Evaluation and treatment of facial feminization surgery: part II. lips, midface, mandible, chin, and laryngeal prominence
Article information
Abstract
Facial feminization surgery (FFS) refers to a set of procedures aimed at altering the features of a masculine face to achieve a more feminine appearance. In the second part of this twopart series, assessment and operations involving the midface, mandible, and chin, as well as soft tissue modification of the nasolabial complex and chondrolaryngoplasty, are discussed. Finally, we provide a review of the literature on patient-reported outcomes in this population following FFS and suggest a path forward to optimize care for FFS patients.
INTRODUCTION
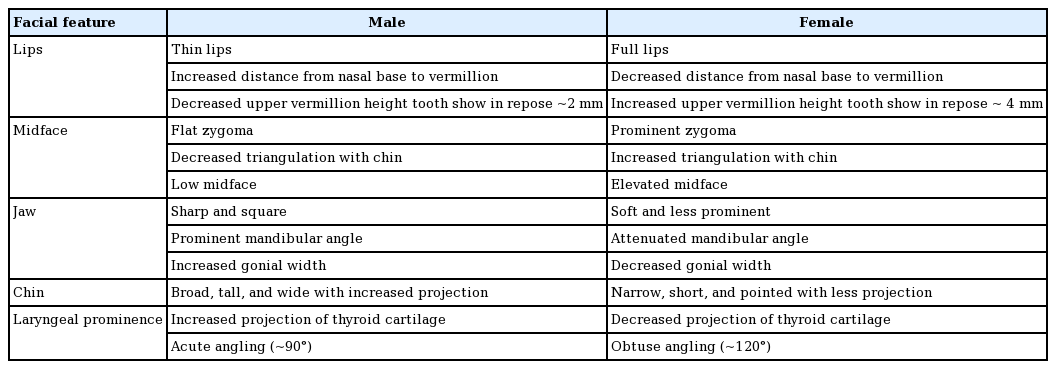
Facial feminization surgery (FFS) is an essential component of the transitioning process in improving mental health-related quality of life (QoL) in transgender women [1,2]. As the prevalence of FFS grows, evidence-based practices are needed to optimize surgical and QoL outcomes. Here, we present a review of the current available literature on facial feminization surgical and non-surgical techniques. For this second part of our two-part series, we focus on the lips, midface, jaw, chin, and laryngeal prominence. We also comment on the current state of postoperative outcomes. An overview of the anatomical differences between the lower male and female face are outlined in Table 1 and Fig. 1.
LIPS
Clinical evaluation
The ideal ratio of philtrum to upper labial height is approximately 3:1 in females [3], with the lower vermilion thicker than upper [4]. In males, the ratio is greater due to an increased philtrum length [5], and the lips are thinner [6]. Normal female tooth show in repose is approximately 4 mm, while in males it is approximately 2 mm [5].
Evaluation of the lips includes the hair-bearing skin under the nose, the red vermillion, and the oral mucosa [7]. Surgical goals include shortening the columellar-lip distance while everting the red vermillion to provide a fuller lip [7] and increasing dental show [8].
Surgical technique
The lip lift for FFS has been described by Salibian and Bluebond-Langner [7] and Altman [8] among others. Through the “bullhorn” technique (Fig. 2), a portion of the white lip is excised in the shape of a bull’s horn [9]. Full thickness skin and tissue is removed in a wedge to the level of the orbicularis oris, which “rolls-out” the upper lip to increase the perceived fullness [10]. The width of the dissection depends on the amount of tissue necessary to be removed for shortening to approximate a 3:1 ratio of philtrum to upper labial height. However, it is important that no more than 25% of the original philtral distance is removed since over-correction can disrupt the balance of the lower face [7,8] and increase the risk of producing a gummy smile. Upon closure, sutures are placed medially first and then extend laterally to medialize the upper lips and preserve fullness of the philtrum [10].

Upper lip lift. For some patients, a portion of the white part of the upper lip is removed in the shape of a bull’s horn. Full thickness skin and tissue is excised to achieve an ideal ratio of 3:1 between philtral and upper labial height. This also rolls out the upper lip to increase its perceived fullness.
Various modifications to the lip lift have been developed to improve aesthetics [10], address scarring [11], and minimize the size and number of incisions [12]. One such modification, in which an incision is created along the alar grooves, lifts the lateral lip more than the medial [13]. Another modification has been used in patients with widened columellas, where two separate incisions are extended into the nose medially, rather than one continuous subnasal incision, to prevent the formation of an overly-visible scar [13]. Further, the transcolumellar incision may be modified such that only a single incision is required for both a lip lift and simultaneous open rhinoplasty [14].
In addition to the lip lift, direct volume enhancement of the lips can be considered. Fillers [15,16], autologous fat grafting [17], and dermal grafts [8] are all commonly utilized methods to provide shape to the upper lips and augment the upper vermillion border.
MIDFACE
Clinical evaluation
In comparison to the female midface, the male midface has a flatter zygoma, with less projection. This results in less triangulation with the chin on profile, as opposed to the increased triangulation in female faces resulting in the classic “heart-shape” [6,18]. Additionally, the female midface sits higher with increased malar definition.
In addition to the bony tissues of the midface [19], particular attention should be given to the soft tissues as it is suggested that the main difference between the appearance of the male and female midface may be the greater concentration of fatty soft tissue in the malar and temporal regions of the female face [8,20].
Bone
Zygoma repositioning in FFS is not universally indicated or performed. When indicated, a commonly utilized method is a reduction malarplasty (Fig. 3, a), described by Kim and Seul [21]. Gingivobuccal incisions are made bilaterally to expose the body of the zygoma. A horizonal osteotomy at the zygomaxillary buttress is met with two parallel oblique vertical osteotomies at the anterior portion of the zygoma to form an L-shaped osteotomy and ostectomy. Next, greenstick fractures are formed at the zygomatic arches via posterior intraoral incisions. Together, this mobilizes of the zygomatic complex to a more medial position, reducing the width of the midface [21].
Bony facial feminization surgeries. (a) Reduction malarplasty: an L-shaped osteotomy is formed at the medial portion of the zygoma. Greenstick fractures are created at the zygomatic arches. The zygomatic section is placed in a more medial position. (b) Mandibular angle reduction: the mandibular angle is reduced via burring or osteotomies. (c) Sliding genioplasty: a T-shaped ostectomy narrows and shortens the chin. Recontouring the lateral aspect of the genioplasty via burring is necessary to avoid any bony step-off deformity.
Another method is a “sandwich” zygomatic osteotomy. A vertical osteotomy is created at the anterior portion of the zygomatic body. Next, an oblique horizontal osteotomy is formed at the junction of the zygomatic body and arch, proceeding anteriorly until it meets the superior end of the vertical osteotomy. Pivoting the zygoma creates greenstick fractures at the temporozygomatic suture and displaces the zygomatic body anteriorly, resulting in a new contour of the midface [22,23].
Soft tissue
Soft tissue augmentation of the midface may be accomplished with surgical as well as non-surgical methods. Among the surgical methods, malar implants may be placed typically via an intraoral route [17]. While implants have the advantage of immediate and long-lasting volume augmentation, malar implants also carry the risks of infection, extrusion, bone resorption, hematoma formation, or migration [18,24]. Alternatively, autologous fat grafting or fillers may also be performed [25,26]. Both fat grafting and fillers come with their common drawbacks, including inadequate correction, resorption, and need for multiple procedures over time.
MANDIBLE
Clinical evaluation
Masculine features of the mandible include prominence of the gonial angles [27] and a greater bigonial width [28]. In general, mandibular surgery in FFS entails reduction of the angle, body, and chin. However, one must carefully consider the patient’s ethnic background and preferences during surgical planning. For example, Western populations tend to prefer a more prominent and angled mandible compared with Asian populations [29]. In addition, orthognathic discrepancies should be carefully considered for correction of malocclusion prior to reduction of the mandible [30].
Bone
Mandibular angle reduction creates a more feminine jawline (Fig. 3, b). The angle and body of the mandibles are exposed via gingivobuccal incisions, and the soft tissue is separated in the subperiosteal plane while protecting the mental nerves. Adequate exposure of the entire body, ramus, and angle allows for precise contouring and prevents injury to the pterygo-masseteric muscles. Patients with prominent mandibular angles may require a combination of osteotomies and burring [30]. Mommaerts et al. [28] describe a mandibular feminization osteotomy technique utilizing an interdental midline osteotomy, two vertical box-shaped ostectomies at the anterior and lateral mandibular transition points, and triangular resections at the lateral mandibular borders to reduce gonial width.
Soft tissue
Repeated neurotoxin injection into the masseter muscles may soften a square-shaped jaw over time [15]. Another option involves resection of the anteromedial portion of the masseter muscle for further width reduction [8,31]. However, the masseter often atrophies over time with mandibular angle reduction; thus, direct masseteric manipulation should be done carefully and after accounting for atrophic changes, though many do still inject neurotoxin to accentuate the muscle wasting [8,13].
CHIN
Clinical evaluation
The male chin is broad, tall, and wide with greater projection than the female chin, which is narrow, pointed, and often short and tapered [6,28,32]. On average, the male chin is 17% taller than that of the female chin, with more lateral fullness [33]. Similar to assessments of the mandible, standard cephalometric relationships should be assessed at the bony level either using a lateral cephalogram or computed tomography scan. Discrepancies in the anterior/posterior or lateral dimensions should be simultaneously addressed with the feminizing procedure.
Bone
Reduction of the chin may be performed either with osteotomies or recontouring. A sliding genioplasty has often been described to feminize the chin (Fig. 3, c). This procedure, if performed in conjunction with mandibular angle reduction, is sometimes referred to as a V-line procedure [34]. The typical reduction genioplasty osteotomy is a horizontal osteotomy with a central wedge resection resulting in both a reduction of the width and height of the chin [32]. In addition to reduction of the chin, the anterior/posterior positioning of the chin is determined by standard cephalometric measurements.
However, some surgeons consider a sliding genioplasty to be unnecessary and prefer progressive reductions of the chin. Benefits include smooth contouring without the need for rigid fixation [13]. Another technique used is an interdental box-shaped impaction chin osteotomy technique by Mommaerts et al. [28] using a midline triangular ostectomy with a caudal base to reduce anterior chin width.
Surgical planning must consider that excessive reduction genioplasties can cause an imbalance between the soft tissue and underlying bone, in addition to loss of mentalis muscle. This may lead to a witch’s chin deformity, which is characterized by ptosis of the premental soft tissue and a prominent submental crease [35].
Soft tissue
After extensive mandibular reduction and genioplasty, excess tissue laxity may occur and induce jowling, even in the youthful patient. A face and/or neck lift corrects the jowling but can lead to unpredictable results if performed during surgical manipulation of the mandible or chin. Thus, a staged approach, where a face and/or neck lift is considered 6 to 12 months post-operatively has been recommended [36].
LARYNGEAL PROMINENCE
Clinical evaluation
The laryngeal prominence, colloquially known as the Adam’s Apple, is formed by the fusion of the anterior borders of two sections of thyroid cartilage that diverge at an angle of approximately 90° in men versus 120° in women resulting in a more projected appearance in male faces [37].
Surgical technique
A chondrolaryngoplasty can be approached in several ways to reduce the size of the laryngeal prominence. In the direct open approach, a transverse incision is made over the cartilage to access the notch. The strap muscles are separated, and the perichondrium is dissected to reveal the prominence. The cartilage is reduced with burring, or direct excision [8,27]. In the indirect approach, an intraoral [38] or submental [39] incision is created to access the thyroid cartilage. This method involves a more difficult dissection and relies on a less direct visualization of the cartilage but does conceal the scar. In addition, it avoids the potential of scar tissue adhering to the underlying cartilage, which can cause tethering when the patient speaks or swallows [27].
Chondrolaryngoplasties risk destabilization of the epiglottis and damage to the vocal cords [8]. Thus, direct visualization either via an open approach or endoscopy have been advocated to maximize the amount of cartilage that can be removed safely [40].
POSTOPERATIVE OUTCOMES
While the effects of FFS on patient psychosocial function and QoL is an active area of research, there is still much to be elucidated [1]. Utilizing a validated QoL survey (SF-36v2), Ainsworth and Spiegel [1] found that transwomen without gender reassignment surgery or FFS had lower physical-, social-, and mental health-related QoL compared with the general female population, while the mental health QoL of transwomen after gender reassignment surgery, FFS, or both, was similar to the general population. These findings have since been corroborated by two follow-up studies [41,42].
Recent reports have attempted to address the lack of data in the literature by focusing on patient satisfaction and QoL following FFS [41,43]. However, most have not used standard and validated approaches specific to FFS [6,44]. In a review of instruments that have been used to assess outcomes after gender-affirming surgery, 110 different tools were found, but only two were validated specifically for gender dysphoria [45]. Unsurprisingly, these inconsistencies and the overall lack of standardization in measuring health outcomes after FFS have made it difficult to compare results across studies.
An alternative measure to QoL is patient satisfaction [6,28,42,46]. A recent study evaluated the relationship between QoL and satisfaction in patients who received gender-affirming surgery, including facial surgery. Postoperative satisfaction, seen in nearly all patients, correlated reasonably well with QoL measures [47]. However, prospective, validated studies are necessary and are currently in progress among multiple multi-disciplinary teams in the world. The development of tools such as the GENDER-Q underline the ongoing effort to create a validated measurement of outcomes in patients receiving gender-affirming treatments [48].
According to the World Professional Association for Transgender Heath Standards of Care, Version 7 (SOC 7) published in 2012, gender-affirming chest reconstruction, known as “top surgery,” is considered a medical necessity, while FFS is not explicitly classified with cases determined on an individual basis [49]. These recommendations are likely secondary to the dearth of information surrounding FFS at the time of the publication of SOC 7. Given the recent increase of evidence in the literature, there is a consensus forming that FFS should be considered among the medically-necessary gender confirming surgeries in the WPATH SOC 8, which is currently under development [50].
CONCLUSION
FFS plays a crucial role in the gender transitioning process. Facial feminization can result in drastic improvements in congruence with one’s gender identity. In addition, surgeons performing FFS should not only understand the wide variety of techniques in the literature, but also the greater context of gender-affirming surgery with gender identity and expression. As FFS becomes more widely practiced, standardized outcomes data are necessary to develop evidence-based practices and optimize patient care.
Notes
Conflict of interest
No potential conflict of interest relevant to this article was reported.
Author contribution
Conceptualization: BN Dang, Justine C. Lee. Funding acquisition: Justine C. Lee. Methodology: BN Dang, Justine C. Lee. Writing - original draft: BN Dang, AC Hu, AA Bertrand, CH Chan, NS Jain, MJ Pfaff, James C. Lee, Justine C. Lee. Writing - review & editing: BN Dang, AC Hu, AA Bertrand, CH Chan, NS Jain, MJ Pfaff, James C. Lee, Justine C. Lee.