Immediate Direct-To-Implant Breast Reconstruction Using Anatomical Implants
Article information
Abstract
Background
In 2012, a new anatomic breast implant of form-stable silicone gel was introduced onto the Korean market. The intended use of this implant is in the area of aesthetic breast surgery, and many reports are promising. Thus far, however, there have been no reports on the use of this implant for breast reconstruction in Korea. We used this breast implant in breast reconstruction surgery and report our early experience.
Methods
From November 2012 to April 2013, the Natrelle Style 410 form-stable anatomically shaped cohesive silicone gel-filled breast implant was used in 31 breasts of 30 patients for implant breast reconstruction with an acellular dermal matrix. Patients were treated with skin-sparing mastectomies followed by immediate breast reconstruction.
Results
The mean breast resection volume was 240 mL (range, 83-540 mL). The mean size of the breast implants was 217 mL (range, 125-395 mL). Breast shape outcomes were considered acceptable. Infection and skin thinning occurred in one patient each, and hematoma and seroma did not occur. Three cases of wound dehiscence occurred, one requiring surgical intervention, while the others healed with conservative treatment in one month. Rippling did not occur. So far, complications such as capsular contracture and malrotation of breast implant have not yet arisen.
Conclusions
By using anatomic breast implants in breast reconstruction, we achieved satisfactory results with aesthetics better than those obtained with round breast implants. Therefore, we concluded that the anatomical implant is suitable for breast reconstruction.
INTRODUCTION
Breast ptosis is a common condition of increasing age. Breastfeeding and hormonal changes in women in their forties going through menopause cause changes in body weight and result in this undesirable condition [1]. In Korea, women in their forties and fifties are most susceptible to breast cancer [2]. Therefore, the breast shape is more ptotic in breast cancer patients, and plastic surgeons often need to reconstruct a more ptotic breast. In an aesthetic breast, the effect of gravity turns the breast mound slightly downward, and the point projecting most is the nipple-areola complex, which from the clavicle to this point should be a smooth straight line. However, in a ptotic breast, this line is concave [3].
In the post-cancer reconstruction of a breast that had a ptotic shape, the use of a round cohesive gel breast implant, currently being used, leads to convexity and an unnatural ptotic shape compared to the shape of the other breast [4,5]. These disadvantages are particularly severe for patients who are thin and have a high inframammary fold and a ptotic breast. To overcome this problem, a shaped breast implant has been developed (Biocell Natrelle 410 Silicone-Filled Breast Implant). This implant is anatomically shaped as a tear drop with less projection in the upper pole and greater projection in the lower pole [6,7]. Thus, it tends to give an appearance of less upper fullness and increased lower pole projection as compared to what would be produced by a round implant. Further, it consists of a highly cohesive form-stable silicone gel. This cohesiveness maintains the implant shape and reduces rippling [8]. The variety of heights (low, moderate, and full) and projections (low, moderate, full, and extra full) offers surgeons more choices. The result of this customization is a natural ptotic breast shape. The authors used this shaped breast implant in patients who underwent sparing mastectomies due to breast cancer and discuss their experience here.
METHODS
Study patients
The current study was conducted in 30 patients (31 breasts) who were diagnosed with breast cancer without radiation therapy at our medical institution during the period from November 2012 to April 2013. The patients' mean age was 44.2 years (range, 32-57 years). Seven patients were diagnosed as stage 0 of breast cancer, 14 as stage I, nine as stage II, and one as stage III. No patients needed radiation therapy, but 11 patients received chemotherapy. The mean follow-up time was 11 months (range, 8-13 months). They underwent skin-sparing mastectomy (SSM), nipple-sparing mastectomy (NSM), or areola-sparing mastectomy. All patients immediately received single-stage breast reconstruction with anatomically shaped implants (Biocell Natrelle 410 Silicone-Filled Breast Implant, Allergan, Irvine, CA, USA) and an acellular dermal matrix (ADM).
Surgical technique
Before surgery, we took a patient history and performed a physical examination, including gathering information on chest wall measurement, chest asymmetry, body-mass index, breast feeding, and menstruation cycle. With the patients sitting upright, the suprasternal notch and xiphosternum were marked on the chest wall. Breast landmarks such as the nipple-areola complex, medial and lateral end of the inframammary crease, and base of the breast were checked to determine the degree of breast symmetry. Next, the inframammary folds and midline were marked using gentian violet. The patients underwent SSM or NSM performed by a general surgeon. The specimen volume was measured following mastectomy. While considering the volume of the specimen, breast shape, and breast symmetry of the opposite side, the surgeon selected the breast implant sizer and inserted it in the pocket through the incision. It was confirmed in the sitting position. The dissection range was designed with the selected implant sizer using gentian violet thus defining the pocket size. The pocket was precisely dissected along the marked pocket size to prevent complications such as malrotation. The lateral border of the pectoralis major muscle was elevated from the chest wall, along its inferior border. The elevated pectoralis muscle was detached from the sternal origin. A pocket was developed beneath, appropriate for inserting the breast implant. The anterior border of the serratus anterior muscle was dissected to provide adequate space for implant insertion. Irrigation with an antibiotic solution was done in the submuscular and subcutaneous pocket. The implant was inserted within the submuscular pocket. ADM was sewn to release the inferior and lateral margin of the pectoralis major. This suture line continued for the length of the ADM following the curving lateral contour of the pectoralis major. The inferior edges of the ADM were then sutured to the chest wall at the inframammary fold. The lateral extent of this suture line mimicked the lower pole contour of the future breast and was sutured onto the serratus anterior fascia. Two suction drains were inserted in both the submuscular and the supramuscular planes. These drains usually remain for 1 or 2 weeks and are removed when less than 20 mL of fluid collects for two consecutive days.
Assessment
Outcomes were assessed by an evaluation of postoperative photographs of patients' breasts at least six months postoperatively by the authors and patients. Results were evaluated on the basis of breast volume and shape compared with the contralateral breast, breast symmetry, and the overall results. Both the authors and the patients scored their impression on a linear numerical analog scale from 1 to 4. For the data analysis, the score of 1 corresponded to a poor result, 2 to a moderate result, 3 to good, and 4 to excellent results. Function was confirmed by the degree of discomfort while wearing a brassiere, and possible complications were checked. Any instances of infection, hematoma, seroma, skin thinning, wound dehiscence, rippling, malrotation, capsular contracture, and removal of implant were evaluated.
RESULTS
The mean resection volume of oncologic surgery was 240 mL (range, 83-540 mL). The mean size of the implant using breast reconstruction was 217 mL (range, 125-395 mL). NSM was conducted in 16 cases, areola-sparing mastectomy in 2 cases, and SSM in 13 cases. The incisions included transverse incisions used in 20 patients, lateral extension in 10, and vertical in 1 patient.
Most of the subjects were implanted with a moderate-height implant. It was placed in a submuscular position superiorly and in an ADM pocket inferiorly (Table 1). All the ADMs were CG cryoderm (CGBio Corp., Seongnam, Korea) or AlloDerm (LifeCell Corp., Branchburg, NJ, USA).
The aesthetic result was considered good or excellent by the surgeons and patients in more than 85% of the cases. The postoperative results are shown in Figs. 1, 2. The lateral view of anatomical implants showed that upper-pole fullness was decreased and lower-pole projection was adequate in comparison with those of round implants (Fig. 3). There was a close correlation between surgeon and patient assessment. One month after surgery, the patients were wearing a wireless brassiere, usually a sports bra. In most cases, there was no discomfort wearing a bra and in daily life. Some of the inconvenience was caused by the hardness of the breast, which was due to the breast implant itself. Infection appeared in one patient who developed erythema and tenderness around the incision area. After chemotherapy, leukopenia can occur as an opportunistic infection. She recovered after admission and intravenous antibiotics for seven days. Hematoma and seroma did not occur. Skin thinning occurred in one case. The skin of the lower pole was thinning, possibly leading to perforation. However, there were no hematomas or seromas under ultrasonography. We observed the progress of skin thinning at short term follow-up; fortunately, the skin recovered without further problems. Three cases of wound dehiscence occurred; one required surgical intervention, and the others healed with conservative treatment in one month. There were no complications such as rippling, malrotation, capsular contracture, or removal of the implant (Table 2).
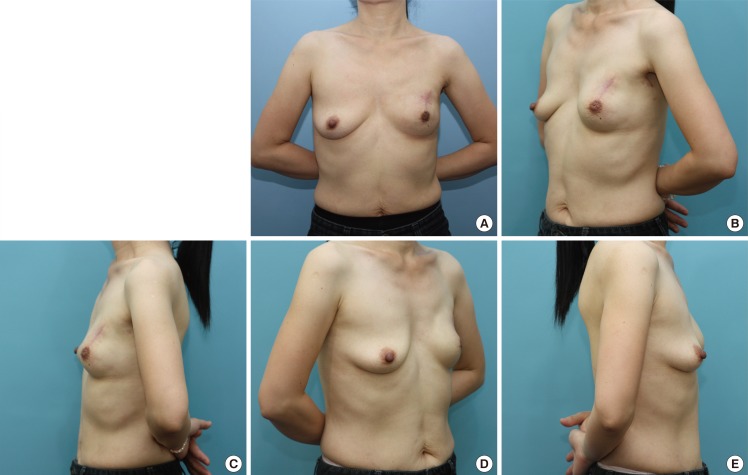
Postoperative results
(A-E) Six-month postoperative view of left breast reconstruction immediately after areola-sparing mastectomy with a Natrelle 410 style full height and moderate projection 155-mL implant.
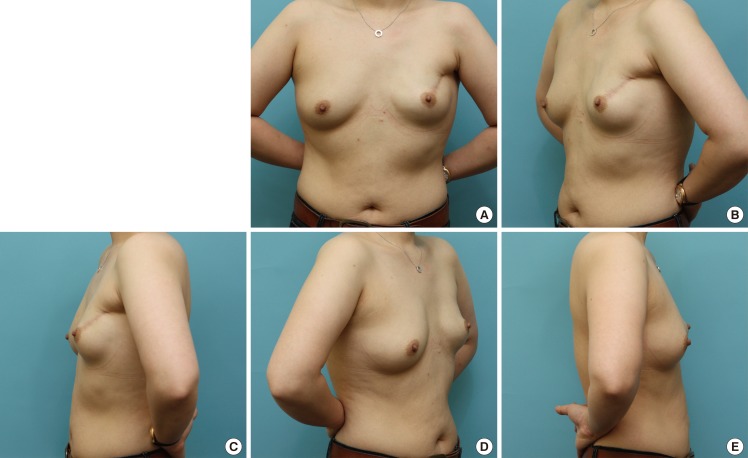
Postoperative results
(A-E) Six-month postoperative view of left breast reconstruction immediately after nipple-sparing mastectomy with a Natrelle 410 style moderate height and moderate projection 215-mL implant.

Comparison of postoperative round and anatomical implant
The six-month postoperative results of breast reconstruction using anatomical breast implant and round implant. Breast reconstruction with anatomical breast implant (A), (B) led to less fullness in the upper pole but an appropriative projection in the lower pole as compared to a round breast implant (C), (D). The anatomical breast implant formed a natural breast shape.
DISCUSSION
Breast implants are continuously improving, and currently, fifth-generation breast implants are in use [9]. While anatomical breast implants were used earlier, a high risk of capsular contracture reduced their use, 20 years after the trial of the round breast implant that was dominant in the market. In 2012, a form-stable silicone gel breast implant was introduced and an anatomical breast implant is being used again. In Korea, the anatomically shaped breast implant has been used formally since July 2012. In February 2013, the US Food and Drug Administration approved it, and its stability has been confirmed [10]. Anatomic implants consist of a form-stable silicone gel and a thick, strong low-bleed shell leading to variable height-to-width ratio implants. Along with variations in the height and width, it made possible the enhancement of projection [11,12]. With the capability of production of a variety of breast implants, implant choice has expanded for patients whose breast shape is asymmetric. This has led to the widespread popularity of the anatomically shaped breast implants in aesthetic surgery. The new breast implant, unlike the round breast implant, gives a more natural breast shape after surgery; upper-pole fullness is decreased and lower-pole projection is adequate in the lateral view. The firm cohesive gel maintains a tear-drop shape, which does not result in folding and leads to less rippling [13]. It is suitable for use in reconstruction after SSM or NSM for breast cancer patients who had a ptotic breast, giving them an aesthetically pleasing appearance. There are some disadvantages. The patients reported being uncomfortable with the hardness of the reconstructed breast. When patients changed position to a recumbent or supine position, anatomical breast implants retained their shape, resulting in an unnatural breast shape [14,15]. Some patients, however, felt their breast to be soft despite the implant. Patients with textured breast implants containing a cohesive silicone gel did not develop severe capsular contracture. The cohesive silicone gel and the cross-linking state withstood the surrounding contracture forces that result in a new capsule. As a result, the anatomical implant was harder but had less capsule formation, resulting in better comfort [13,16]. Malrotation of anatomical breast implants is reported to be in the range of 1.1% to 14% [14,17]. Because the implant can rotate in the pocket, the surgeon was careful during implant selection and to avoid suboptimal techniques of pocket dissection and suboptimal pocket dimensions [14,18]. Anatomical implants offer a variety of profiles, and surgeons can select their width, projection, and height. Surgeons try to please patients by allowing them to choose from among the different types of breast implants, but the correct choice can be challenging. In the current study, the length of the incision was in the range of 6 to 10 cm, and this provided a sufficient operation field. The authors inserted the breast implant sizer in the subcutaneous plane and marked the range of the dissection area with gentian violet. As a result, the authors performed pocket dissection according to the breast implant size and inserted it exactly. None of our patients experienced any significant malrotation or capsular contracture. In general, capsular contracture occurs less often than with a round implant, in the range of 4.6% to 9% [14]. Because we did not have enough follow-up time to assess whether these complications occurred, we need to continue follow-up. Infection occurred in one patient and was resolved conservatively. Unlike infection, red breast syndrome, which is erythema occurring on the lower pole, did occur in several cases. Red breast syndrome appears similar to infection or cellulitis without systemic signs of infection, such as fever and leukocytosis, and without any radiographic evidence of seroma or abscess [19]. Such patients were treated with intravenous antibiotics and fluid. However, this symptom was refractory to treatment and was self-limiting. It appeared on the skin flap of the lower pole overlying the ADM. The cause of this symptom was not the anatomical implants but the ADM. The preservatives in which the ADM was soaked cause an inflammatory-like response. For this reason, it is recommended that the ADM be washed in saline baths to eliminate the preservatives [19]. We obtained acceptable results from breast reconstruction by using the anatomical breast implant. The natural ptotic breast shape was well maintained due to the form-stable silicone gel. In addition to the aesthetics, the anatomical breast implant produced excellent functional outcomes of breast reconstruction as compared to a round breast implant. However, all materials have benefits and drawbacks. This study provided us with a better understanding of a new type of breast implant, enabling safe and appropriate clinical application.
Notes
This article was presented at the 31st International Conference of the Korean Society for Aesthetic Plastic Surgery on April 27-28, 2013 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.


