Distally Based Sural Artery Adipofascial Flap based on a Single Sural Nerve Branch: Anatomy and Clinical Applications
Article information
Abstract
Background
The distally based sural artery flap is a reliable, local reconstructive option for small soft tissue defects of the distal third of the leg. The purpose of this study is to describe an adipofascial flap based on a single sural nerve branch without sacrificing the entire sural nerve, thereby preserving sensibility of the lateral foot.
Methods
The posterior aspect of the lower limb was dissected in 15 cadaveric limbs. Four patients with soft tissue defects over the tendo-achilles and ankle underwent reconstruction using the adipofascial flap, which incorporated the distal peroneal perforator, short saphenous vein, and a single branch of the sural nerve.
Results
From the anatomical study, the distal peroneal perforator was situated at an average of 6.2 cm (2.5-12 cm) from the distal tip of the lateral malleolus. The medial and lateral sural nerve branches ran subfascially and pierced the muscle fascia 16 cm (14-19 cm) proximal to the lateral malleolus to enter the subcutaneous plane. They merged 1-2 cm distal to the subcutaneous entry point to form the common sural nerve at a mean distance of 14.5 cm (11.5-18 cm) proximal to the lateral malleolus. This merging point determined the pivot point of the flap. In the clinical cases, all patients reported near complete recovery of sensation over the lateral foot six months after surgery. All donor sites healed well with a full range of motion over the foot and ankle.
Conclusions
The distally based sural artery adipofascial flap allowed for minimal sensory loss, a good range of motion, an aesthetically acceptable outcome and can be performed by a single surgeon in under 2 hours.
INTRODUCTION
The distally based sural artery flap is a reliable, local reconstructive option for small soft tissue defects of the distal third of the leg. In 1992, Masquelet [1] introduced the neurocutaneous island flap that included superficial nerves thereby improving its reliability. He described the vascularity of the flap to be enhanced by a dense arterial plexus between the vasa nervorum and branches of the septocutaneous perforators of the leg. Nakajima [2,3] subsequently expanded on the vascular anatomy of this area. He demonstrated the presence of an intricate vascular network surrounding the sural nerve and the short saphenous vein and outlined extensive connections between the fascia and dermis that supplied the skin. He coined the term 'venoneuroadipofascial pedicled fasciocutaneous flap'.
From our experience, the distally based sural artery flap may also be raised as an adipofascial flap by including the vein and nerve, but leaving the skin intact. This technique reduces donor morbidity and improves the reach when it is used as a turnover flap. Key to sufficient vascularity of the flap is the inclusion of the sural nerve, but this leads to sensory loss over the lateral aspect of the foot. The purpose of this study is to describe an adipofascial flap based on a single sural nerve branch (medial or lateral) without completely sacrificing sural nerve continuity and thereby preserving lateral foot skin sensation.
METHODS
Anatomical study
We dissected the posterior aspect of 15 cadaveric limbs. The course of the sural nerve, the short saphenous vein and the perforating branches in the adipofascial layer were identified to define the vascular anatomy of the distally based sural artery flap.
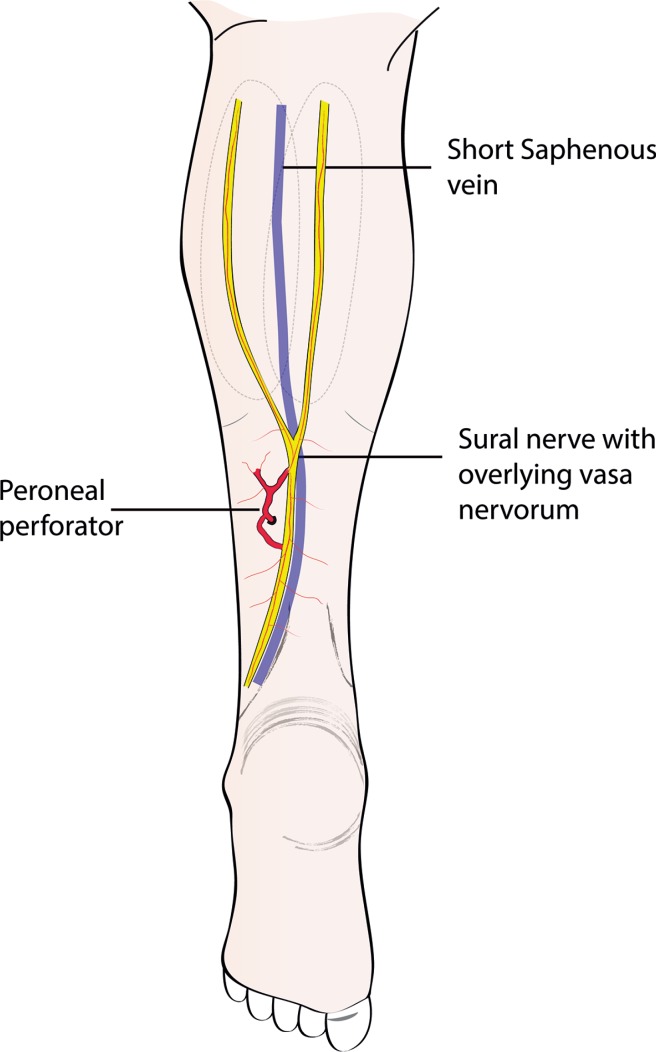
The primary blood supply of the adipofascial layer was derived from septal perforators. These originated from the peroneal artery (13 specimens) and the posterior tibial artery (2 specimens). Distally, they course between the soleus and peroneus longus, with the distal-most peroneal perforator situated at an average of 6.2 cm (2.5-12 cm) above the distal tip of the lateral malleolus (Table 1). The peroneal perforators formed a vascular network with the perforators of the posterior tibial artery, and contribute to the vasa vasorum of the saphenous vein and the vasa nervorum of the sural nerve (Fig. 1).

Distances between the distal tip of the lateral malleolus and distal peroneal perforator, and the convergence point of the medial and lateral sural nerve branches, and the level of fascia penetration

Posterior aspect of the right lower limb
Dissected specimen showing a peroneal perforator (arrow) giving rise to the vasa nervorum with branches extending to the skin (reflected).
The common sural nerve was formed by the confluence of the medial and lateral sural nerve branches in all specimens (Fig. 2). The medial sural nerve originated from the tibial nerve in the inferior triangle of the popliteal fossa. It coursed alongside the tibial nerve while passing between the two heads of the gastrocnemius muscle. Between the bellies of the gastrocnemius, it coursed subfascially in the musculoaponeurotic channel. The lateral sural nerve originated from the common peroneal nerve and ran across the lateral gastrocnemius belly in the subfascial plane. As both nerves travelled distally, they entered the subcutaneous plane by piercing the muscle fascia 16 cm (14-19 cm) proximal to the lateral malleolus. They merged 1-2 cm distal to the subcutaneous entry point to form the common sural nerve at a mean distance of 14.5 cm (11.5-18 cm) proximal to the lateral mallelolus (Table 1).
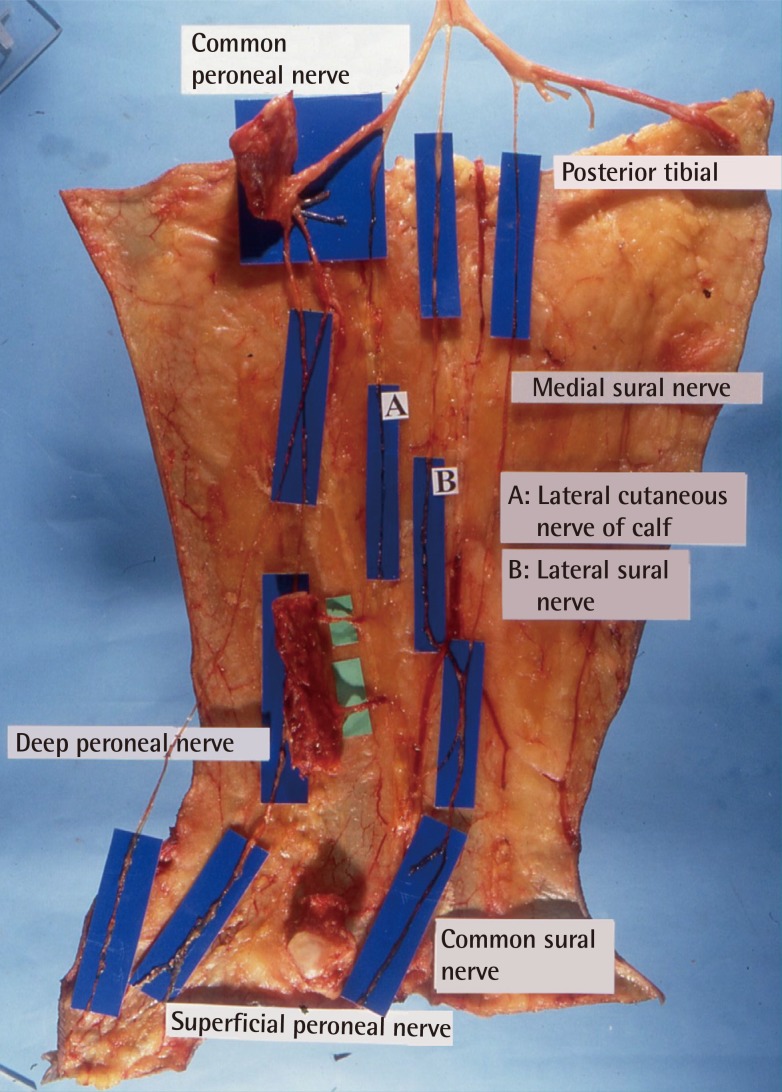
Sural nerve anatomy of the right lower leg
Dissected specimen showing the medial sural nerve branch originating from the posterior tibial nerve, and the lateral sural nerve originating from the common peroneal nerve, converging to form the common sural nerve 14.5 cm from the distal tip of the lateral malleolus.
The common sural nerve and the short saphenous vein were located in the subcutaneous plane adjacent to one another in the lower third of the leg. The short saphenous vein ran in the subcutaneous plane following the posterior midline of the leg and pierced the muscle fascia in the upper third of the leg to join with the popliteal vein (Fig. 3). We designed a broad flap to capture one of the sural nerve branches and the short saphenous vein.
Surgical technique
Four patients with soft tissue defects over the tendo-achilles and ankle underwent reconstruction using the distally based sural artery adipofascial flap (Table 2). The flap design incorporated the distal peroneal perforator, short saphenous vein, and a single branch of the sural nerve. Markings of the flap dimensions and lower limb midline were made and at least two distal perforators of the peroneal artery were identified using a hand-held Doppler. The approximate path of the sural nerve was also marked out (Fig. 4). We harvested the flap via a lazy-S incision over the posterior calf and raised the skin flaps to expose the adipofascial layer. A broad adipofascial flap was elevated distal to proximal and this included the deep fascia overlying the gastrocnemius muscle. The short saphenous vein was harvested with a 5 cm stump to allow intermittent blood letting of the flap during the first 48 hours after operation. A broad flap was necessary to capture both a branch of the sural nerve and the short saphenous vein, which are parallel structures spaced 1-2 cm apart (Fig. 3). The flap was based on a single branch of the sural nerve with its accompanying vasa nervorum, the short saphenous vein with its accompanying vasa vasorum and the most distal perforator branch of the peroneal artery [2,3]

Flap design for harvest of adipofascial flap
Axis of the flap (x). The path of the medial sural nerve is marked (←) and the nerve is spared.
We aimed to harvest a single branch of the sural nerve. For this reason, the pivot point of the flap was determined by the point of convergence of both branches of the sural nerve. In our study, this was approximately 14.5 cm from the distal tip of the lateral malleolus, meaning that our technique would also capture peroneal perforators supplying the adipofascial flap (Table 1). The lateral branch of the sural nerve was included in three of our cases while the medial branch in one case. The adipofascial flap was turned down to cover the defect and in turn covered with split thickness skin grafts from the medial thigh after two weeks. The flap donor sites were closed primarily. In the first two weeks after surgery, the patients were nursed in prone position. They were initially allowed mobilization on a wheelchair, followed by ambulation with the support of crutches. They were all fully weight bearing by four weeks. All patients underwent follow-up care at one, three, and six months postoperatively.
RESULTS
All four patients reported a near complete recovery of sensation over the lateral foot, six months after surgery. Recovery of sensation was defined as two-point discrimination <20 mm to pinprick and comparative soft touch [4]. At one month after surgery, all patients reported a healed donor site with a full range of motion over the foot and ankle. They were satisfied with the aesthetic appearance of both the flap and the donor site at the posterior calf. There were no complications such as flap necrosis or wound breakdown. The patients did not have problems with weight bearing or footwear fit.
Clinical cases
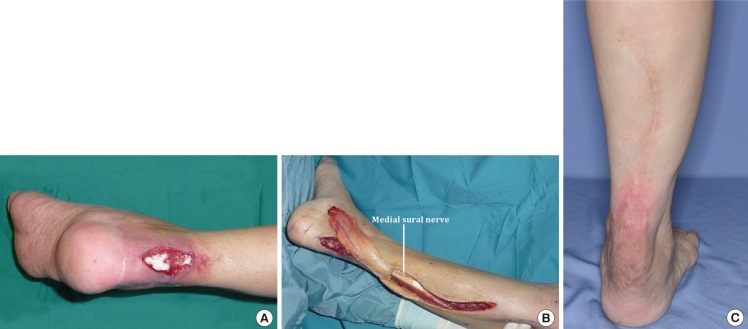
Case 1
A 22-year-old man sustained acute trauma to his left lower leg with a degloving injury over the lateral malleolus, exposing the fibula bone. The 3 cm×2 cm defect was covered with a 15 cm×4 cm adipofascial flap that included the medial sural nerve (Fig. 5).

A case of acute traumatic degloving injury
(A) A 3 cm×2 cm lateral malleolar defect exposing the fibula, covered with a turn down adipofascial flap. The distal defects were resurfaced with split skin grafts. (B) A 15 cm×4 cm adipofascial flap based on a distal peroneal perforator, harvested with the short saphenous vein and medial sural nerve branch. The lateral sural nerve was preserved. (C) Postoperative appearance at 6 months.
Case 2
A 54-year-old woman sustained acute trauma to her right lower leg with skin breakdown over the tendo-achilles region after tendon repair. The 5 cm×2 cm defect was covered with a 15 cm×4 cm adipofascial flap, which included the lateral sural nerve (Fig. 6). The patient described good sensory recovery over the lateral foot and a good aesthetic outcome one year after the procedure.
A case of tendo-achilles wound breakdown
(A) Skin breakdown after tendo-achilles repair with resultant 5 cm×2 cm defect. (B) A 15 cm×4 cm adipofascial flap including the lateral sural nerve was elevated and turned down to cover the defect. The medial sural nerve was preserved. (C) Appearance of adipofascial flap 1 year postoperatively.
Case 3
A 66-year-old man had wound dehiscence over the left tendo-achilles region after tendon repair. The 3 cm×2 cm defect was covered with a 10 cm×4 cm adipofascial flap that contained the lateral sural nerve (Fig. 7).
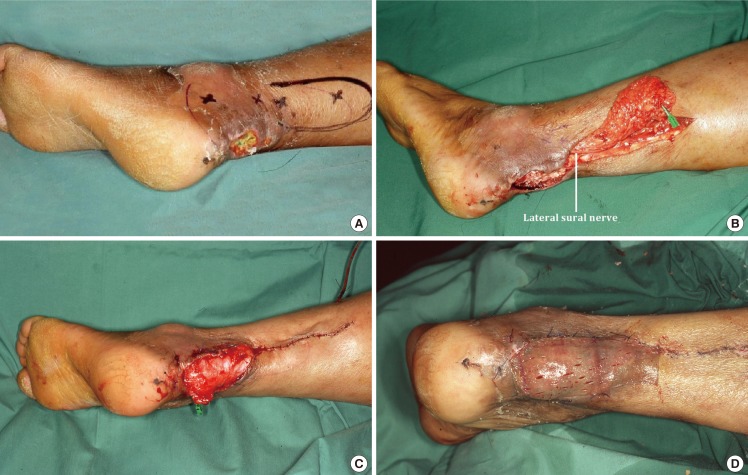
A case of tendo-achilles wound breakdown
(A) Skin breakdown after tendo-achilles repair with resultant 3×2 cm defect. (B) A 10×4 cm adipofascial flap including the lateral sural nerve was elevated and turned down to cover the defect. (C) Immediately after adipofascial flap inset. Short saphenous vein stump held with green vessel clip. (D) Skin grafting over adipofascial flap 2 weeks after turndown.
DISCUSSION
The distally based sural artery adipofascial flap is supplied by distal peroneal perforators which contribute branches to the overlying skin via the vasa nervorum and vasorum of the sural nerve branch and short saphenous vein respectively. Inclusion of the sural nerve and short saphenous vein gives a robust axial blood supply to the flap [5,6]. In our study, we found that the distal-most perforator was located 2.5 cm to 12 cm proximal to the distal tip of the lateral malleolus. This variability is consistent with the findings of other authors [7,8] who maintain that the pivot point should be a minimum of 5 cm proximal to the lateral malleolus for consistent flap survival. Additionally, our study showed that the peroneal perforators form an intricate network with 1) the perforators of the posterior tibial artery, 2) the vasa of the short saphenous vein and 3) the vasa of the sural nerve. This finding is consistent with Nakajima's study [3]. Thus, the inclusion of the sural nerve and short saphenous vein improved vascularity and permitted the harvest of a longer flap.
The distally based sural artery flap has two venous drainage systems: the short saphenous vein and the vena comitantes of the peroneal perforator. The blood flow in the short saphenous vein is in reverse fashion while that in the vena comitantes is anterograde. Unlike traditional distally based sural artery flaps, adipofascial flaps manifest venous congestion atypically as they are devoid of skin. We routinely lance the capillaries on the fascia to evaluate the colour of bleeding. The flap is deemed congested when dark blood is seen. As a safety measure, we included an extra 5 cm of the short saphenous vein beyond the flap for blood letting in the first 48 hours postoperatively. This manoeuvre relieved venous congestion and promoted flap circulation, while a more efficient venous drainage was being established gradually [9].
The most common pattern of the sural nerve and its branches consists of the medial and lateral sural nerves merging to form the common sural nerve in 73% of individuals [10], This anatomical pattern was found in all our cadaveric specimens (Figs. 2, 3).
Sensory loss occurs over the lateral foot after sural nerve harvest and our technique of preserving sensibility depends on the anatomical pattern described above. The level at which the medial and lateral sural nerves converge to form the common sural nerve has been reported variously as 8.5 and 18.3 cm above the lateral malleolus [5,10]. We report a mean of 14.5 cm (range, 11.5-18 cm) in this study. We based the pivot at the point of convergence and this enabled the inclusion of either the medial or lateral branch, without complete sacrifice of the sural nerve axis.
The turndown flap design was used to maximize the reach of the flap, minimize flap lost in transit and prevent kinking of the perforator. In harvesting the adipofascial flap with a single sural nerve branch, our patients reported near complete sensory recovery over the lateral foot on 2-point discrimination and comparative soft touch. Additionally, we believe this reduced the risk of neuropathic dermatitis associated with skin denervation [11].
Donor morbidity was minimal, with very good functional and aesthetic outcomes. Compared to fasciocutaneous flaps, adipofascial flaps are less bulky, result in less donor site morbidity and lead to a better aesthetic outcome [12]. Adipofascial flaps leave donor site skin intact while fasciocutaneous flaps cause narrowing of the calf. Skin grafts were laid onto the adipofascial flap two weeks postoperatively. The adequate vascularity of the adipofascial flap ensured that the skin grafts survived and remained stable. There was no skin breakdown or abrasions and the patients were prescribed emollients for daily application. Adipofascial flaps, by virtue of their thinness, re-establish foot contour and allow for normal footwear.
In our study, the flap resulted in minimal sensory loss and a good range of motion. Furthermore, the flap is simple to harvest, and can be performed by a single surgeon in under 2 hours. A comparative study supports these advantages and illustrates the adipofascial flap to be as safe as the fasciocutaneous flap [13].
The main limitations of this technique are that it is restricted to small defects which are proximal in location and there is greater flap loss in transit due to the higher pivot point.
Notes
This article was presented at the World Society for Reconstructive Microsurgery Congress on 2013 in Chicago, IL, USA.
No potential conflict of interest relevant to this article was reported.