Excisional lipectomy versus liposuction in HIV-associated lipodystrophy
Article information
Abstract
Background
Human immunodeficiency virus (HIV)-associated lipodystrophy is a known consequence of long-term highly active antiretroviral therapy (HAART). However, a significant number of patients on HAART therapy were left with the stigmata of complications, including fat redistribution. Few studies have described the successful removal of focal areas of lipohypertrophy with successful outcomes. This manuscript reviews the outcomes of excisional lipectomy versus liposuction for HIV-associated cervicodorsal lipodystrophy.
Methods
We performed a 15-year retrospective review of HIV-positive patients with lipodystrophy. Patients were identified by query of secure operative logs. Data collected included demographics, medications, comorbidities, duration of HIV, surgical intervention type, pertinent laboratory values, and the amount of tissue removed.
Results
Nine male patients with HIV-associated lipodystrophy underwent a total of 17 procedures. Of the patients who underwent liposuction initially (n=5), 60% (n=3) experienced a recurrence. There were a total of three cases of primary liposuction followed by excisional lipectomy. One hundred percent of these cases were noted to have a recurrence postoperatively, and there was one case of seroma formation. Of the subjects who underwent excisional lipectomy (n=4), there were no documented recurrences; however, one patient’s postoperative course was complicated by seroma formation.
Conclusions
HIV-associated lipodystrophy is a disfiguring complication of HAART therapy with significant morbidity. Given the limitations of liposuction alone as the primary intervention, excisional lipectomy is recommended as the primary treatment. Liposuction may be used for better contouring and for subsequent procedures. While there is a slightly higher risk for complications, adjunctive techniques such as quilting sutures and placement of drains may be used in conjunction with excisional lipectomy.
INTRODUCTION
Highly active antiretroviral therapies (HAART) are efficacious treatment options for patients with human immunodeficiency virus (HIV) or acquired immunodeficiency syndrome (AIDS), reducing HIV-related mortality by 50% to 80% [1]. Traditional HAART is composed of a triple (or more) combination drug therapy of nucleoside/nucleotide reverse transcriptase inhibitors (NRTIs), non-nucleoside reverse transcriptase inhibitors (NNRTIs), protease inhibitors, integrase strand transfer inhibitors, and fusion inhibitors. However, patients reliant on these medications face an increased risk of developing metabolic disturbances, including fat redistribution, dyslipidemia, insulin resistance, lactic acidemia, and abnormalities in bone mineral metabolism. This risk is significantly elevated in patient groups who also take NRTIs and protease inhibitors. Several of these conditions, specifically HIV lipodystrophy, pose a unique challenge to clinicians owing to complex metabolic abnormalities and disfiguring clinical features [2,3].
First documented by Carr et al. in 1998 [4], HIV-associated lipodystrophy syndrome is frequently seen in patients on longterm HAART. In this condition, patients suffer from metabolic abnormalities which cause unique clinical features. Physiologically, patients have hyperlipidemia, insulin resistance, and lactic acidemia. Externally this condition manifests with lipoatrophy of subcutaneous adipose tissue, especially in the face, limbs, and buttocks, and accumulation of visceral adipose tissue in the intra-abdominal, breast, and dorsocervical regions [5]. Impacting a large percentage of these patients, HIV-associated lipodystrophy has a documented prevalence of up to 80% in cross-sectional cohort studies with reports of 17% prevalence in 18 months after treatment initiation [6-8].
Unfortunately, medical and surgical treatment options for HIV lipodystrophy are limited. Medical management aims to limit the cardiovascular sequelae of dyslipidemia and insulin resistance. Often these therapies include switching antiretroviral drug regimens to combinations that exclude a class of drug believed to have contributed to the lipodystrophy and therapies designed to improve or reverse specific abnormalities (hypertriglyceridemia, insulin resistance, cholesterol, etc.). However, since HIV-associated lipodystrophy’s pathophysiology has yet to be elucidated, medical management has not found a treatment to prevent, mitigate, or reverse this condition.
Surgical approaches aim to provide short-term functional and aesthetic improvement. In carefully selected patient populations, surgical treatments have shown encouraging results in addressing soft tissue hypertrophy and atrophy. However, few studies have described the successful removal of focal areas of lipohypertrophy with successful outcomes. This manuscript reviews the outcomes of excisional lipectomy versus liposuction for HIV-associated cervicodorsal lipodystrophy over 15 years.
METHODS
Patient population
The Veterans Affairs Long Beach Healthcare System Institutional Review Board approved this single-center retrospective review of plastic surgery patients with HIV cervicodorsal lipohypertrophy. From January 2002 to October 2017, nine consecutive subjects with HIV-associated lipodystrophy underwent 17 procedures including a combination of excisional lipectomy and liposuction for management of cervicodorsal lipohypertrophy. All nine subjects were male veterans. All patients developed HIV lipodystrophy. The type of surgical intervention, pertinent laboratory values, and the amount of tissue removed were reviewed. Additional information regarding complications, recurrence, duration of follow-up, and placement of drain and quilting sutures in excisional lipectomy cases was gathered. Unfortunately, photography of before and after results were not readily available and thus excluded from analysis.
Preoperative evaluation
Patients with HIV-associated lipodystrophy actively or previously on HAART therapy were assessed for morphologic changes. Patients were considered for surgery if they presented with a chief complaint regarding the cervicodorsal lipohypertrophy. These patients were symptomatic from their lipodystrophy and complained of discomfort and altered quality of life. They were medically optimized with stable HIV disease on HAART therapy. The patients must have demonstrated realistic expectations, reliability, and compliance with previous medical management. The selection of the procedure was based on the nature of the lipohypertrophy. The more diffuse fibrofatty tissue was more likely to be addressed with liposuction; the discrete and defined lipohypertrophy was more likely to be addressed with excisional lipectomy. Recurrence was primarily identified by patients as a recurrent mass in the surgical area after at least 6 months after the initial procedure.
Excisional lipectomy technique
A midline vertical or horizontal incision was made and carried down to the subcutaneous tissue. Skin and subcutaneous tissue flaps were elevated lateral to the cervicodorsal fat pad and the hypertrophied fat was resected. A large Jackson-Pratt suction drain was then placed through a lateral stab incision and secured when large volume of fat was removed. Quilting sutures were used to close the dead space at the discretion of the attending surgeon. The midline skin was closed in layers. Compressive dressings and garments were then applied.
Liposuction technique
The cervicodorsal lipohypertrophy was removed via suctionand vibration amplification of sound energy at resonance (VASER)-assisted lipectomy with super wet technique through superolateral and inferolateral access sites. The endpoints for VASER-assisted lipectomy were time and loss of resistance, while the endpoint for suction-assisted lipectomy was bloodtinged lipoaspirate. Closed suction drains were placed in cases with high lipoaspirate volumes at the discretion of the attending surgeon. Compressive dressings and garments were also used to minimize the risk of serum formation, assist with skin redraping, and improve final contour.
RESULTS
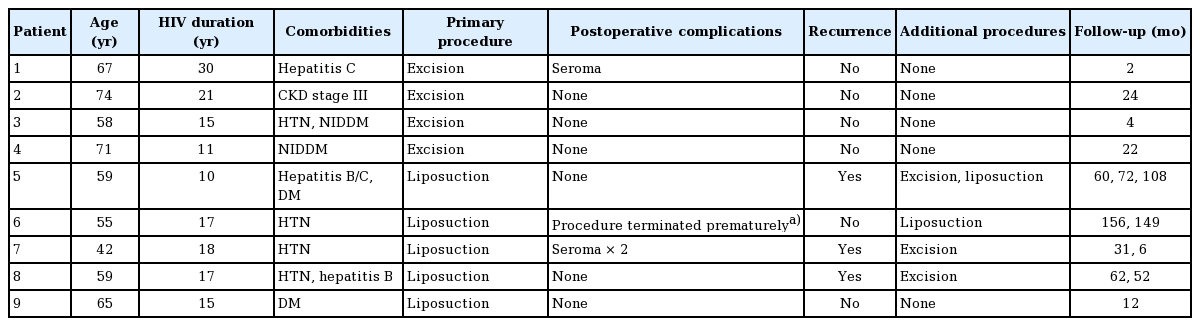
During the 15-year study period, nine male subjects with HIV-associated lipodystrophy underwent a total of 17 procedures addressing their cervicodorsal lipohypertrophy. At the primary procedure, patients’ mean age was 60.7 years (standard deviation [SD], 9.2 years; range, 42–74 years) with a mean duration of HIV of 16.7 years (SD, 6.2 years; range, 6–30 years). Mean follow-up across all procedures was 4.5 years (range, 2 months to 13 years) (Table 1).
Between the nine patients, there were nine primary procedures, four secondary/tertiary procedures, and four subsequent procedures for complications in subjects with stable viral titers and optimized CD4+ cell counts. In the subgroup of patients who needed a secondary/tertiary procedure, the average age was 54.3 years old (SD, 5.6 years; range, 45–60 years) with a mean duration of HIV of 16.3 years (SD, 4.3 years; range, 9–20 years). Mean time between primary and secondary treatment was 1.2 years. Overall, patients who required a secondary procedure were younger and had HIV for a shorter duration. All patients who needed a secondary procedure had liposuction as the primary procedure.
Of the patients who underwent liposuction alone (n = 5), 80% (n = 4) experienced a recurrence; however, one patient’s postoperative course was complicated by seroma formation. Lipoaspirate volume ranged from 50 to 350 mL. Of the subjects who underwent excisional lipectomy (n = 4), there were no documented recurrences; however, two patients’ postoperative courses were complicated by seroma formation. There was one patient who had primary liposuction, secondary excisional lipectomy, and tertiary liposuction. This patient also developed seroma formation after both the liposuction and excisional lipectomy, respectively. There were a total of three cases of primary liposuction followed by excisional lipectomy. One hundred percent of these cases were noted to have a recurrence postoperatively, and there was one case of seroma formation requiring evacuation within 6 weeks of initial surgery. Of the seven excisional lipectomy procedures, drains were placed in two cases, quilting sutures in one case, and both quilting sutures and drain placement in one case. There was one excisional lipectomy procedure documented without the use of quilting sutures or drain placement. Postoperative seroma formation was noted in one patient with drain only, one patient with quilting only, and no seroma formation with both drain placement and quilting sutures.
DISCUSSION
According to the Joint United Nations Programme on HIV/AIDS, there were approximately 36.7 million people worldwide living with HIV/AIDS at the end of 2016 [9]. As of July 2017, 20.9 million people living with HIV were accessing HAART globally. Suppression of viral replication by HAART and subsequent increases in CD4+ cell counts have led to an increase in disease-free survival. However, there are metabolic complications and disfiguring morphologic changes in patients receiving these therapies, first described by Carr et al. in 1998 [4]. Studies have reported the prevalence of HIV-associated lipodystrophy syndrome varying from 20% to 80% in HIV patients on HAART therapy, threatening compliance with therapy [10]. They demonstrated an association with several metabolic disorders including increased triglycerides, hypercholesterolemia, insulin resistance, and lactic acidosis. This phenomenon can be attributed to mitochondrial dysfunction and cortisol activation, which have been linked to the mitochondrial toxicity induced by certain HAART therapies. Studies have demonstrated depletion in mitochondrial DNA and mitochondrial dysfunction do not reverse completely, even after treatment has been discontinued [1,11-13].
Mallon et al. [6] described altered fat redistribution with lipohypertrophy, involving the neck, trunk, and breasts, and lipoatrophy, most pronounced in the face, arms, and legs. The frequency of cervicodorsal lipohypertrophy has been reported to range from 2% to 13%, with a higher prevalence (6%–13%) in patients with additional features of the lipodystrophy syndrome. Guallar et al. [14] reported the UCP1, the gene marker for brown fat, expression as a disturbance that is highly specific to “buffalo hump” adipose tissue, not shared by lipoatrophic subcutaneous adipose tissue from patients equally infected by HIV treated with HAART. They concluded that alterations in the white-versus-brown differentiation pattern of adipocytes characteristic feature only of “buffalo hump” and not a common feature of adipose tissue disturbances associated with HAART. There is no difference in the appearance of fat in vivo. In addition, these researchers found unaltered inflammatory status and adipogenesis of the buffalo hump adipose [14].
The implications of lipodystrophy including risk of metabolic diseases, quality of life, and adherence are considerable, especially in resource-limited settings [1]. Medical management of the fat redistribution including antiretroviral substitutions, imitation of metabolic agents, addition of growth hormone or testosterone, supplementation with antioxidants or mitochondrial cofactors, and exercise have been studied [15]. Diet and exercise are typically well tolerated and confer other health benefits; they are recommended in the initial treatment approach to lipohypertrophy [11]. Studies of the peroxisome proliferator-activated receptor-gamma agonist rosiglitazone and metformin in HIV infected patients with insulin resistance may have beneficial effects on visceral fat accumulation; however, the results are not consistent [16]. Leung and Glesby [11] found the analogues of the growth hormone/growth hormone-releasing hormone axis, like tesamorelin, have shown the most promising results in reducing visceral adipose tissue [17].
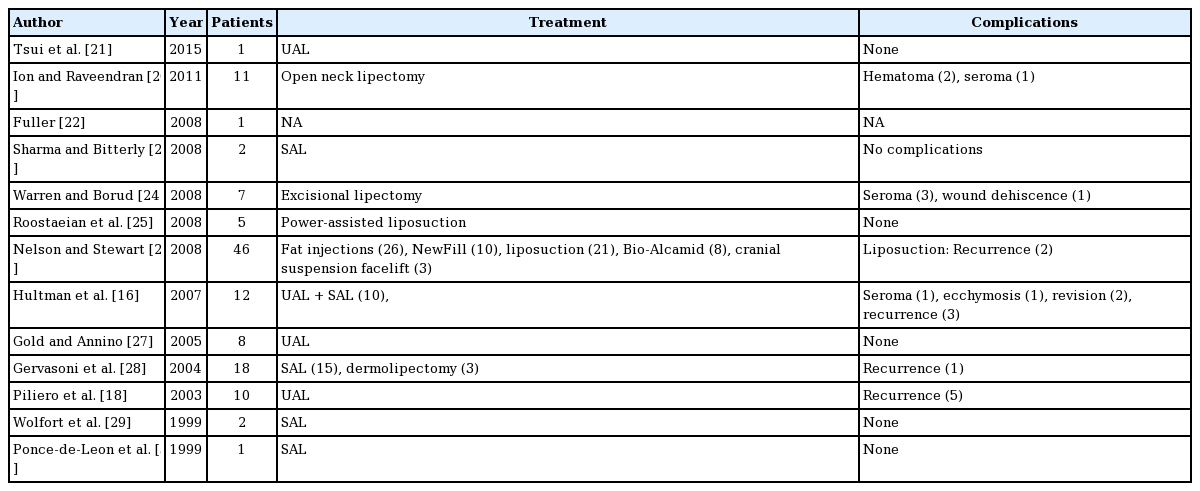
This study demonstrates lower rates of recurrence when cervicodorsal lipohypertrophy is initially managed with excisional lipectomy as opposed to initial liposuction. These findings are consistent with the literature, which suggests the hypertrophied fat found in the HIV-associated lipodystrophy patients is very fibrous, making passage of the liposuction cannulas quite challenging. Also, liposuction alone may involve insufficient removal of abnormal cervicodorsal fat. This theoretically allows for hyperplasia and subsequent hypertrophy of remaining adipocytes, thus causing reaccumulation of the cervicodorsal fat pad. The use of ultrasonography-assisted liposuction (UAL) was studied by Piliero et al. [18] in a study cohort of 10 HIV-positive patients with cervicodorsal lipodystrophy. They found UAL was well tolerated and effective treatment modality in addressing the lipohypertrophy in this area. Overall, one-half of patients achieved a sustained reduction in the size of the cervicodorsal lipohypertrophy after UAL treatment; however, recurrence was common. Table 2 summarizes the findings from a review of the literature.
In our cohort, while seroma formation was rare, excision carries a slightly higher risk of seroma formation when compared to liposuction. The risk may be decreased in excisional lipectomy cases when quilting sutures and drains are used in conjunction. A prospective, adequately powered study would be necessary to conclude a statistically significant difference in seroma rate when combining these additional modalities with excisional lipectomy. In the literature, there is controversy over risk factors and preventative methods for seroma formation. Magann et al. [19] found no difference in the subsequent risk of wound complications when no closure of the subcutaneous tissue layers occurs versus suture closure or a closed drainage system. At this time, the exact pathophysiology of seroma formation is not well characterized.
Hultman et al. [16] reviewed combined data from 11 different studies and revealed 88 patients who underwent surgical removal of fat in the anterior and posterior neck, torso, and breasts. The overall rate of reported complications was found to be approximately 26.1%, and the recurrence rate in 72 patients available for follow-up was 23.6%. The length of follow-up was reported in four studies, ranging from 12 to 30 months. Ion and Raveendran [20] found the open anterior cervicoplasty with subplatysma contouring a powerful tool for predictable and safe results addressing HIV-related anterior anterolateral neck lipohypertrophy.
Hultman et al. [16] also provided clinical guidelines to consider when determining the surgical management of HIV-associated lipodystrophy. They highlighted the importance of the patient truly understanding that the role of surgery as a primary or adjunctive modality has not been completely defined. Surgery should only be offered to patients with stable HIV infection with realistic expectations regarding outcomes. These patients must also have focal accumulations of fat amenable to liposuction or lipectomy. Informed consent process must include the understanding of suboptimal correction or recurrence of lipohypertrophy. This may involve staged or late reoperation if necessary.
This study has several limitations in addition to those inherent in a single-institution retrospective review. Because this review involved a retrospective cohort study over a 15-year period, there were deviations in the surgical technique, and attending discretion was often used to determine the surgical intervention that was pursued. Moreover, patient satisfaction is notably separate from clinical outcome and deserves to be further investigated. Patient postoperative satisfaction is often multifactorial and must be properly surveyed with a validated questionnaire. The generalizability of the study is limited by the small number of subjects; however, this study represents the largest reported case series addressing the surgical management of HIV cervicodorsal lipohypertrophy.
HIV-associated lipodystrophy is a disfiguring complication of long-term antiretroviral therapy with significant morbidity. Given the limitations of liposuction alone as the primary intervention, excisional lipectomy is recommended as the primary treatment for correction of this deformity. Liposuction may be used for better contouring and for subsequent procedures. While there is a slightly higher risk for complications, adjunctive techniques such as quilting sutures and placement of drains may be used in conjunction with excisional lipectomy.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Ethical approval
The study was approved by the Institutional Review Board of Veterans Affairs Long Beach Healthcare System (IRB No. 1455) and performed in accordance with the principles of the Declaration of Helsinki. Informed consent was obtained.
Author contribution
Conceptualization: G Evans. Data curation: N Barton, R Moore, K Prasad. Formal analysis: N Barton, R Moore, K Prasad, G Evans. Methodology: N Barton, R Moore, G Evans. Project administration: N Barton, G Evans. Visualization: N Barton, R Moore, K Prasad, G Evans. Writing - original draft: N Barton, R Moore, K Prasad, G Evans. Writing - review & editing: N Barton, R Moore, K Prasad, G Evans