Cutaneous Fusariosis in Unprotected Snake Bite Wound of Farmer's Hand
Article information
The genus Fusarium is widespread in soil, plants, and the air, and broad manifestations of human disease can be caused by infection with it, which can be superficial, locally invasive, or disseminated infections, including mycotoxicosis [1]. One of the most frequent aspects of infection by Fusarium species is the development of skin lesions; such lesions are typically the only source for diagnosis [2]. Thus, diagnosis and treatment of human Fusarium infection is usually delayed, causing poor results.
We report on a case of cutaneous fusariosis caused by continuous soil and plant contamination of an open wound that formed after a snake bite on the hand. The infection was ultimately treated and there was no recurrence after three months.
The patient was an 81-year-old, otherwise healthy woman. She was a farmer and had a history of abusing oral corticosteroids due to arthritis from approximately five years until one year ago (2006 to 2011). She was transferred to our hospital with a painful progressive skin ulceration around her right third knuckle and proximal phalanx after a snake bite two weeks earlier (Fig. 1). After the snake bite, she continued working on the farm without wound protection and the bite wound worsened.

Photograph of the subject when she first visited the hospital. There was a painful progressive skin ulceration around the right third knuckle and proximal phalanx after a snake bite two weeks earlier.
First, because she was healthy, the lesion was evaluated for bacterial infection and methicillin-resistant Staphylococcus aureus was cultured from a swab specimen. Intravenous vancomycin was continued for two weeks and the patient underwent serial surgical debridement, and, two weeks later, a full-thickness skin graft surgery was performed. However, one week after surgery, progressive eschar formation was observed from the distal tip of the graft to the distal aspect. At three weeks after surgery, a skin defect and eschar formed from the distal half of the grafted skin to the middle third of the proximal phalanx. We expected possibility of other kind of infection because wound healing was delayed and she has a history of working on the farm without wound protection. She was readmitted to the hospital, and a tissue biopsy was taken. Microscopic examination of the surgical specimen revealed fungal hyphae and necrotic tissue (Fig. 2). However, there was no evidence of immunocompromised status, such as neutropenia basis her laboratory finding and there was not any other systemic symptom. A diagnosis of cutaneous fusariosis was made, and the patient underwent aggressive surgical debridement.
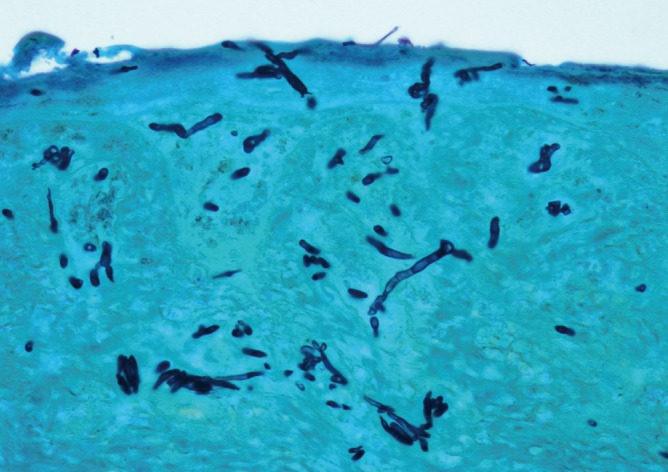
Septate fungal hyphae of Fusarium species in a high-power view of a tissue biopsy specimen (GMS stain, ×400).
Intravenous amphotericin B (Fungizone 50 mg; BMS Pharmaceutical Korea Ltd., Seoul, Korea) 1 mg/kg daily, was started and continued for one week and switched to oral voriconazole (Vfend 200 mg; Pfizer Inc., Seoul, Korea) 200 mg twice daily for four weeks. After ensuring that there were no fungal hyphae or fungi growth in tissue culture, a second operation (full-thickness skin graft) was performed. Six months after the operation, there was no evidence of recurrence (Fig. 3).

A second operation (full-thickness skin graft) was performed, and, three months postoperatively, there was no evidence of recurrence.
The genus Fusarium is widely distributed in plants and soil in temperate and tropical climates. Microscopically, the hyphae of Fusarium have multiple filaments, which are hyaline, septate, 3-8 µm in diameter, and typically branch at acute or right angles. The most frequent human Fusarium isolates are Fusarium solani, Fusarium oxysporum, and Fusarium proliferatum, however, species differentiation may be difficult except in specialized laboratories [3]. Fusarium species possesses several virulence factors, including the production of tricothecene and other mycotoxins. These mycotoxins can suppress humoral and cellular immunity, and cause break down of tissue [4]. Such skin breakdown may precede infection by up to one year [2].
The majority of immunocompetent patients (77%) have a history of recent skin breakdown at the lesion of cutaneous fusariosis, either as a result of trauma (54%) or preexisting onychomycosis (23%) [2]. Skin lesions may vary, including granulomas, ulcers, nodules, mycetomas, necrosis, panniculitis, and intertrigo [5].
For the diagnosis of cutaneous fusariosis, a meticulous physical examination is required for identification of suspicious skin lesions with tissue breakdown and all suspicious lesions should be cultured, and a biopsy should be performed [2]. If Fusarium species are identified in culture or biopsy, aggressive debridement should be performed and antifungal therapy should be administered. Previous guidelines recommended amphotericin B for treatment of fungal infections, including Fusarium infection, however, in a recent analysis, voriconazole was recommended as the most cost-effective therapy [4]. Treatment of cutaneous fusariosis is usually successful. Determination of the endpoint of antifungal treatment should be made by serial tissue cultures and biopsies, until there is no growth in culture and no fungal hyphae in a biopsy.
In our case, because methicillin-resistant Staphylococcus aureus infection was demonstrated by culture, a fungal infection was not considered initially and diagnosis was delayed. In addition, the patient had a history of long-term corticosteroid abuse, which had likely weakened her immune resistance to infection and had caused thinning of her skin. Her skin was broken by a snake bite, and she continued to work on a farm even after the bite without protecting the wound. These events allowed continuous penetration of Fusarium and might easily have enabled colonization.
In a patient who has chronic wounds with sustained farming, fungal infection should be suspected. Also, because skin breakdown due to infection may precede illness by up to one year, it is necessary to obtain a detailed history of the patients' behavior. In addition, a tissue biopsy should be recommended because it provides the only diagnostic clue.
Notes
This work was supported by the Soonchunhyang University Research Fund.
No potential conflict of interest relevant to this article was reported.