimize prominence of the muscles, and facilitate facial rejuvenation and feminization [29].
Manipulation of the frontal sinus and forehead recontouring should be carried out with proper care and training to avoid postoperative complications. Temporary paresthesia in the distribution of the supraorbital nerves and edema of the upper eyelid are common. Cerebrospinal fluid rhinorrhea may also occur if the frontal sinus osteotomy is too high, damaging the dura and penetrating the posterior table [30]. While infection rates or mucocele formation appear to be low [23], latent mucoceles may go undetected until several years after surgical manipulation of the sinus [31]. Future studies focusing on the long-term effects of frontal sinus setback and role of sinus functionalization are necessary to better characterize these potential complications.
EYEBROWS AND EYES
Clinical evaluation
Male eyebrow morphology tends to be straight and flat, sitting at the level of the supraorbital ridge with increased intercanthal distance compared to females [19,32]. The female eyebrow is curved in shape and tends to sit superior to the supraorbital ridge [19], peaking at approximately 1 cm above the ridge at the lateral limbus with a positive canthal tilt [33]. In Caucasian males, the supratarsal crease lies 8–11 mm above the upper eyelid, while in Caucasian females, the distance is about 6–9 mm [32]. Ethnic considerations must be noted during evaluation and operative planning to preserve the patient’s ethnic identity [34,35].
Eyebrows
Although the brows are naturally modified during bony reduction of the supraorbital ridge and when the hairline is lowered via skin excision, a brow lift can better control brow morphology to achieve a more feminine appearance [36]. A number of methods have been reported to supplement temporal brow lifting from soft tissue excision. Our group prefers to use suture suspension with bone channels created in the outer table of the frontal bone superior to the brows beneath the hairline. Others have described brow lift techniques using various forms of suture anchors [37].
Eyes
While bony modifications of the orbital rims during forehead recontouring augment the appearance of the eyes, soft tissue modifications to this region may be beneficial as a supplementary procedure for certain patients. A lateral canthopexy can change canthal tilt to achieve a more feminine appearance [33,38]. While not specifically for the purposes of gender affirmation, both upper and lower blepharoplasties may be beneficial for optimal results in older patients.
NOSE
Clinical evaluation
Feminization of the nose requires a detailed understanding of the conventional aesthetics of the nose, knowledge of key anatomical differences between males and females, and functional considerations [39,40]. The most prominent features of the male nose include a wide nasal bones, nostril flaring, a nasofrontal angle of approximately 130°, a higher radix positioned at the upper lid crease, and a nasolabial angle of approximately 90° [41,42]. The female nose has a nasofrontal angle closer to 145° with a radix closer to the mid-pupillary level, and an obtuse nasolabial angle. The male nasal tip is also projected approximately 5 mm more than the female nasal tip [43].
General surgical considerations
The approach to the feminizing rhinoplasty, as in any procedure, is dictated by the desired anatomical changes and the exposure needed to achieve the desired results. While an open rhinoplasty can provide easy access to the bony and cartilaginous framework of the nose, a closed approach may be sufficient in certain cases. A reduction of the dorsum is typically required and should be accompanied by adjunctive maneuvers to preserve internal and external nasal valve function [44,45]. Classic rhinoplasty reduction techniques alone, without these additional supportive measures, may risk long-term complications in the FFS patient, especially given the degree of reduction often needed [39]. It is therefore critical that any preoperative functional issues related to a deviated septum, nasal valve incompetence, and turbinate hypertrophy be identified and potentially included in the operative plan as any intervention may exacerbate underlying problems.
Radix and dorsum
At the same time as anterior table setback, the radix is typically reduced such that a smooth transition may be achieved between the frontal bone and the nose. The reduction of the radix is generally one of the more unique maneuvers of the reduction rhinoplasty in facial feminization as this is approached superiorly from the coronal approach rather than from the typical rhinoplasty approach. Depending on the patient, dorsal reduction is frequently necessary due to the overall projection of the more masculine nose compared to feminine noses. Berli and Loyo [42] suggested that the goal of dorsal reduction should be a nasal dorsum approximately 1–2 mm posterior to an imaginary line between the ideal nasal tip and the nasion.
Nasal tip projection and the nasolabial angle
The goals of nasal tip refinement include decreasing nasal tip projection, decreasing nasal width, and increasing tip rotation [42]. Typical techniques used to modify and rotate the nasal tip are those common to conventional aesthetic rhinoplasties, including resecting cephalic margins of the lower lateral crura to decrease projection, transdomal and intradomal sutures to narrow the tip, and modifications of the caudal septum, septal extension grafting, or columella strut grafting to rotate the tip and increase the nasolabial angle [46]. Frequently, for the purposes of stability in the change in tip rotation, particularly in the setting of a combined reduction rhinoplasty with upper lip lift, rib cartilage autograft or allograft will be necessary as a septal extension graft or columella strut.
Width reduction
Both the nasal bones and the alar base are wider in masculine noses compared to feminine noses. Hence, osteotomies are generally needed. Alar base width reduction via Weir and or sill excisions is typically undertaken when the alar base width is greater than intercanthal distance [42] and is the last step in the FFS rhinoplasty. Alar flaring can occur secondary to radical reduction of the nasal tip, requiring an alar base reduction during the initial operation. At the same time, aggressive resection is needed to decrease projection and alar flaring may risk alar retraction and collapse. Thus, prophylactic alar rim grafts may be necessary to maintain nasal aesthetics and external valve competence [42].
CONCLUSIONS
FFS is a rapidly progressing field that plays an important role during the gender transitioning process. As the face drives gender identification, understanding the hard and soft tissue differences between males and females as well as the wide variety of techniques used to transition is essential to optimize outcomes. Further, extensive preoperative evaluation by a multidisciplinary team is crucial for surgical planning and to ensure that the needs of patients are addressed adequately prior to and after surgery.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization: BN Dang, Justine C. Lee. Methodology: BN Dang, Justine C. Lee. Writing - original draft: BN Dang, AC Hu, AA Bertrand, CH Chan, NS Jain, MJ Pfaff, James C. Lee, Justine C. Lee. Writing - review & editing: BN Dang, AC Hu, AA Bertrand, CH Chan, NS Jain, MJ Pfaff, James C. Lee, Justine C. Lee