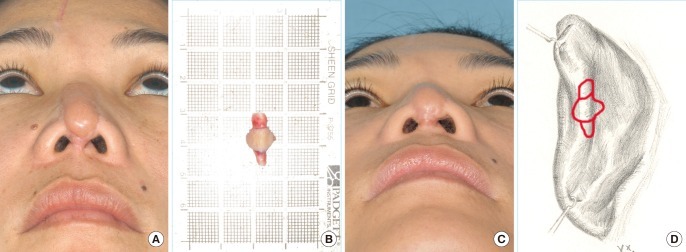
Large Auricular Chondrocutaneous Composite Graft for Nasal Alar and Columellar Reconstruction
Article information
Abstract
Background
Among the various methods for correcting nasal deformity, the composite graft is suitable for the inner and outer reconstruction of the nose in a single stage. In this article, we present our technique for reconstructing the ala and columella using the auricular chondrocutaneous composite graft.
Methods
From 2004 to 2011, 15 cases of alar and 2 cases of columellar reconstruction employing the chondrocutaneous composite graft were studied, all followed up for 3 to 24 months (average, 13.5 months). All of the patients were reviewed retrospectively for the demographics, graft size, selection of the donor site and outcomes including morbidity and complications.
Results
The reasons for the deformity were burn scar (n=7), traumatic scar (n=4), smallpox scar (n=4), basal cell carcinoma defect (n=1), and scar contracture (n=1) from implant induced infection. In 5 cases of nostril stricture and 6 cases of alar defect and notching, composite grafts from the helix were used (8.9×12.5 mm). In 4 cases of retracted ala, grafts from the posterior surface of the concha were matched (5×15 mm). For the reconstruction of the columella, we harvested the graft from the posterior scapha (9×13.5 mm). Except one case with partial necrosis and delayed healing due to smoking, the grafts were successful in all of the cases and there was no deformity of the donor site.
Conclusions
An alar and columellar defect can be reconstructed successfully with a relatively large composite graft without donor site morbidity. The selection of the donor site should be individualized according to the 3-dimensional configuration of the defect.
INTRODUCTION
Reconstructive rhinoplasty to correct a nasal deformity caused by trauma, tumor extirpation, or scar contracture is challenging because it requires the reconstruction of the outer skin, supporting cartilage, and inner mucosal layer of the nose simultaneously in a 3-dimensional shape and functional aspects also have to be taken into account.
To address these challenges, the known techniques have included the local flap, full thickness skin graft, composite graft, and free flap. Among the various nasal reconstruction procedures, the chondrocutaneous composite graft is one of the most advantageous methods because it is possible to reconstruct the structural cartilage along with the inner mucosa and outer skin reconstruction in one stage, and the surgical time is shorter than the other methods. However, it is not used frequently for large defects as it may cause postoperative deformity of the donor site and reduced survival rate of the graft. Brown and Cannon [1] and Lehman et al. [2] concluded that a graft larger than 10 mm is not suitable for the reconstruction because of the limited blood flow, which results in subsequent necrosis of the graft. Nevertheless, the present authors achieved satisfactory results from alar and columellar reconstruction and minimized deformity of the donor site for large defects via selective harvesting of the chondrocutaneous composite graft from the ear and open ointment moisture balance dressing.
METHODS
An institutional review board-approved, retrospective review was carried out on patients who underwent surgery between October 2004 and January 2011 in our department. Patients who underwent nasal reconstruction using a chondrocutaneous composite graft from the ear were identified. Preoperative and postoperative photographs, office charts, and hospital records were reviewed retrospectively for patient demographics and indications for the composite graft, as well as the donor sites of the ear, the size of the graft, result, and complications. Associated demographics included patient age, sex, and former or active tobacco use. Indications for the chondrocutaneous composite graft included alar notching or alar defect, retracted ala, stricture of the nostril, or collapsed columella. The donor sites of the ear for the graft were the helical rim and root, concha, and scapha.
In the cases of alar and nostril reconstruction in which one side required the reconstruction, the midline was marked on the nasal dorsum and the site that needed the reconstruction was found after being compared with the normal side. To make the deformed side similar to the normal side, we analyzed the size, shape, and components of the defect after release, found similar components of the ear for the graft, and harvested the graft. When both sides of the ala and nostril required reconstruction, the design was drawn to release the contracture completely so that it would fit well with the overall nasal structure. All procedures were conducted abiding by the following principles [3]. During the surgery, beveled incisions were performed to increase the contact surface of the recipient site for the graft and a bipolar electrocoagulator was used to minimize the thermal damage to the tissue. For the harvesting of the chondrocutaneous composite graft, epinephrine was not used; only 1% lidocaine was injected. Moreover, the donor site for the harvesting was not standardized but customized for each person based on the components and the figures of the defect, the color of the surrounding tissue, and the unique shape of the each individual's ear. It was approximated precisely without tension. After the operation, the graft was immobilized with Merocele and was kept in moisture balance with antibiotic ointment to improve the success rate of the large composite graft.
RESULTS
Over a 6-year period, 13 patients (17 cases) underwent nasal reconstruction using the chondrocutaneous composite graft. The mean age of the patients was 55 years, with a range of 18 to 71 years, and the patients were 2 males and 15 females. The patients were followed up for 3 to 24 months (average, 13.5 months).
The indications for composite graft included alar notching (n=3), alar defect (n=3), retracted ala (n=4), stricture of nostril (n=5), and collapsed columella (n=2). The causes of nasal deformities were burn scar contracture (7 cases), post traumatic scar (4 cases), smallpox scar (4 cases), defect due to basal cell carcinoma excision (1 case), and scar contracture from implant infection (1 case).
In the 6 cases that required partial or total reconstruction (alar notching, alar defect), we removed the scar tissue of the recipient site with a beveled incision and grafted the composite tissue from the helical rim and root (6×8-10×18 mm; mean, 8.7×13 mm). In the 5 cases of nostril stricture, we released the contracture with wedge-shaped scar excision and grafted chondrocutaneous composite graft from the helical rim and root (7×12-9×15 mm; mean, 9.2×12 mm). In the 4 cases of retracted ala caused by burns, we incised the alar rim and released the scar contracture, grafted slightly larger composite tissue than the defect from the posterior concha of the ear (3×12-9×15 mm; mean, 5×15 mm). In the 2 cases that required columellar reconstruction, we completely released the contracture and harvested the tissue from the posterior scapha (8×8-10×19 mm; mean, 9×13.5 mm). The maximum size of the graft was 10×19 mm and the majority of the patients had a graft larger than 10 mm. But most of grafts led to high rate of success.
Almost all of the patients showed no noticeable deformity on the donor site and showed a successful chondrocutaneous composite graft taken by the 10th day (on average) except one patient with partial necrosis of the graft and delayed healing (Table 1, patient 1) who had been drinking and smoking heavily for a long time (50 pack-years).
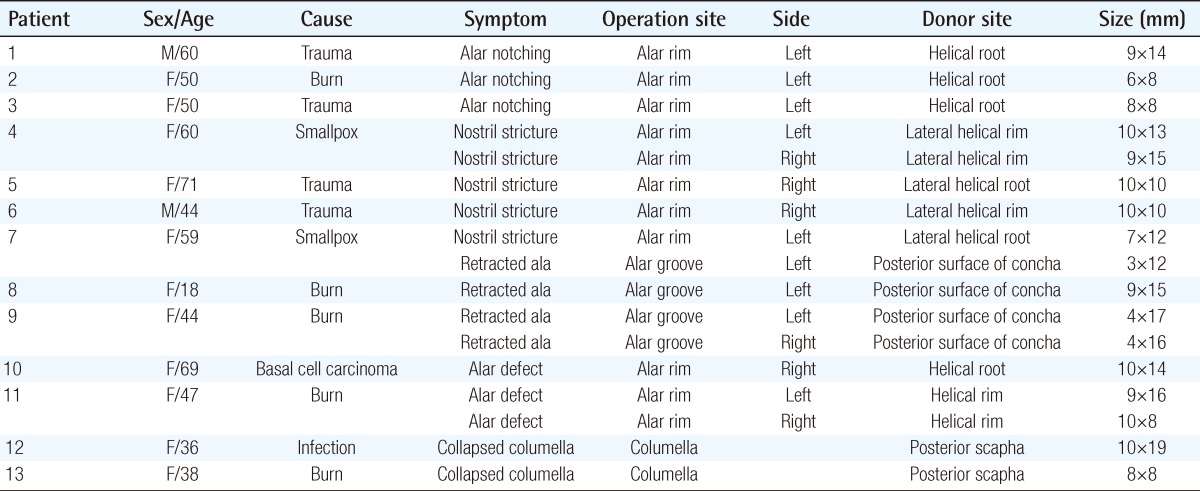
Case 1
A 44-year-old female had retracted alae as a result of a flame burn. She had scar tissue on the alar grooves and retracted alae. We incised the tissue perpendicularly along the alar groove, released the contracture to its maximal degree, harvested chondrocutaneous composite grafts from the posterior concha on both ears, and grafted tissue slightly larger than the size of the defect (4×17 mm, 4×16 mm). Six months after the surgery, we observed the alar contracture to be corrected (Fig. 1).
Case 1
(A) A 44-year-old female with both retracted alae (Table 1, patient 9). A preoperative lateral view shows the retracted ala. (B) The skin surface of 4×17 mm and 4×16 mm chondrocutaneous composite tissue from the concha were grafted. Lateral view 6 months after the operation shows the correction of the retracted ala. (C) The donor site of the ear in this patient. (D) The donor site of the ear 1 year after the operation.
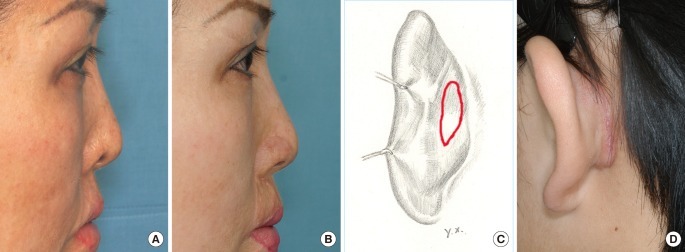
Case 2
A 47-year-old female with an alar defect caused by a scalding burn came to our clinic. She required total alar reconstruction and we incised the scar tissue, increased the contact surface and harvested the chondrocutaneous composite graft from both helices (9×16 mm, 10×18 mm). Six months after the surgery, the ala was natural and symmetrical (Fig. 2).

Case 2
(A) A 47-year-old female with both alar defects after a burn (Table 1, patient 11). Preoperative view shows alar defect. (B) 9×16 mm and 10×18 mm chondrocutaneous composite grafts from the helix were harvested and grafted. A frontal view 6 months after the operation shows improvement. (C) The donor site of the ear in this patient.
Case 3
A 36-year-old female complained of scar contracture of the columella. She had received an augmentation rhinoplasty using a silicone implant but the implant had been removed due to infection 12 years earlier. She had also received a forehead flap to correct her short nose. She had a collapsed columella due to scar contracture. We released the contracture using a columellolabial incision and found the collapsed cartilage (Fig. 3). Afterwards, 10×19 mm composite graft including the ear cartilage and skin was harvested from the posterior scapha and grafted to supplement the cartilage and skin.
Case 3
(A) A 36-year-old female with a collapsed columella after infection (Table 1, patient 12). The columella is broken by scar contracture. (B) A 10×19 mm butterfly-shaped auricular chondrocutaneous composite graft from the scapha was harvested. (C) Worm's eye view 6 months after the operation shows improvement. (D) The donor site of the ear in this patient.
DISCUSSION
The nose is divided into 6 subunits according to their different support structures, skin thicknesses, and properties [4]. Among those, the ala has a 3-dimensional shape and a complex structure with 3 different components; the inner mucous membrane, the cartilage that supports its three-dimensional shape, and the outer skin [5]. The columella also is composed of skin and a cartilage layer. Therefore, it is important to reconstruct the cartilage layer to straighten a disfigured columella effectively and to prevent-columellar shortening. In light of their structural and functional complexity, it is difficult to reconstruct alar and columellar deformities and defects. For the reconstruction of the ala and columella, the size, symmetry, color matching with the surrounding tissues, skin texture, condition of the surrounding tissue, and the donor site should be considered [6]. Various methods including secondary intention, skin graft, composite graft [7], local flap [8,9], and distant flap including free flap [10] are used for the reconstruction of the nose.
The skin graft has good rate of success and is a simple procedure for the reconstruction of a large defect. However, it is difficult to reconstruct the recipient's tissue volume sufficiently. On the other hand, a local flap is relatively simple and is similar in texture and color. However, an additional scar remains on the exposed facial area. In the case of free flaps, the volume of flap can be bulky, and it cannot be used to construct a delicate 3-layered structure.
The composite graft is used for the correction of various full thickness skin defects. The tissues of the helix, antihelix, concha, and lobule are often used as the donor site. The ear composite graft has the following benefits. First, it is possible to reconstruct the 3-layered structure of the ala and harvest the skin and cartilage simultaneously for the reconstruction of the columella. Second, the ear is considerably similar to the ala and columella in the shape, curve, color, and texture. Third, the ear has components with various shapes and curves, so the graft that is the most similar to the recipient site can be harvested. Therefore, we do not have to harvest the unnecessary extra tissue from the ear. The reconstruction would be satisfactory and the donor site deformity can be minimized. Singh and Bartlett [11] achieved a satisfactory result from primary closure without helical rotation, advancement flap or skin graft for a defect less than 15 mm. We were able to obtain good aesthetic results for the donor site with primary closure. Fourth, there is minimal contracture after the successful healing of the graft because of the cartilage included in the graft [12].
However, nasal reconstruction with a composite graft has a high failure rate if the graft is too large. Brown and Cannon [1] and Lehman et al. [2] concluded that a graft larger than 10 mm is not suitable for reconstruction because of the limited blood flow, which results in subsequent necrosis of the graft. On the other hand, Parkhouse and Evans [13] reported a successful graft of 10×15 mm. In this research, we obtained successful results with a 10×19 mm graft for the columella and a 10×18 mm graft for the ala. The grafts were larger than 10 mm for the majority of the cases, but we were able to obtain successful cosmetic results anyway. Actually, we expect that the original sizes of the grafts were larger than we measured because we measured them after the primary contraction of the graft. Based on our clinical experience, the following factors contributed to our successful results. The first principle for the composite graft procedure to increase the survival rate is proper preparation of the recipient wound bed. We took care to preserve the vascular components, to remove all devitalized tissue, and to increase the contact surface not only of the wound edge but also the wound bed. We carefully used bipolar diathermy with normal saline to minimize the thermal injury of the wound bed vessels and the beveled incisions for the larger contact surface of the recipient bed. Furthermore, we did not use any epinephrine-mixed injections before an incision to prevent constriction of the vessel. From a previous study [3], we found that the subcutaneous layer does not produce a barrier but works as a significant source of vessel communication. So direct vessel-to-vessel anastomosis between the vessels of the subcutaneous fat at the graft and the basal surface of the recipient wound is another important mechanism for the success of composite grafts. The second principle is accurate approximation of the graft to the recipient site without tension. For vessel-to-vessel anastomosis from the wound edge, we took care to put the edges together precisely. The third is absolute immobilization and keeping the moisture balance of the graft. We used Merocele in the nostril for the immobilization of the graft and better shape of the nostril. Antibiotic ointment was used to keep the moisture balance of the graft. We ensured that ointment covered the composite graft all the time so that the graft would not dry. In addition, we did not use any foam dressing or occlusive dressing. The last principle is to find a suitable donor site. It is very important to select as similar tissues as possible for the recipient site. The donor site was not standardized but individualized for each person based on the components, figures of the defect, and different shapes of the ear components. For example, we used the cartilage and skin of the scapha for the columellar reconstruction. Because the patient happened to have a prominent scapha that was more similar to the columella than are those of other people, we were able to attain good cosmetic results and less ear deformity than usual with the primary closure.
Moreover, the average alar width of a Korean is 33.20±3.12 mm and the average columellar length and width are 10.00±2.32 mm and 21.40±2.14 mm, respectively [14]. Koreans have smaller noses than those of Caucasians. Therefore, if the principles of the composite graft procedures are followed carefully and post-surgical care is well provided, a composite graft could be a useful method for the partial or total reconstruction of the ala and columella, particularly for ethnic Koreans and others with similar alar and columellar proportions.
In conclusion, the auricular chondrocutaneous composite graft is a simple and superior method for reconstructing the ala and columella in terms of color, shape, and structural support. If the principles of the procedure are followed carefully, a relatively large alar and columellar defect can be reconstructed successfully with the composite graft without donor site morbidity. The selection of the donor site should be individualized according to the 3-dimensional configuration of the defect.
Notes
This article was presented at the 1st Research and Reconstructive forum on May 12-13, 2011 in Daejon, Korea.
No potential conflict of interest relevant to this article was reported.