A New Method for Forming the Pretarsal Fullness after Lower Blepharoplasty
Article information
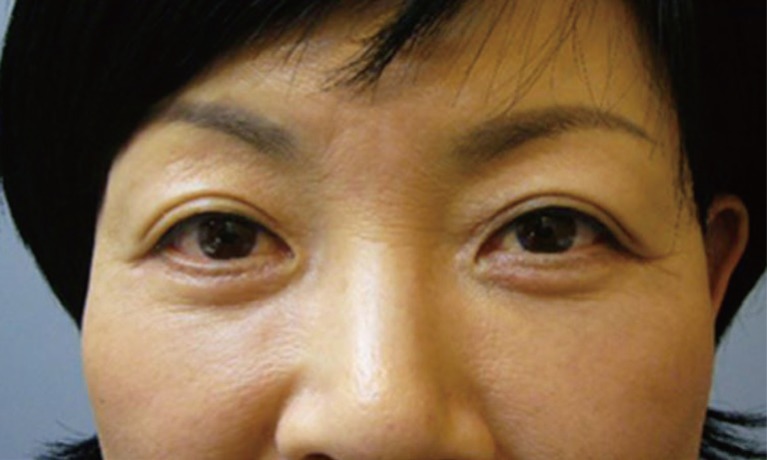
Patients with lower eyelid aging may frequently have a dull appearance with no facial expression rather than a younger, healthy and sweet one after the removal of the orbital fat bulging, resection of the redundant skin and orbicularis oculi muscle (OOM) (Fig. 1). This is because the pretarsal fullness disappears or becomes flattened or depressed after lower blepharoplasty. To resolve this, many local clinics perform various procedures for re-creating the pretarsal fullness after lower blepharoplasty. Still, however, there are only a limited number of reports about such surgical methods. Unlike a few methods that have been already published, however, our two-step fixation methods are simplified and effective in shortening the operation time and obtaining excellent cosmetic outcomes.
Preoperative marking was done below the lacrimal punctum at a length of 2 to 3 mm under the eyebrow in the lower palpebral region. Then, a line was drawn in parallel with the lower margin of the lower eyelid. Laterally, the surgical design was done for crow's feet within such a scope that is not remote from the lateral orbital rim. We made an incision from the lateral crow's feet to such a depth that the orbital septum could be seen as the underlying structure of the OOM in the visual field, thus creating a hole. A small mosquito was placed through this hole and then used to dissect between the OOM and the orbital septum along the medial side of the lower eyelid.
With the dissection of the region between the OOM and the orbital septum using a blunt scissor, they were isolated from each other using a bevel incision while meticulously preserving the pretarsal portion of the OOM at a length of approximately 4 to 5 mm (Fig. 2).
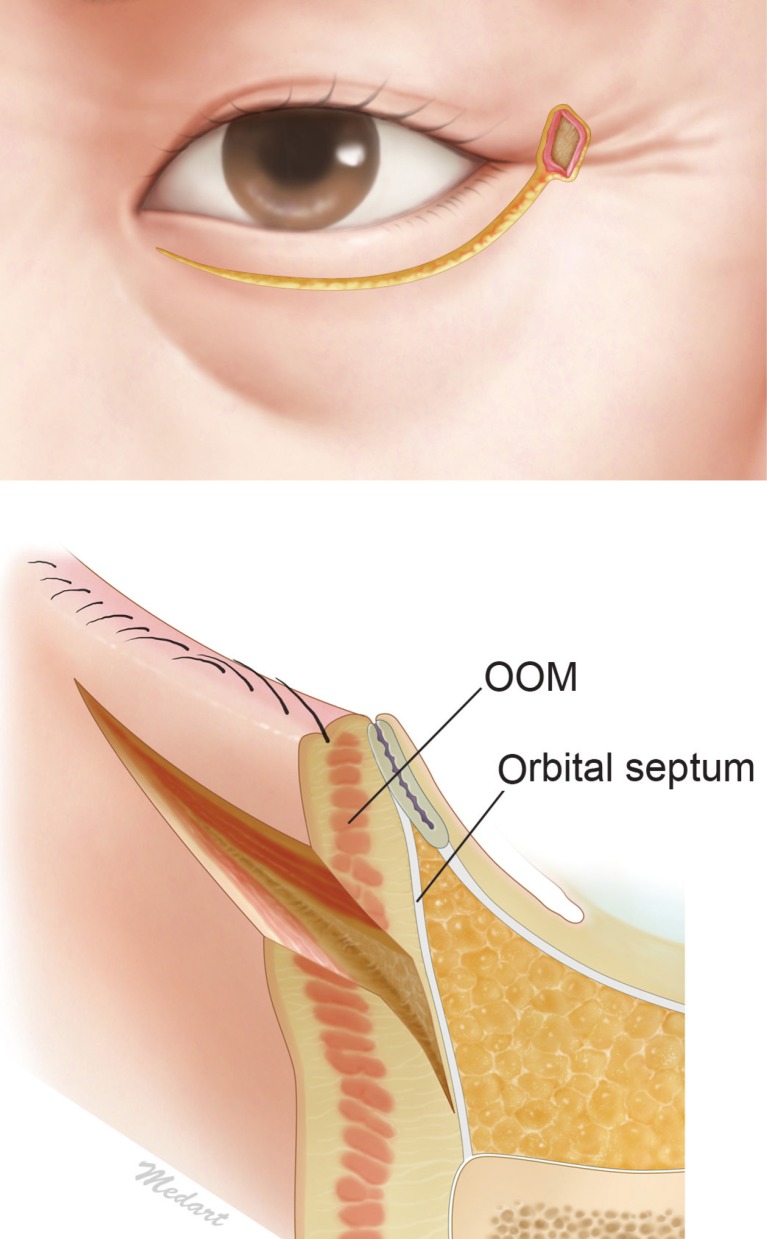
We made an incision from the lateral crow's feet to such a depth that the orbital septum could be seen as the underlying structure of the orbicularis oculi muscle (OOM) in the visual field, thus creating a hole. A small mosquito was placed through this hole and then used to dissect between the OOM and the orbital septum along the medial side of the lower eyelid.
This was followed by the submuscular dissection, by which a muscle flap was elevated to the inferior orbital rim (IOR). Then, the arcus marginalis was released. With the supraperiosteal dissection, we removed and repositioned the periorbital fat. The OOM flap was elevated laterally to the skin and the OOM through a subcutaneous dissection of them. Following the elevation of the OOM flap, we performed suspensory fixation of its orbital and preseptal portions to the lateral orbital periosteum (LOP) or the lateral canthal raphe while exerting a tension to them to a certain degree. The first step of the fixation is known to play a definite role in creating the lower eyelid tightness and its overall contour, for which it would be mandatory to identify sites for the formation of the appropriate lower eyelid tightness while retracting the orbital portion of the OOM using a forcep, this followed by the fixation using a 4-0 vicryl to the LOP that is located right below the superficial lateral canthal tendon (Fig. 3).
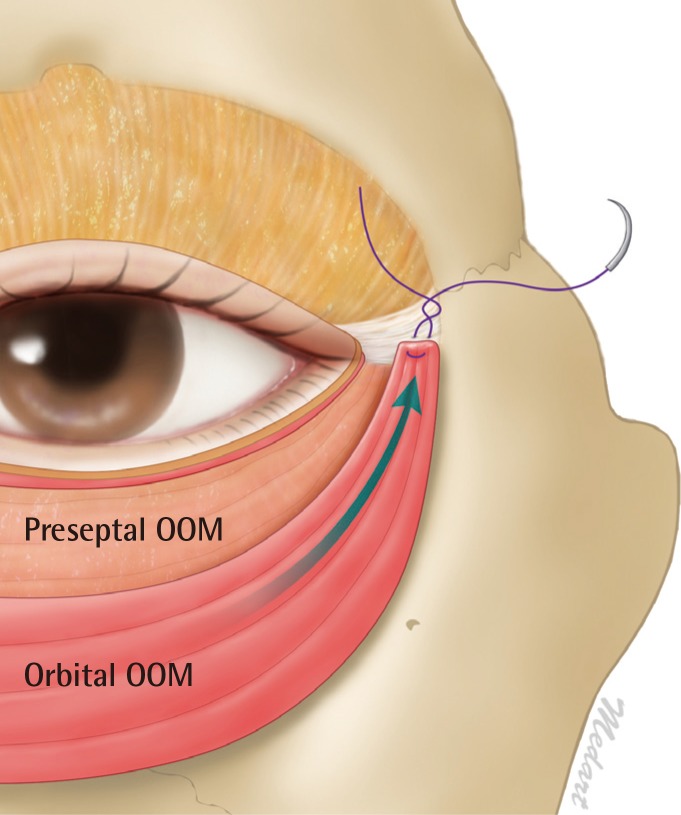
The first step of the fixation. To identify sites for the formation of the appropriate lower eyelid tightness and its overall contour while retracting the orbital portion of the orbicularis oculi muscle (OOM) using a forcep, we fixed it to lateral orbital periosteum which is located right below the superficial lateral canthal tendon.
The second step of the fixation is known to play a definite role in creating the pretarsal fullness, for which it would be mandatory to identify sites for the formation of the appropriate pretarsal fullness while retracting the preseptal portion of the OOM using a forcep. Then, while carefully examining the size, location and shape of the protruded part of the pretarsal portion of the OOM, we fixed the preseptal portion of the OOM to the LOP or superficial lateral canthal tendon, which is higher as compared with the first step of the suspensory fixation (Fig. 4). In patients who had a greater amount of the OOM at the pretarsal fullness, surgeons should appropriately dissect it after the fixation. In patients with a weak contour, they should perform a fixation procedure at another site between the pretarsal and preseptal portion of the OOM, thus creating natural contours.
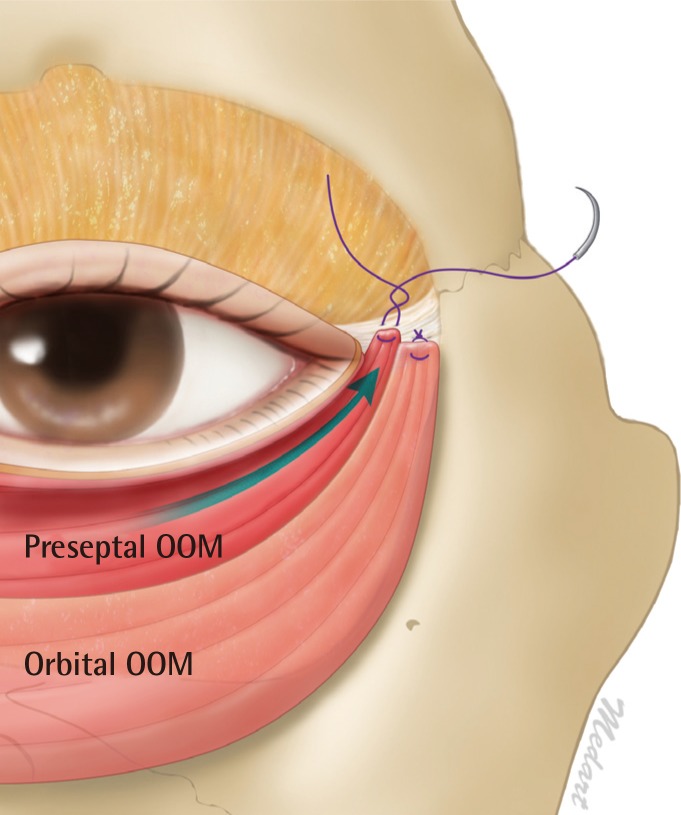
The second step of the fixation. To identify sites for the formation of the appropriate pretarsal fullness while retracting the preseptal portion of the orbicularis oculi muscle (OOM) using a forcep, we fixed the preseptal portion of the OOM to the lateral orbital periosteum or superficial lateral canthal tendon, which is higher as compared with the first step of the suspensory fixation.
The location of the fixation may vary depending on the status of the eyes of patients. In other words, it should be higher in patients with lagophthalmos and lower in those with small eyes or enophthalmos.
After the fixation of the OOM flap, skin incision was solely performed on the lateral side. On the medial side, however, patients were recommended to open their mouth. While preventing the excessive dissection, surgeons should preoperatively mark the target skin and then perform deepithelization of the skin only.
After the deepithelization, the residual flap was spontaneously overlapped with the pretarsal portion of the OOM. This eventually contributes to marked appearance of the pretarsal fullness, which is helpful for surgeons to confirm the formation of the pretarsal fullness on the OOM which had been tightly fixed. Finally, the skin was sutured with a 7-0 nylon, for which we minimized the formation of scars by sufficiently involving the skin and dermal layer.
To summarize, our surgical procedures are as follows: 1) We made a bevel incision, thus shortening the operation time and avoiding damages to the adjacent normal tissue through a one-step approach to the LOP while preserving the pretarsal portion of the OOM that is associated with the pretarsal fullness. 2) We performed two steps of the suspensory fixation at the appropriate sites of the OOM, thus creating natural contours of pretarsal fullness as well as tightening of the lower eyelid skin (Fig. 5). 3) As compared with previous methods for forming the pretarsal fullness, where the pretarsal and preseptal portions of the OOM are sutured more than three times, our methods can prevent the possible formation of scarring granulomas and bulky and irregular pretarsal fullness that can result from unnecessary suturing of the muscle on both sides [1].
Notes
No potential conflict of interest relevant to this article was reported.