Topical EMLA Cream as a Pretreatment for Facial Lacerations
Article information
Abstract
Background
Topical anesthetics, such as eutectic mixture of local anesthetics (EMLA) cream, can be applied to reduce pain before minor procedure. This trial evaluated EMLA as pretreatment for facial lacerations and compared pain, discomfort and overall satisfaction.
Methods
This trial included consecutive emergency department patients ≥16 years of age who presented with simple facial lacerations. At triage, lacerations were allotted to either the routine processing group or EMLA pretreatment group according to date of admission. Initially, the emergency department doctors inspected each laceration, which were dressed with saline-soaked gauze. In the pretreatment group, EMLA cream was applied during wound inspection. The plastic surgeon then completed primary closure following the local injection of an anesthetic. After the procedure, all patients were given a questionnaire assessing pain using the 10-point visual analog scale (VAS) ("no pain" to "worst pain"). All questionnaires were collected by the emergency department nurse before discharge.
Results
Fifty patients were included in the routine processing group, and fifty patients were included in the EMLA pretreatment group. Median age was 39.9 years, 66% were male, and the average laceration was 2.67 cm in length. The EMLA pretreatment group reported lower pain scores in comparison with the routine processing group (2.4 vs. 4.5 on VAS, P<0.05), and lower discomfort scores during the procedure (2.0 vs. 3.3, P=0.60). Overall satisfaction was significantly higher in the EMLA pretreatment group (7.8 vs. 6.1, P<0.05).
Conclusions
Pretreating facial lacerations with EMLA topical cream aids patients by reducing pain and further enhancing overall satisfaction during laceration treatment.
INTRODUCTION
Simple facial lacerations are a common chief complaint among patients who visit the emergency department and require primary closure and wound care. Many of these wounds are traumatic lacerations that are accompanied by pain and discomfort, and additional local anesthesia is needed for primary closure. During triage and inspection by emergency department doctors, patients often seek other forms of relief but must endure pain before wound closure. The most effective way to relieve pain is infiltration with a local anesthetic, but this often causes more pain and phobic reactions to needles. As a result, several methods for reducing the pain associated with local anesthetic injection have been suggested. Recently, several studies proposed topical anesthetics as a substitute for local anesthetic infiltration or as a supplement to local infiltrations [1,2,3,4,5]. Even though topical anesthetics demonstrate several disadvantages, such as delayed onset of anesthesia, most patients who visit the emergency department are not seen by plastic surgeons for ≥60 minutes. In the current study, the mean amount of time between initial presentation at the emergency department and wound closure was 101 minutes. Therefore, adequate time is available for the onset of topical anesthesia while patients wait for plastic surgeons and further laceration management. While many combinations of topical anesthetics have been evaluated, a recent study suggested that EMLA cream may be the most effective topical anesthetic for laceration repair [6]. EMLA cream (5%)-a eutectic mixture of 2.5% lidocaine and 2.5% prilocaine- is a topical dermal anesthetic that can be applied during simple surgical procedures [5,7,8,9,10]. The objective of this study was to evaluate EMLA cream as a topical anesthetic for pretreating lacerations at initial presentation to emergency department doctors, therefore reducing pain and discomfort while patients await further laceration management.
METHODS
Study design
This clinical trial was designed to compare subjective evaluations of pain, discomfort, and overall satisfaction during each step of laceration management. Patients were enrolled in either the routine processing (only lidocaine injection) or EMLA pretreatment groups. EMLA cream was applied by emergency department doctors to healthy patients with simple facial lacerations at initial presentation. Information about EMLA application was not provided to the patients during the study, and the plastic surgeons were also blind to this information.
Patients and setting
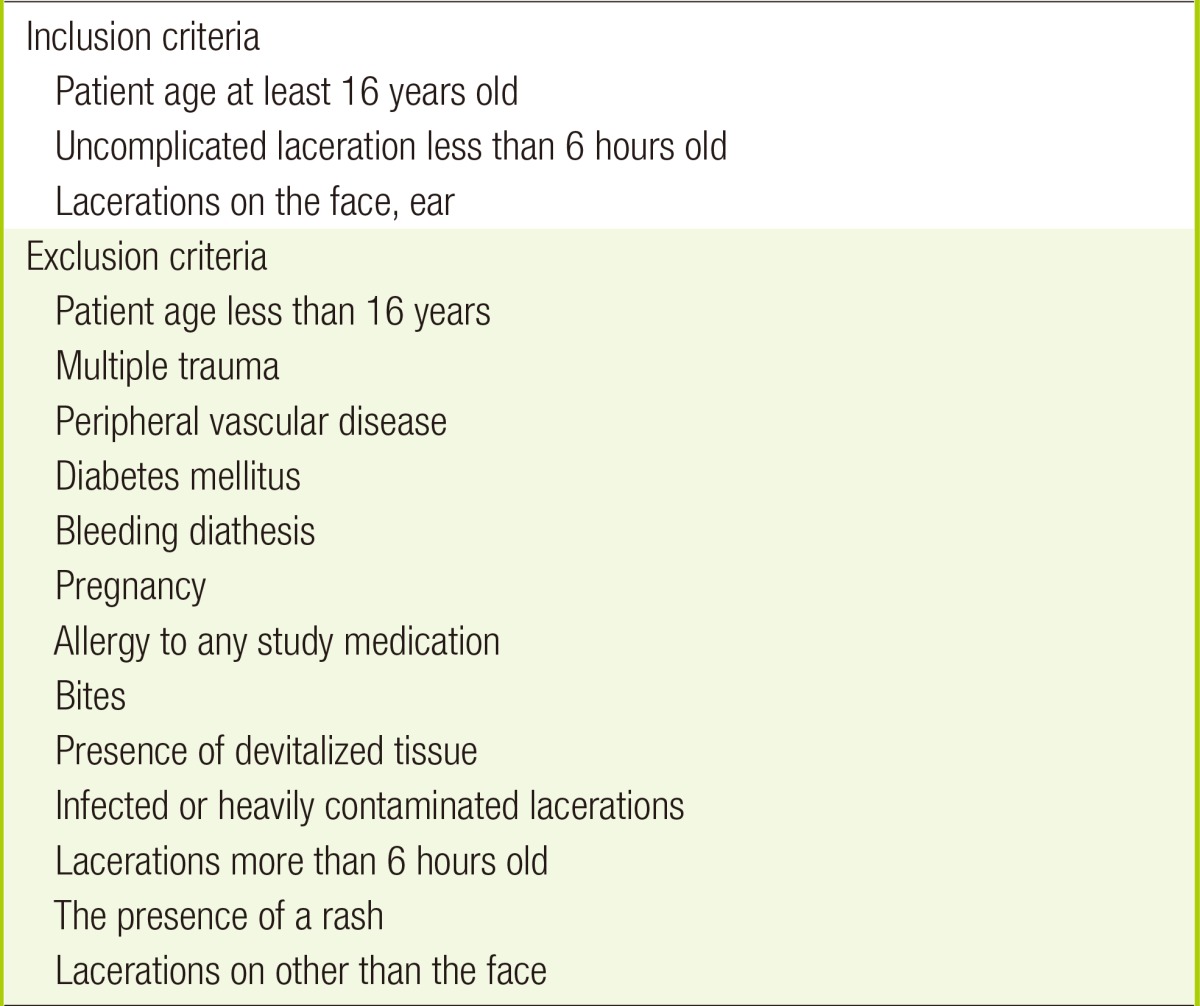
This trial was conducted at the emergency department and patients >16 years of age with simple facial lacerations were enrolled between May to September 2013. Specific inclusion and exclusion criteria are shown in Table 1.
Study protocol
Patients with traumatic lacerations were evaluated by a triage nurse at initial presentation. Patients who met the inclusion criteria were enrolled and allotted to study groups according to the date of admission. Patients treated between May to June 2013 were enrolled in the routine processing group, and patients treated between July to September 2013 were enrolled in the EMLA pretreatment group. Wound irrigation was performed, and saline-soaked gauze dressing was applied with or without EMLA pretreatment. Patients were not informed about the pretreatment procedure. Plastic surgeons who performed primary closure did not evaluate the original wound or receive information about pretreatment procedures, and the same closure procedures were completed in both groups. Questionnaires were given to the patients by the emergency department nurses, and each step in the procedure, discomfort, and overall satisfaction after the procedure were evaluated using the 10-point visual analogue scale (VAS). Patient demographics were compared by retrospective chart review.
Laceration management procedure
At initial wound inspection, emergency department doctors recorded the length, depth, margin status, presence of foreign bodies, and injury mechanisms. A 10-mL syringe with a needle was used to directly irrigate saline using manual pressure. After adequate irrigation, saline-soaked gauze dressing was applied with mild compression. In the EMLA pretreatment group, EMLA cream (eutectic mixture of 2.5% lidocaine and 2.5% prilocaine; Astra USA Inc., Westborough, MA, USA) was directly applied to the wound margins using sterile swabs and then saline-soaked gauze dressing was applied by the emergency department doctors. The amount of EMLA cream was not specified due to individual laceration size, but complete superficial coverage without wound exposure was achieved according to the final state of the wound. At the beginning of primary wound closure, emergency department doctors removed the dressing and cleansed the wound with saline, the plastic surgeon re-inspected the wound, and two wound registries were evaluated by comparing the emergency department and plastic surgery department charts. The edges of the lacerations in all patients were then slowly injected with 1% lidocaine using a 30-gauge needle. Wounds were managed according to standard care protocols, and were mainly sutured using 5-0 PDS for dermal closure (Ethicon Inc., Somerville, NJ, USA) and 6-0 Ethilon sutures for skin closure (Ethicon Inc.). All wounds were evaluated for any signs and symptoms of infection at the initial presentation to the emergency department and follow-up visits until the stitches were removed.
Outcomes
All outcomes were measured via retrospective questionnaire reviews. Pain was evaluated by subjective reporting using 10-point VAS (1 indicating no pain through 10 indicating devastatingly painful). Pain scores were evaluated at each step, including initial inspection at triage, initial wound inspection and irrigation, secondary wound inspection with local infiltration, primary closure, and after the dressings were applied. Discomfort associatied with each item was also evaluated using the same scale (1 indicating no discomfort through 10 indicating extreme discomfort). Overall satisfaction with the emergency department was also assessed (1 as the least satisfied through 10 as the most satisfied). Infection was assessed by taking into account erythema, edema, pain, and heating sense, which was later reassessed at the plastic surgery department clinic at 1 week after primary closure.
Data analysis
Questionnaires were collected, and data were entered into a spreadsheet for further statistical analysis using the Fisher test. For all tests, P<0.05 indicates statistical significance.
RESULTS
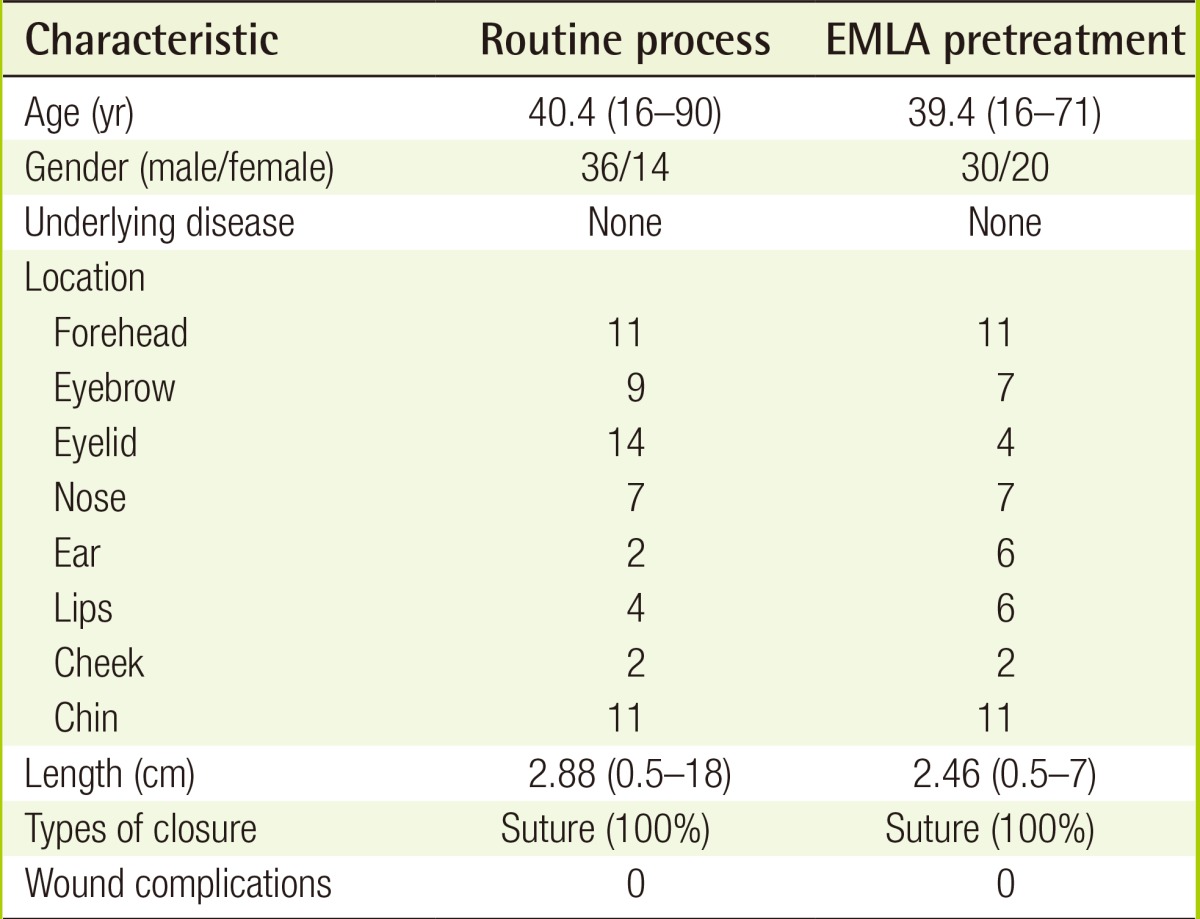
In total, 108 patients were screened and enrolled during the 4-month study period, and 8 patients were excluded because of multiple traumatic injuries, puncture wounds, diabetes, or dog bites (Fig. 1). The median patient age was 39.9 years old (range, 16-90 years), and 34% of patients were female. All wounds were located on the face, and the average length of laceration was 2.67 cm (range, 0.5-17 cm). There were no statistically significant differences in terms of demographics (Table 2). All wounds were anesthetized by the local infiltration of lidocaine before wound closure, and same methods were in both groups to close all wounds.
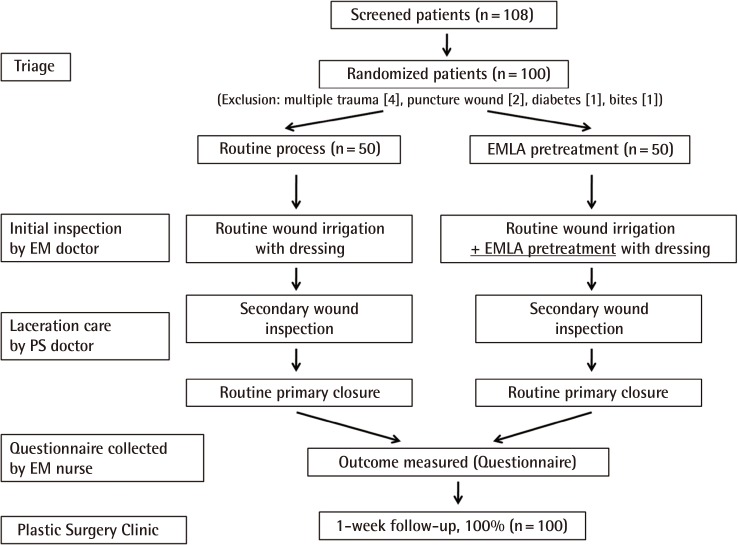
Study design
Designed protocol of enrollment of patients with facial laceration and procedure process. EM, Emergency Medicine; PS, Plastic Surgery; EMLA, eutectic mixture of local anesthetics.
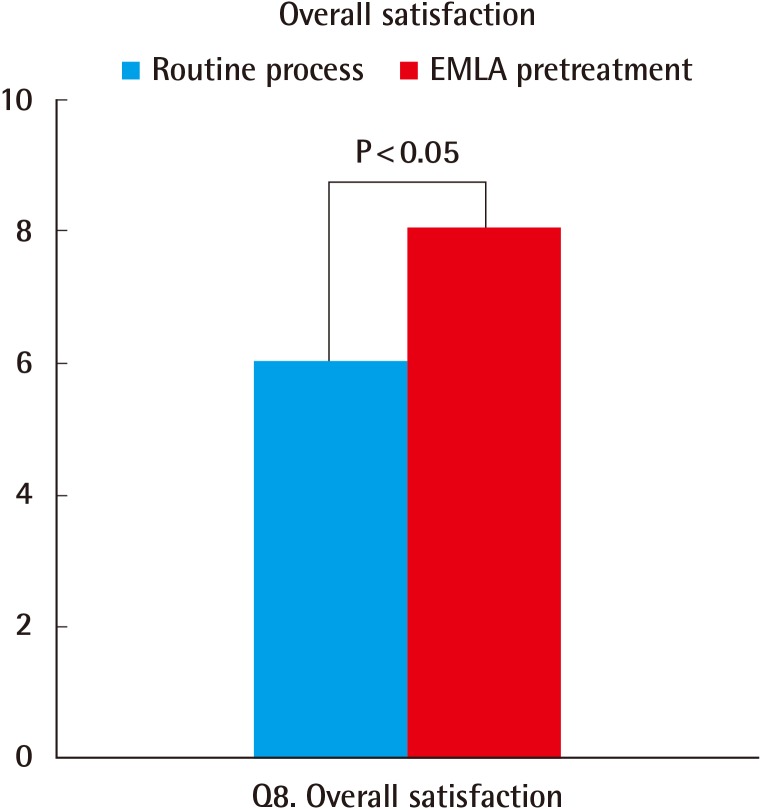
Pain scores at initial presentation demonstrated no significant difference between groups (question 1, 4.24 vs. 4.66; P=0.51) (question 2, 5.0 vs. 5.0; P=0.9) (Fig. 2). Pain scores during primary closure demonstrated a statistical difference between groups, indicating that the pretreated wounds were less painful (questions 3-5; P<0.05) (Fig. 3). Discomfort scales during the procedure demonstrated lower score in pretreatment group, but these differences were not statistically significant (question 6, P=0.70; question 7, P=0.60) (Fig. 3). Patients with pretreated wound reported significantly higher overall satisfaction scores (question 8; P<0.05) (Fig. 4). All patients returned to the plastic surgery clinic for follow-up examinations, and the stitches were removed from wounds. No infected wounds developed in either group.
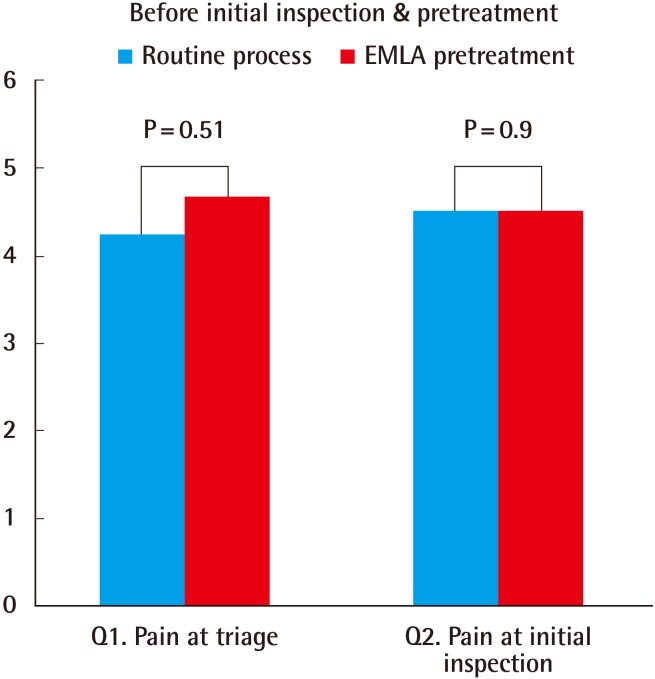
Pain scales before inspection and pretreatment
Question 1 (Q1) evaluated pain at triage according to the 10-point visual scale analogue, and question 2 evaluated pain at inspection by the emergency physician. There were no statistically significance differences between groups (Q1, P=0.51; Q2, P=0.9). EMLA, eutectic mixture of local anesthetics.
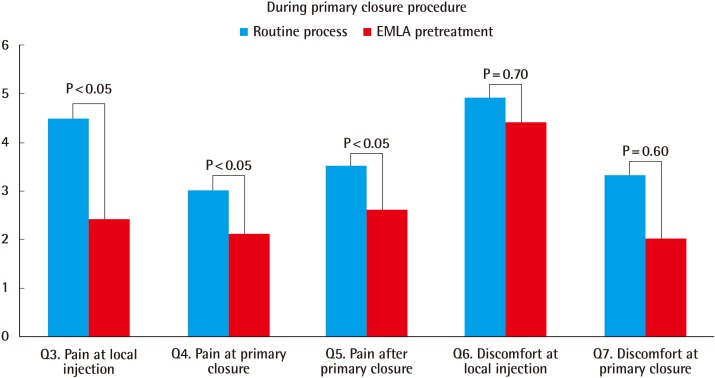
Pain and discomfort scales during the procedure
The EMLA pretreatment group reported lower pain scores than the routine processing group at the local site of lidocaine injection during primary closure and immediately postprocedure (P<0.05). However, differences in discomfort scores between groups were not statistically significant (Q6, P=0.70; Q7, P=0.60). Q, question; EMLA, eutectic mixture of local anesthetics.
DISCUSSION
Previously published studies used topical anesthesia as single anesthetic method, or in conjunction with local injection, to treat lacerated wounds because application results in relatively less pain and avoids unintentional needle stick to the wound itself [2,3,4,7,10,11]. However, topical anesthesia is mainly applied to children due to stronger phobic reactions to needle stick in this population. EMLA cream is a reliable topical anesthesia for a variety of painful cutaneous procedures, such as venipuncture, lumbar puncture, vaccination, and circumcision, and its usage was recently extended for use before facial laser resurfacing [10,11,12]. While EMLA is not approved for use over non-intact skin, Zempsky and Karasic [13] recently compared the anesthetic efficacy of EMLA when suturing 32 uncomplicated extremity lacerations. They found that EMLA is superior to a combination of tetracaine, adrenaline and cocaine when used as an anesthetic for simple lacerations on the extremities following direct application to the lacerated wound itself.
Here, EMLA cream was used to pretreat simple facial lacerations in an adult population. The advantage of pretreating lacerated wounds using topical EMLA cream is pain relief while waiting for the practitioner in the emergency department. Pain relief directly influences subjective pain and discomfort when routine wound closure begins with the local injection of the anesthetic. In the current study, there was a mean of 101 minutes between initial presentation at the emergency department and wound closure, and therefore topical EMLA cream can be applied and its anesthetic effects can be administered. Here, pretreated wounds demonstrated less pain, and patients were more comfortable before and during routine wound care, which eventually led to higher overall satisfaction in comparison with the routine processing group. Still, complete pain loss cannot be achieved using topical anesthesia alone. Therefore, we recommend using topical EMLA cream as a pretreatment in order to supplement the routine injection of local anesthesia. In the current study, no complications were reported 1 week after wound closure in either group. In recent studies of the use of topical anesthetic on lacerations, EMLA cream was reported to be safe to use on open wounds, such as lacerations, in pediatric and adult populations [2,3,4,5,6]. Furthermore, Adam and Mary reported that EMLA is rapidly absorbed when applied to an open wound, and that application of EMLA to an open wound does not cause pain or discomfort [5].
Although the direct puncture of the wound itself is not unavoidable and besides its anesthetic efficacy of EMLA usage, there was significant improvement in overall satisfaction among patients pretreated with EMLA at initial presentation by emergency department doctors (Fig. 4). Furthermore, the extra cost associated with the use of EMLA was minimal; medical expenses did not significantly differ between the two groups (115,300 vs. 118,600 Korean Won; P=0.73). Moreover, the amount of time spent in the emergency department did not significantly differ between the two groups (P=0.85) because EMLA was applied during the initial inspection, which all patients underwent upon entering the emergency department. Topical anesthetics, such as EMLA cream, are useful when pretreating simple facial lacerations by relieving pain and discomfort in patients during the periprocedural period. Conjunctive use aids the routine processing of lacerations and further enhances overall patient satisfaction.
Notes
This clinical trial was preformed according to Clinical Performance Improvement (CPI) guidelines of Asan Medical Center. This study was cooperatively performed by the Plastic Surgery and Emergency Departments.
No potential conflict of interest relevant to this article was reported.