Pseudoaneurysm Leading to Necrotizing Fasciitis at the Femoral Arterial Puncture Site
Article information
Abstract
In this article, we present two cases of femoral pseudoaneurysm (PA) at the femoral arterial puncture site followed by necrotizing fasciitis, which is rare but can be fatal when not managed appropriately. PA was revealed by lower-extremity angiography and color-flow Doppler ultrasonography. Hematoma removal, thrombolysis, and bleeder ligation with Gelfoam were repeatedly performed by a vascular surgeon. When necrotizing fasciitis developed, aggressive surgical drainage and creation of a viable wound bed for reconstruction were mandatory. We adopted a vacuum-assisted closure device (Kinetics Concepts International) as the standard treatment for complicated, serious, infected PA of the puncture site. Excellent clinical outcomes were obtained.
INTRODUCTION
The femoral arterial puncture site for angiography or vascular catheterization may become infected or necrotized, requiring meticulous management. Although rare, pseudoaneurysm (PA) and huge hematomas may also develop at the femoral arterial puncture site. These problems usually require urgent management, including anticoagulation therapy or radiologic intervention, and sometimes hematoma removal or PA and vascular repair. The soft tissue and skin may be superimposed by infection, and in rare cases, fatal necrotizing fasciitis may develop and extend to the adjacent areas. Necrotizing fasciitis, a life-threatening surgical emergency, requires aggressive surgical debridement of the necrotic and infected tissue, but the affected site cannot be immediately covered with a skin graft or flap. We dealt with two cases of necrotizing fasciitis that developed after the removal of PA at the femoral arterial puncture site; the wounds were treated with a vacuum-assisted closure device (VAC; Kinetics Concepts International, San Antonio, TX, USA).
CASES
Case 1
A 78-year-old man with ischemic heart disease underwent cardiac catheterization and percutaneous transluminal coronary angioplasty via the femoral artery. His premorbid condition included old age, liver cirrhosis, renal cell carcinoma, diabetes mellitus, and significant ischemic cardiomyopathy. Six days following discharge from the hospital, the patient experienced severe sharp pain in the right groin with no skin discoloration of the right lower extremity. On physical examination, a pulsatile mass was noted in the right groin. Lower-extremity angiography revealed a PA of the superficial femoral artery (Fig. 1). Hematoma removal and bleeder ligation were performed by a vascular surgeon. The affected part of the superficial femoral artery was freed, the aneurysm was opened along its length, and the thrombus was evacuated. A heparin infusion was begun postoperatively.
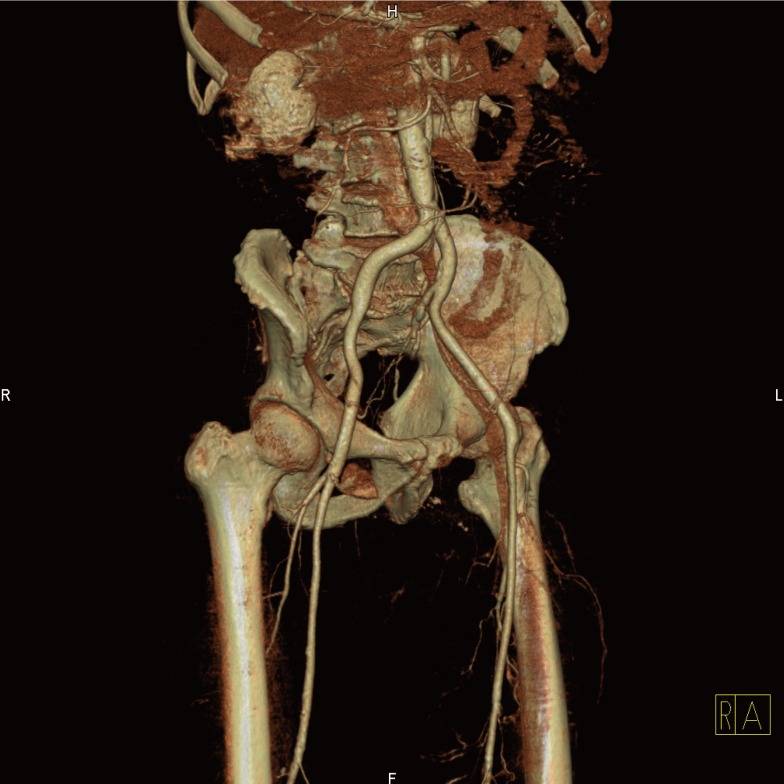
Case 1: lower extremity CT angiographic findings
The computed tomography (CT) angiographic findings revealed a pseudoaneurysm of the superficial femoral artery, at the puncture site, in a patient who underwent cardiac catheterization.
Five days later, the patient developed progressive abdominal pain, fever, vomiting, skin discoloration, and wound induration (Fig. 2). A laboratory study revealed that the white blood cell count was 2000/µL, erythrocyte sedimentation rate (ESR) level was 11 mm/hr, and reactive protein-C (CRP-C) level was 17.91 mg/dL; all these were mildly elevated values. Further, the creatine kinase-MB (CK-MB) level was in the normal range, but the myoglobin level was elevated to 174 ng/mL (normal range, 22-75 ng/mL). The sodium level was found to be 132 mmol/L (normal range, 135-153 mmol/L), a slightly lowered level, and blood urea nitrogen (BUN) was 25.6 mg/dL (normal range, 8-20 mg/dL). Computed tomographic scans of the abdomen and perineal region revealed fluid accumulations involving multiple subcutaneous spaces and the peritoneum. The patient also had ileus of multiple bowel loops (Fig. 3). At that time, he was diagnosed with necrotizing fasciitis of the upper thigh, abdomen, and perineum. The necrotic wound was serially excised, and treatment was performed with the VAC device. VAC therapy was conducted for a period of 12 days (Fig. 4). The patient had an uneventful recovery with a normal range of laboratory results and finally underwent wound closure (Fig. 5).

Case 1: necrotizing fasciitis at femoral arterial puncture site
Diffuse hematoma in the lower abdomen and multiple areas of localized skin and soft tissue necrosis and induration.
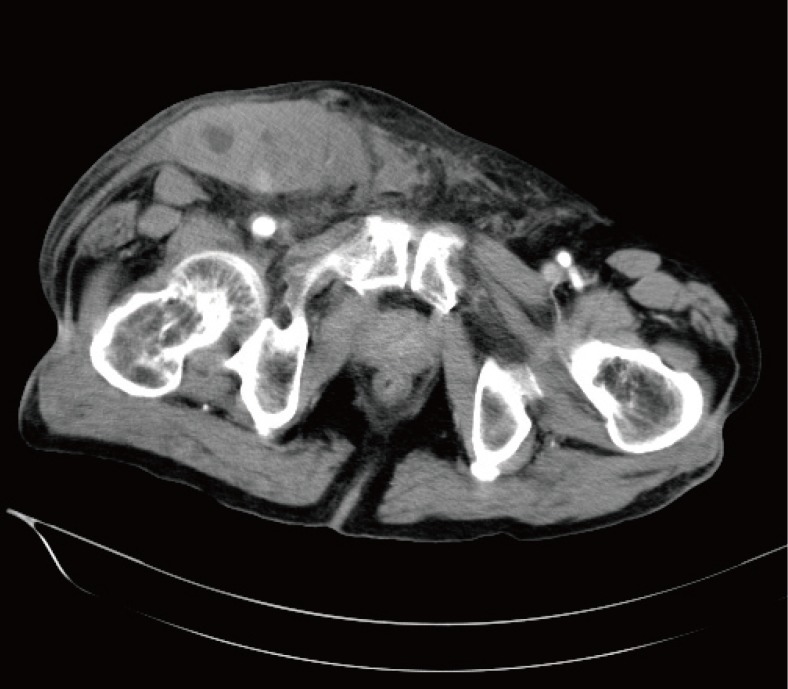
Case 1: contrast-enhanced CT findings of necrotizing fasciitis
Massive subcutaneous tissue edema, fluid collection, muscle swelling, and a large, diffuse hematoma on computed tomography (CT).

Case 1: negative pressure wound therapy for treatment of choice
The necrotic wound was serially excised and treated with the negative-pressure wound therapy device for 12 days. Healthy granulation tissue was present.
Case 2
A 46-year-old woman with symptoms of hemoptysis underwent bronchial angiography via the femoral artery. The patient's premorbid conditions were liver cirrhosis, chronic renal failure, diabetes mellitus, and obesity. However, upon the patient's return to the emergency room, she had a huge hematoma at the femoral arterial puncture site. Color-flow Doppler ultrasonography revealed a giant hematoma and hemorrhagic liquid at various concentrations in the upper third of the right thigh (Fig. 6). Angiography revealed a PA of the superficial femoral artery. Thrombolysis and bleeder ligation with Gelfoam were performed twice by an interventional radiologist. However, on the fourth postoperative day, the patient developed intense thigh swelling accompanied by bleeding from the surgical wound, induration, and marked tenderness. Seven days later, she was diagnosed with necrotizing fasciitis of the upper thigh, abdomen, and perineum (Fig. 7). A laboratory study revealed that the white blood cell count was 12,870/µL, ESR level was 29 mm/hr, and CRP level was 28.48 mg/dL (normal range, 0-0.5 mg/dL); all these values were mildly elevated. Further, the CK-MB level was elevated to 10.7 ng/mL (normal range, 0.1-5.8 ng/mL) and the myoglobin level was elevated to 565 ng/mL (normal range, 22-75 ng/mL). The sodium level was found to be 142, which was a slightly lowered level, and BUN was 27.3 mg/dL (normal range, 8-20 mg/dL). The necrotic wound was serially excised, and treatment was performed with the VAC device. The VAC therapy was conducted for a period of 21 days. However, the patient died of multiorgan failure and aspiration pneumonia.
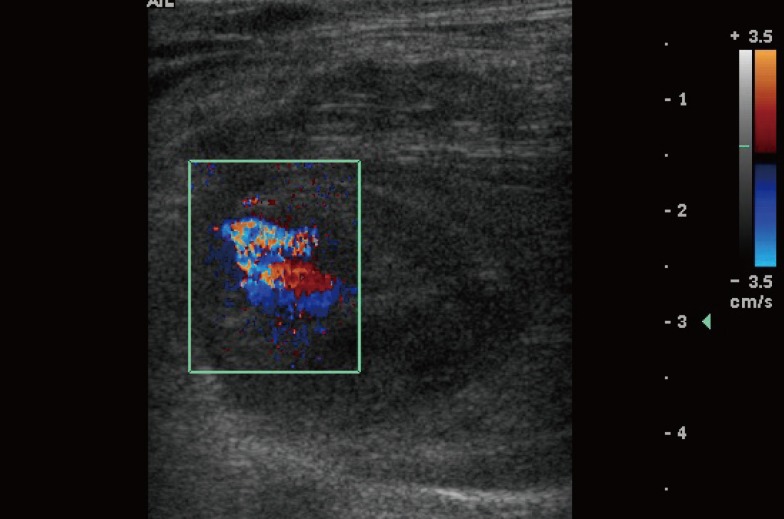
Case 2: color-flow Doppler ultrasonographic findings of PA
The transverse ultrasonographic view showing a short-necked pseudoaneurysm (PA) with spiral flow within the aneurysm sac.
DISCUSSION
Although rare, PA may develop at a femoral arterial puncture site. Treatment demands a joint-team approach from an early stage, including discussions about the anticoagulation regimen, timing of the surgery, planning of the incision, and so on. A plastic surgeon's participation is required for evaluating skin and soft tissue viability right from the early procedures [1].
PA generally results from arterial trauma or occurs at the site of surgery [2]. The extravasation of blood into subcutaneous tissues is surrounded by a pseudo-capsule of fibrous tissue within the adjacent soft tissue. The incidence of femoral arterial PA has been determined to be up to 1% of the patients undergoing diagnostic studies and increases to 3.2% when cardiac intervention is performed [1]. Although arteriography has remained the standard of diagnosis, in cases of an extreme low flow into the PA, arteriography can result in incomplete opacification and size underestimation [2]. Duplex ultrasound has recently become the diagnostic choice for evaluating the PA size, the thrombotic material inside, and the communication between PA and the artery [3]. Many PAs require only observation; radiological treatment options include ultrasound-guided compression repair, embolization, and thrombin injection [1]. Vascular surgery is required when radiological techniques fail or the patient is unstable.
In this report, two cases of PA complicated with necrotizing fasciitis are discussed. Necrotizing fasciitis is an advancing soft tissue infection with extensive fascial necrosis that may be fatal [4]. It begins with constitutional symptoms of fever and chills with minimal skin viability but is soon characterized by rapidly spreading necrosis of the soft tissue and fascia. The extent of the affected tissue cannot be easily predicted. Early surgical debridement of all of the affected tissues is the only treatment option for controlling the source of infection and can be life-saving [4]. Hence, reconstruction of the wound with a skin graft or muscle flap is required in many cases. However, reconstruction of the defect can be considered only after the infection has been resolved and healthy granulation tissue is present [4]. Negative pressure removes the interstitial fluid and edema in order to improve tissue oxygenation. It also removes inflammatory mediators that suppress the normal progression of wound healing [5]. The granulation tissue forms relatively rapidly, and the wound bacterial count is decreased to <105 organisms per gram of tissue [5]. Gabriel et al. [6] demonstrated the use of a VAC system for temporizing wounds, enabling surgeons to perform less complex reconstructions of major soft tissue defects.
Melchionda and Pession [7] also introduced this negative-pressure therapy for two children with malignancy who developed necrotizing fasciitis. They proved its usefulness for constant debridement and removal of secretions and maintaining cleanliness of the wound area when other conventional techniques had failed to achieve wound closure.
This article describes the role of the plastic surgeon in dealing with femoral arterial PAs of an interventional puncture site that result in necrotizing fasciitis. The introduction of this technique using the VAC device as an alternative treatment for complicated and seriously infected PAs resulted in excellent clinical outcomes.
Notes
No potential conflict of interest relevant to this article was reported.

