Early Surgical Site Infection Following Tissue Expander Breast Reconstruction with or without Acellular Dermal Matrix: National Benchmarking Using National Surgical Quality Improvement Program
Article information
Abstract
Background
Surgical site infections (SSIs) result in significant patient morbidity following immediate tissue expander breast reconstruction (ITEBR). This study determined a single institution's 30-day SSI rate and benchmarked it against that among national institutions participating in the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP).
Methods
Women who underwent ITEBR with/without acellular dermal matrix (ADM) were identified using the ACS-NSQIP database between 2005 and 2011. Patient characteristics associated with the 30-day SSI rate were determined, and differences in rates between our institution and the national database were assessed.
Results
12,163 patients underwent ITEBR, including 263 at our institution. SSIs occurred in 416 (3.4%) patients nationwide excluding our institution, with lower rates observed at our institution (1.9%). Nationwide, SSIs were significantly more common in ITEBR patients with ADM (4.5%) compared to non-ADM patients (3.2%, P=0.005), and this trend was observed at our institution (2.1% vs. 1.6%, P=1.00). A multivariable analysis of all institutions identified age ≥50 years (odds ratio [OR], 1.4; confidence interval [CI], 1.1-1.7), body mass index ≥30 kg/m2 vs. <25 kg/m2 (OR, 3.4; CI, 2.6-4.5), and operative time >4.25 hours (OR, 1.9; CI, 1.5-2.4) as risk factors for SSIs. Our institutional SSI rate was lower than the nationwide rate (OR, 0.4; CI, 0.2-1.1), although this difference was not statistically significant (P=0.07).
Conclusions
The 30-day SSI rate at our institution in patients who underwent ITEBR was lower than the nation. SSIs occurred more frequently in procedures involving ADM both nationally and at our institution.
INTRODUCTION
Implant-based breast reconstruction rates continue to increase across the United States as a percentage of total breast reconstructions [1,2,3]. Immediate tissue expander breast reconstruction (ITEBR) with or without acellular dermal matrix (ADM) remains the most common form of post-mastectomy reconstruction [4]. Many studies have demonstrated that surgical site infections (SSIs) following ITEBR result in significant patient morbidity and health care costs [5]. The American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP) database provides outcome data from a wide range of centers, thereby creating national standards for postoperative complications. As a result, individual institutions are increasingly interested in benchmarking their outcomes against national standards in an attempt to improve quality of care and patient safety. This study aims to determine the 30-day SSI rate of a single institution and benchmark it against that among participating national institutions for quality improvement purposes.
METHODS
Data source
Women who underwent mastectomies followed by ITEBR with or without ADM between 2005 and 2011 were identified using the ACS-NSQIP database. The ACS-NSQIP program has developed a large, prospective, nationally validated, multi-institutional database that collects variables from patients undergoing inpatient and outpatient procedures at over 250 participating university and private hospitals. The variables analyzed in this study included patient demographics, preoperative comorbidities, intraoperative proceedings, and postoperative morbidities for the 30-day period after the procedure. The definitions of the variables collected by the ACS-NSQIP program can be found on their website [6]. Current audits have shown a disagreement rate of less than 2% for program variables using this database [7]. Although the ACS-NSQIP program and participating institutions have collected these data, they are not responsible for the statistical validity or the authors' interpretations and/or conclusions of the data.
Cohort identification
Women over the age of 18 who underwent mastectomies followed by ITEBR were identified using the Current Procedural Terminology codes for mastectomies (codes 19180, 19182, 19240, 19301, 19302, 19303, 19304, 19305, 19306, or 19307) for their primary procedure, and their concurrent tissue expander placement procedures (code 19357) were identified in the ACS-NSQIP database. In addition, those who received acellular dermal matrix were identified (code 15330). The subset of these patients treated at our institution was also identified. Patient variables included age, body mass index (BMI) (<25, 25-29.9, and ≥30 kg/m2), smoking status, steroid use, diabetes mellitus, preoperative radiation, year of operation, and operative time (>4.25 hours vs. ≤4.25 hours quartiles), focusing on the longest operations. The primary goal of this study was to assess the postoperative 30-day SSI rate. Three types of SSIs have been defined: superficial (limited to the skin and subcutaneous tissue), deep (involving deep tissues including fascia and muscle), and organ space (involving the surrounding organs) [8]. Unless otherwise specified, patients from our institution were excluded from any nationwide data reported in this study.
Statistical analysis
Demographic, clinical, and procedural characteristics of patients who did and did not develop SSIs were compared using chi-square tests; Fisher's exact tests were used when low expected cell counts were observed. Multivariable logistic regression was used to determine patient characteristics independently predictive of 30-day SSIs and to assess the difference in likelihood of SSIs at our institution compared to other institutions in the ACS-NSQIP database. Results were considered significant if P-values were less than 0.05. Patient characteristics that resulted in a P<0.05 in the univariate analysis or that were deemed to be clinically relevant were included in the multivariable logistic regression model as independent variables, with the SSI rate as the dependent variable. Statistical analyses were performed in SAS ver. 9.3 (SAS Institute Inc., Cary, NC, USA).
RESULTS
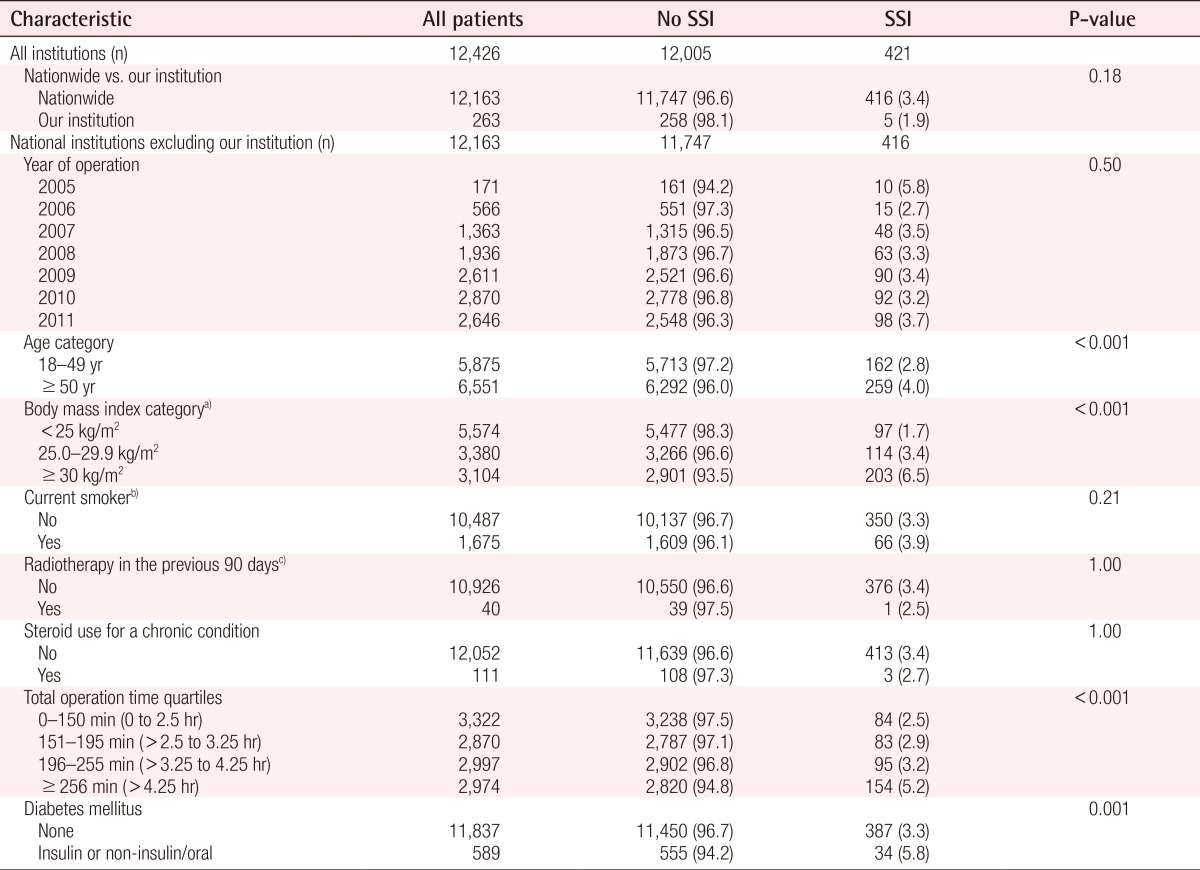
A total of 12,163 patients underwent ITEBR between 2005 and 2011, including 263 patients at our institution (Table 1). Over that period, ADM was used in 15.5% of all ITEBR procedures across the nation excluding our institution, and the percentage of cases with ADM steadily increased from 4.4% in 2006 to 22.5% in 2011 (Table 2). At our institution, 53.2% of patients received ADM from 2005 to 2011, with an increase in ADM use from 57.7% to 86.4% among cases recorded in 2008 and 2011, respectively (Table 2). ADM was not used in breast reconstructions at our institution before 2008, and the use of ADM during breast reconstructions was not seen in the NSQIP participant use data file until 2006.
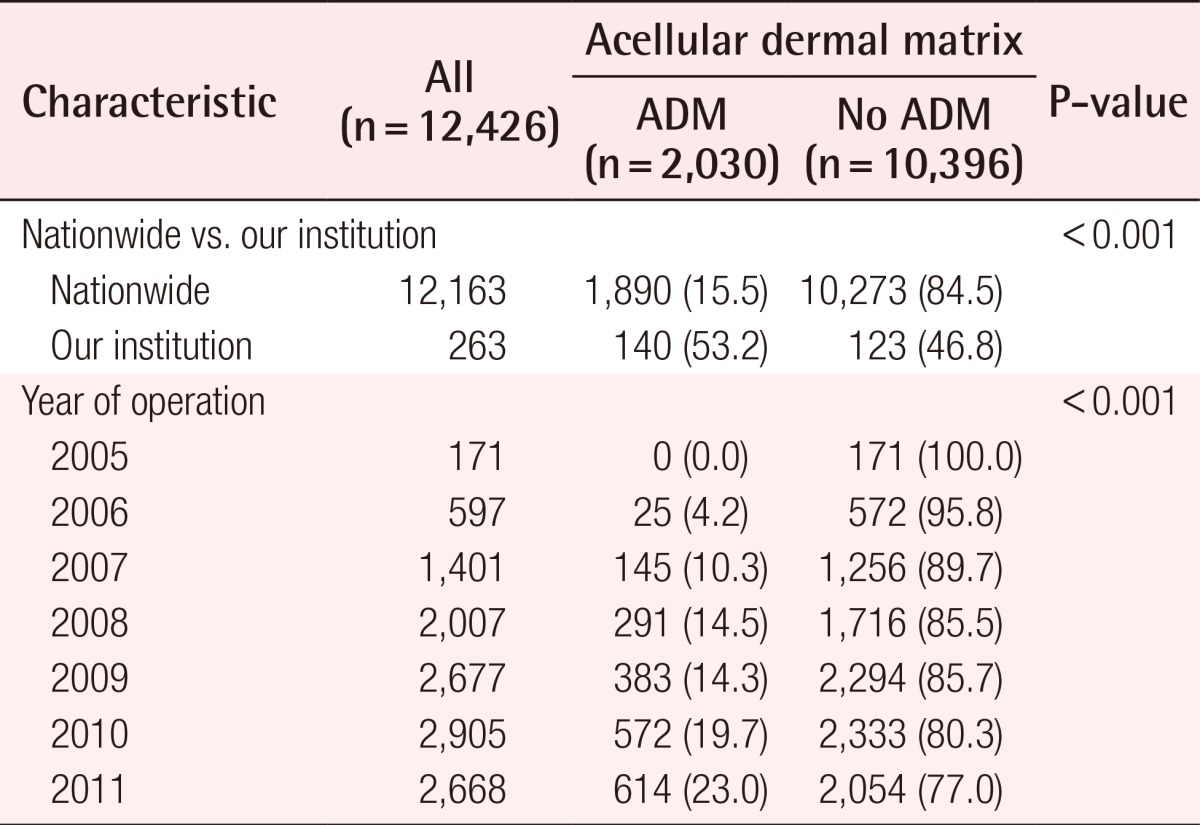
Those with acellular dermal matrix (ADM) compared to those with no ADM in our institution, nationwide, and each year between 2005 to 2011
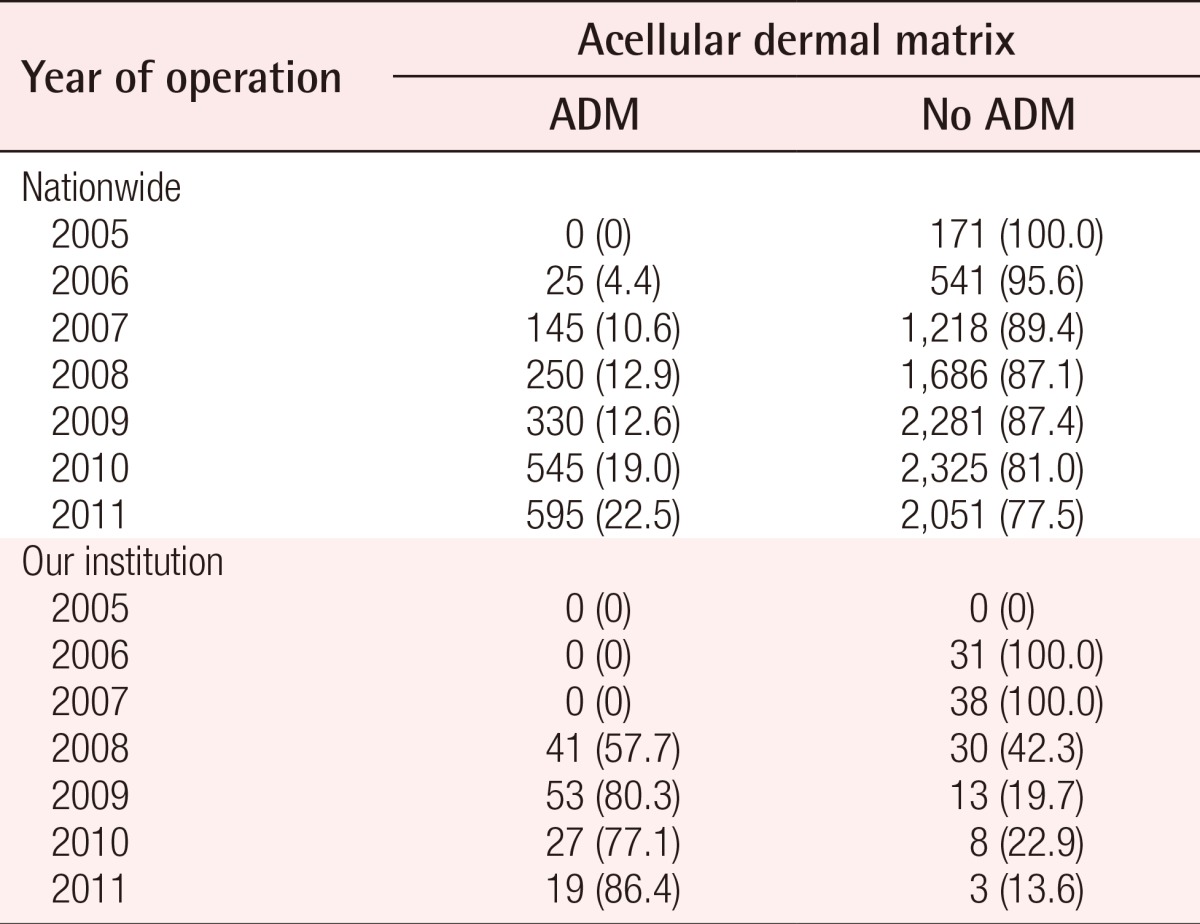
Those with acellular dermal matrix (ADM) compared to those with no ADM by year in our institution and nationwide
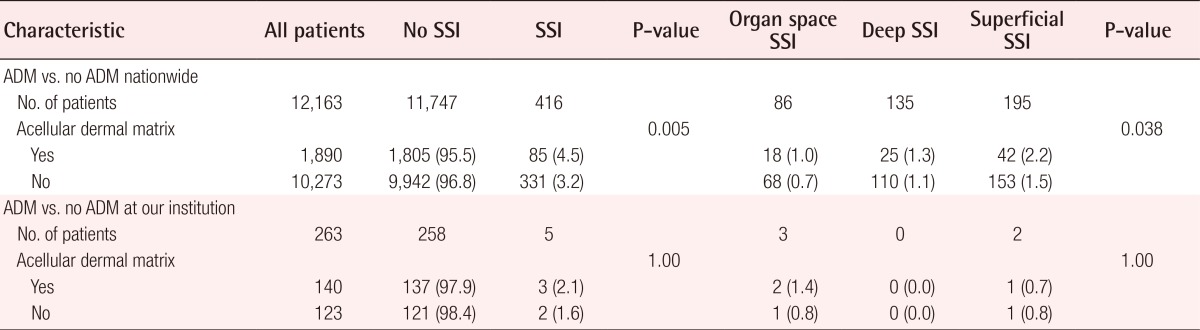
Nationwide, SSIs occurred in 416 patients (3.4%) compared to five patients (1.9%) at our institution (Table 3). The annual SSI rate across national institutions from 2005 to 2011 varied from 2.7% to 5.8%, but this variation was not statistically significant (P=0.50). The occurrence of 30-day SSIs was significantly greater in ADM patients compared to non-ADM patients nationally (4.3% vs. 3.2%, respectively; P=0.010). This trend was also observed at our institution (2.1% vs. 1.6%, respectively), although it was not statistically significant (P=1.00) (Table 4).
Of the three types of SSIs, the most common was superficial, followed by deep, and finally organ space SSI (Table 4). A four-level SSI variable (none, organ space, deep, and superficial) was then created and patients with more than one type of SSI were assigned to the most serious category, which was organ, followed by deep, and then superficial. SSIs still proved to be significantly more common in ADM patients when compared to non-ADM patients (P=0.038). However, despite the low numbers of patients, this trend was not observed at our institution (P=1.00) (Table 4).
Across the nation, the univariate analysis identified age ≥50 years (P<0.001), a higher BMI (P<0.001), diabetes (P=0.001), and a greater total operative time (P<0.001) as risk factors for SSIs. In addition, the absence of current smoking was associated with lower SSI rates, but this trend was not statistically significant. Radiotherapy and the absence of steroid use did not appear to affect the SSI rate (P=1.00 and P=1.00, respectively) (Table 3).
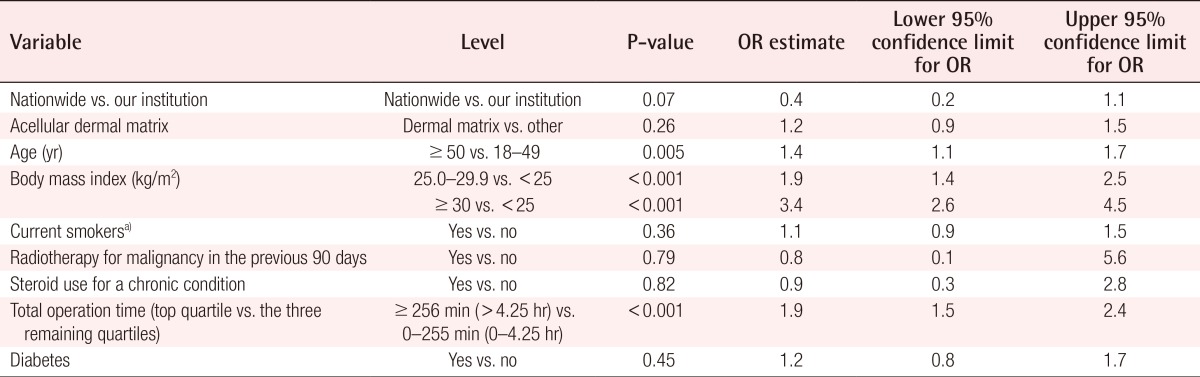
The multivariable analysis including all institutions identified age ≥50 years (odds ratio [OR], 1.4; confidence interval [CI], 1.1-1.7), BMI ≥30 kg/m2 vs. <25 kg/m2 (OR, 3.4; CI, 2.6-4.5), and operative time >4.25 hours (OR, 1.9; CI, 1.5-2.4) as risk factors for SSIs. Univariate and multivariable analysis of SSI risk factors could not be performed separately for patients at our institution due to an insufficient total number of cases of SSIs during this period. After adjusting for clinical and procedural characteristics, our institutional SSI risk was lower than other institutions in the ACS-NSQIP database (OR, 0.4; CI, 0.2-1.1), although this difference was not statistically significant (P=0.07) (Table 5).
DISCUSSION
ITEBR is the most common modality for breast reconstruction in the United States, with several studies showing increasing rates in recent years [1,2,3]. The use of ADM as an adjunct in ITEBR has also become more common, with numerous studies demonstrating its benefits [9,10,11], including increased expander fill volume on initial operation. These benefits reduce the need for additional postoperative expansions, improve the lower pole coverage, and enhance the inframammary fold definition [9,10,11]. However, other studies have demonstrated increased rates of postoperative complications such as SSIs and seroma among this patient population [12,13].
Our goal was to determine the 30-day SSI rate of our institution among patients who underwent ITEBR with or without the use of ADM and to compare our institution's rate to that of other institutions on a national level. We identified an overall SSI incidence of 3.4% in other ACS-NSQIP institutions, compared to 1.9% at our institution (P=0.18). SSIs were significantly more common in ADM patients compared to non-ADM patients nationally (4.5% vs. 3.2%, respectively; P=0.005), and this trend was also observed at our institution (2.1% vs. 1.6%, respectively; P=1.00). Unsurprisingly, organ space SSIs, which is the most invasive and severe type of SSI, were observed less frequently than deep and superficial SSIs were nationwide. When analyzed by subtype, SSIs were still more common in ADM patients than non-ADM patients (P=0.038). Several studies have demonstrated similar findings [14,15]. Chun et al. [15] showed increased seroma and infection rates in patients reconstructed with ADM, although they proposed that the increased infection rate may have been mediated by seroma and/or native breast skin flap necrosis in this group of patients.
Many modalities have been implemented to reduce these complications, including judicious drain placement with strict criteria for removal [14], the consistent use of perioperative antibiotics [16], and a strict sterile technique in the operating room [16]. More recently, the use of sterile ready-to-use ADM has been advocated [15]. Weichman et al. [17] compared ready-to-use ADM to aseptic ADM in a patient cohort of 546 reconstructed breasts and demonstrated that ready-to-use ADM was associated with a decrease in the overall infection rate, major infection rate, and the need for implant explantation. They concluded that the use of ready-to-use ADM mitigates the risk of infectious complications when compared with aseptic ADM [17]. At our institution, a strict sterile technique and consistent administration of perioperative antibiotics while performing these procedures are routine. We also change our gloves before handling the prosthesis and avoid contact between the ADM and the patient's skin before insertion and placement. The use of drains is also routine in ITEBR, with strict criteria for removal when the output is <30 mL per day for two consecutive days. Finally, oral antibiotics are routinely administered until the drains are removed. Overall, there has been a shift towards the use of sterile ready-to-use ADM at our institution in the last few years, although this is not reflected in the ACS-NSQIP database. It is possible that some of these modalities help explain the lower SSI rates at our institution when compared to the national average. However, we recognize that the possible effect of these institutional practices is anecdotal and have not been confirmed by a rigorous trial.
Several risk factors for SSIs were identified in this study, including increased BMI, age, and total operative time. Obesity is a well-established risk factor for surgical complications and wound healing. We found that across all institutions, patients with a BMI <25 kg/m2 had a 1.7% SSI rate, compared to a 6.5% SSI rate in patients with a BMI ≥30 kg/m2 (P<0.001). These findings corroborate those of other publications [18,19]. According to Fischer et al.'s [18] review of the impact of obesity on breast reconstruction outcomes, patients with higher BMIs had a higher incidence of comorbidities and experienced higher complication rates, including wounds, medical complications, infectious complications, major surgical complications, prosthesis loss, and return to the operating room, all of which were statistically significant.
Increasing age (≥50 years) was also associated with higher SSI rates by both univariate analysis (P<0.001) and multivariable logistic regression (OR, 1.4; CI, 1.1-1.7). The univariate analysis allows us to infer that this patient group has a higher incidence of comorbidities that would make them more susceptible to SSIs. However, the statistically significant results of the multivariable analysis suggest that age in itself is an intrinsic risk factor or that we did not or could not control for other risk factors in our model. This finding corresponds to the findings of other previously published studies [20,21]. Shermak et al. [20], in their study of 2,156 reduction mammoplasties, found that women older than 50 years were more likely to experience infection and wound healing problems. They concluded that hormonal deficiencies might partially account for this finding.
Longer total operative times were also associated with a progressively higher SSI rate nationally (excluding our institution). Procedures lasting <2.5 hours had a 2.5% SSI occurrence compared to those that lasted >2.5-3.25 hours (2.9%), >3.25-4.25 hours (3.2%) and >4.25 hours (5.2%), P<0.001. An association between prolonged operative time and complications is well established in the general surgery literature [22,23]. However, Procter et al. [22] show that the determinants of prolonged operative time are multifactorial; therefore, we should interpret these results with caution. In contrast, Fogarty et al. [24] suggest that operative time alone is not a major determinant of postoperative complications, and that the type of surgery and the patient's overall condition are more important predictors of the outcome.
This study has several limitations. First, this analysis was limited to 30-day outcomes and a potentially significant group of patients can present with SSIs more than 30 days after the operation. These patients may also have drains in place, theoretically increasing their risk of SSIs. Nevertheless, we would expect that patients with SSIs more than 30 days after the operation would present equally frequently at our institution and other institutions nationwide, resulting in a similar trend in SSI rates. However, including data from SSIs occurring more than 30 days after surgery might have provided us with a sufficient number of cases to evaluate SSI risk factors specific to our institution. Another limitation is selection bias in the ACS-NSQIP database. Hospital participation in NSQIP is voluntary, and although the database includes a large number of both university and private hospitals, there may be a selection bias that affects the accuracy of the data when benchmarking against national averages. In addition, only a percentage of patient cases within any given participating institution are included in the database. Although this selection is random, it does not completely eliminate bias. Finally, many important postoperative complications relevant to our patient population are not captured by the ACS-NSQIP, such as mastectomy skin flap necrosis and seroma.
Overall, the 30-day SSI rate at our institution in patients undergoing ITEBR was lower than the nationwide rate as reflected in the ACS-NSQIP database. Instances of SSIs were more common in procedures involving ADM both nationally and at our institution. National risk factors for SSIs include increasing age, obesity, and longer operative times; however, the insufficient number of cases at our institution did not allow for the benchmarking of these risk factors at a national level. Further work is under way to confirm whether SSI risk factors at our institution are similar to those across the nation. Retrospective cohort studies outside of the ACS-NSQIP database would be necessary to obtain sufficient patient numbers to benchmark SSI rates against that in the rest of the nation. Nevertheless, ongoing comparisons between individual institutions and the national ACS-NSQIP database are important to identify roles for quality improvement projects to improve surgical outcomes.
Notes
This paper was presented at the Plastic Surgery Research Council on March 7-9, 2014 in New York, NY, USA.
No potential conflict of interest relevant to this article was reported.