A Ganglion Cyst of the Temporomandibular Joint
Article information
Ganglion cyst, although its precise etiology is not determined, is generally considered a degeneration of the mucoid connective tissue, collagen in specific, and was reported for the first time by Ledderhose in 1893 [1]. It is a benign soft-tissue tumor that usually appears near joints such as the hand, wrist, or foot. A ganglion cyst of the temporomandibular joint (TMJ) is a rare disease, and few cases of this condition have been reported in the English language literature. It may develop from a myxoid decay of the collagenous tissue of the TMJ capsule, without an epithelial or endothelial lining. Unconnected with the joint cavity, this cyst arises from the capsule of the joint. The cyst is filled with a gelatinous material and lined with a fibrous connective tissue wall without cells [2]. We present important aspects of the clinical findings, histologic features, and therapeutic options of a rare case of a ganglion cyst of TMJ with a review of the previous articles.
A 48-year-old man was admitted at the Department of Head and Neck Surgery at our hospital for an acute spinning type of dizziness lasting a week. An otolaryngologist's first impression was vestibular neuritis, and magnetic resonance imaging (MRI) was performed for further evaluation. The MRI revealed chronic otomastoiditis and a cystic mass in the left pre-auricular region (Fig. 1). The otolaryngologist prescribed medications for vestibular neuritis. Because the otolaryngologist and a radiologist regarded the patient's preauricular mass to be a simple subcutaneous benign mass, the patient was also referred to the Plastic and Reconstructive Department for mass removal. Preoperatively, the patient had no typical symptoms and signs such as malocclusion, trismus, a clicking sound, or TMJ tenderness except for the mild swelling at the preauricular area. Physical examination revealed a 1-cm round, slightly mobile mass in front of the right tragus. As the junior author regarded the mass to be a simple subcutaneous cyst such as a lipoma or an epidermal cyst, he performed a surgical excision of the tumor under local anesthesia. The surgeon injected local anesthetics (2% lidocaine with 1:80,000 epinephrine) very superficially into the subcutaneous layer. Then, he made a direct vertical small incision in front of the right tragus over the protruding mass and performed dissection with a pair of blunt Metzenbaum scissors. During dissection around the mass, he inadvertently found that the mass penetrated into the depth of the temporalis fascia, and he started to use a nerve stimulator. After retraction of the superficial temporal vessels anteriorly with the skin flap, with the aid of a nerve stimulator, the surgeon made an oblique incision parallel to the frontal branch of the facial nerve, through a superficial layer of the temporalis fascia above the zygomatic arch. Then, he inserted the periosteal elevator beneath the superficial layer of the temporalis fascia and stripped the periosteum off the lateral zygomatic arch. Dissection was carried out inferiorly to expose the capsule of the TMJ. Intraoperatively, a cystic mass sized 10 mm in diameter was found. Its surface was soft, round, and translucent. The cystic mass was filled with a jelly-like material and connected with the lateral surface of the TMJ capsule by a short, narrow stalk. The tumor was successfully extirpated without injury to the facial nerves (Fig. 2). Histopathologic examination confirmed a ganglion cyst (Fig. 3). There was no sign of recurrence 8 months postoperatively, and the patient's symptom of dizziness disappeared.
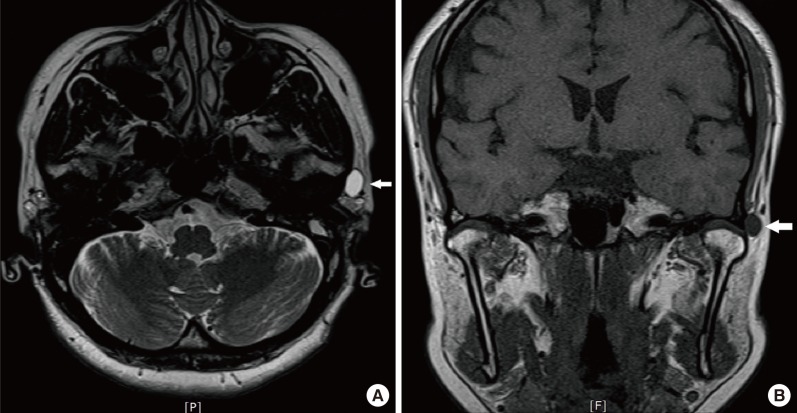
(A) Preoperative axial T2-weighted magnetic resonance image. (B) Coronal T1-weighted magnetic resonance image shows a cystic lesion (white arrows) lateral to the left condyle.

Intraoperative photograph showing the ganglion cyst in the lateral aspect of the temporomandibular joint capsule.
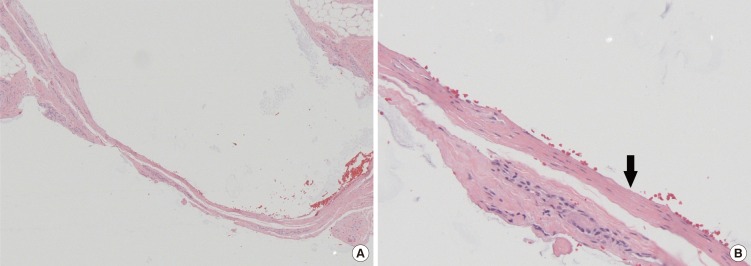
(A) Histopathologic photomicrographs show a cystic wall of fibroconnective tissue with H&E, ×40. (B) Cystic wall consisted of a myxoid degeneration of the collagenous tissue (black arrow), ×200.
The ganglion cyst of the TMJ is more frequently seen in middle-aged women than in men or women of other ages and usually presents as a parotid or preauricular mass because of its anatomical region [3]. Because a ganglion cyst in the TMJ is not common, an accurate preoperative diagnosis is not easily made. The differential diagnosis of the preauricular mass has extensive lists. A variety of conditions or diseases must be considered in the differential diagnosis of a ganglion cyst at the TMJ, such as parotid tumor, parotid cyst, retention cyst, sebaceous cyst, branchial cleft cyst, vascular tumor, and lymphangioma. Besides, rare TMJ lesions, such as synovial chondromatosis, osteochondroma, osteoma, pigmented villonodular synovitis, bone cyst, Langerhans cell histiocytosis, plasma cell myeloma, and sarcoma, must also be considered.
Among the most commonly used radiological modalities, that is, sonography, computed tomography, and MRI, MRI remains the best diagnostic imaging technique to determine TMJ pathology [2] as MRI usually reveals the location, size, and density of the lesion, as well as its connection with the surrounding structures [1].
Despite their distinct entities, ganglion cysts and synovial cysts are often mistakenly used alternatively in the literature. Although ganglion cysts and synovial cysts seem similar clinically, synovial cysts are true cysts filled with synovial fluid and lined with endothelial cells because they are produced by the movement and herniation of the synovial lining due to an increased pressure in the associated joint. On the other hand, ganglion cysts, which are not connected to the joint cavity, appear to be developed from a myxoid degeneration of the collagenous tissue of the joint capsule. They are not true cysts because they lack a cellular lining and are made of a gelatinous, viscous material and surrounded by fibrous connective tissue [2]. These two kinds of cysts can be clearly differentiated from each other only through histological examination.
The treatment options of the ganglion cyst vary from conservative treatment to surgical removal. The surgical excision of symptomatic ganglion cysts of the TMJ remains the mainstay of the treatment, with the most common complication being recurrence due to incomplete excision. Surgical excision has usually been performed by using a preauricular approach and is considered to be the procedure of choice. Although there is a case establishing facial nerve palsy and intracranial extension, patients with asymptomatic lesions may undergo some period of conservative management, because there are some cases of spontaneous regression [4].
We emphasize that if a patient has a mass adjacent to the TMJ and shows concomitant vague symptoms related to TMJ disorders such as headache, otalgia, TMJ sounds or crepitus, dizziness or vertigo, fullness of the ear, and tinnitus, surgeons must consider the possibility of a ganglion cyst of the TMJ [5]. We expect our rare case to be helpful to surgeons for making an early diagnosis and planning a treatment strategy for the ganglion cyst of the TMJ.
Notes
This article was presented at the 3rd Research and Reconstructive Forum on May 9.10, 2013, in Daegu, Korea.
No potential conflict of interest relevant to this article was reported.