The Role of the Plastic Surgeon in Sentinel Lymph Node Biopsy of Internal Mammary Nodes
Article information
The presence of lymph node metastasis is the single most important prognostic factor in the staging of breast cancer. While the majority of lymphatic drainage of the breast is to the axillary nodes, the most common extra-axillary site of lymph drainage is the internal mammary chain (IMC). The primary method for assessing the tumor status of these nodes is a sentinel lymph node (SLN) biopsy, which allows a surgeon to sample only the primary drainage sites of the tumor rather than performing a complete dissection of the nodal basin. Currently SLN biopsy is routinely used to determine axillary lymph node status in clinically node negative patients with breast cancer, however it is not commonly used to sample IMC SLNs [1]. Although there is much literature arguing for and against routine IMC SLNs, none specifically describe techniques for biopsy of these nodes, particularly when the nodes are more difficult to access. We believe that IMC SLN biopsies can alter the course of treatment and that the plastic surgeon, who has experience working in that difficult-to-navigate region of the thorax, is ideally equipped to perform them.
A 47-year-old woman with a history of stage II (T2N0), estrogen receptor (ER) positive, progesterone receptor (PR) negative, and human epidermal growth factor receptor 2 (HER-2)/neu amplified left breast invasive ductal carcinoma in the lower inner quadrant presented with a new 4.2 cm magnetic resonance imaging-demonstrated mass in the lower outer quadrant. Her first cancer was treated with lumpectomy, axillary SLN biopsy, adjuvant chemotherapy consisting of adriamycin/cyclophosphamide followed by paclitaxel and 1 year of herceptin, and 60.8 Gy of adjuvant radiation therapy. After treatment she remained on tamoxifen. A core biopsy of the new mass showed triple negative invasive ductal carcinoma. She was treated with neoadjuvant chemotherapy consisting of four cycles of gemcitabine and carboplatin with a minimal response.
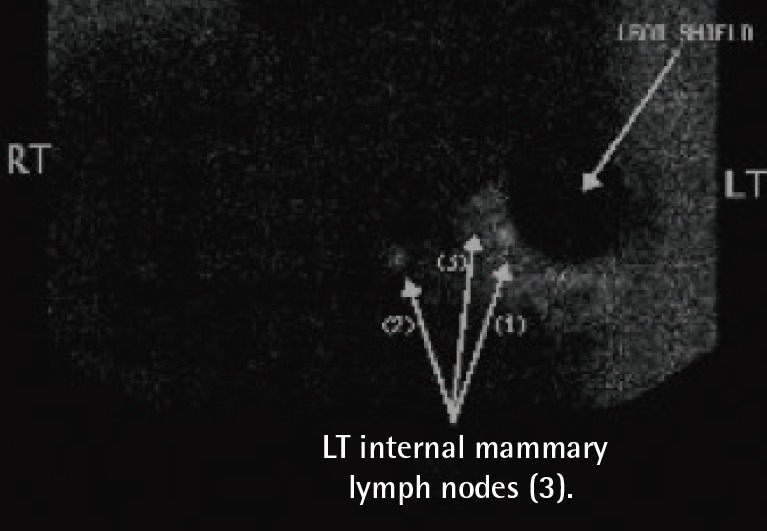
Three weeks before her mastectomy lymphoscintigraphy showed drainage to the internal mammary nodal basin, and biopsy was indicated to determine the need for adjuvant radiation therapy. Plastic surgery was consulted to perform the procedure. One day prior to surgery a dose of 01.05 mCi of 99m-technetium labeled sulfur colloid was given in 4 intradermal injections around the areola. In one hour 3 SLNs were visualized in the IMC (Fig. 1) using a dual head gamma camera (Brightview, Phillips, Andover, MA, USA). The overlying skin was marked.
After induction of general anesthesia, 4 mL of methylene blue dye was injected subcutaneously and into the breast tissue in the retroareolar region, and the breast was massaged for ten minutes to promote drainage. A gamma ray detection probe (Navigator, RMD Instruments, Watertown MA, USA) revealed increased radioactivity in the medial superior left breast, a few centimeters lateral to the sternal border.
Following the raising of skin flaps and resection of the breast tissue medially by the breast surgeon, the plastic surgeon (J.E.P.) performed the biopsy. The internal mammary vessels and adjacent lymph nodes were exposed by splitting the longitudinal fibers of the pectoralis major muscle. The anterior perichondrium of the second costal cartilage was scored and elevated off of the cartilaginous rib, and the rib was incised both laterally and medially using a 10-blade. To protect the underlying pleura, a Doyen was used to separate the posterior perichondrium from the underlying rib, which was then resected. The internal mammary vessels and nodes were exposed by carefully removing the posterior perichondrium.
The gamma probe identified a single SLN. Lymph channels and nearby vessels were ligated using 4-0 silk ties, small clips and bipolar cautery, and the node was excised. There was no evidence of pleural violation. The posterior perichondrium was laid back over the vessels, the split in the pectoralis was repaired, and the breast surgeon completed the mastectomy.
The pathology report showed no involvement of the IMC SLN, staging the tumor as T2N0M0, and the decision was made to forgo additional radiation therapy. There were no perioperative complications. Two months later she underwent prophylactic right mastectomy and bilateral reconstruction.
Debate exists over whether routine IMC SLN biopsy is appropriate. Studies have shown that complete IMC node dissection showed no improvement in survival; however, these studies primarily contained patients with tumors in the lateral quadrants, which are less likely to drain to the IMC, and the studies were underpowered with regards to patients with tumor drainage to the parasternal region [2].
Physicians opposed to routine IMC SLN biopsy argue that the only significant treatment change from identifying a positive IMC node is in adjuvant locoregional radiation therapy, which has not been proven to significantly alter survival and can lead to significant morbidities such as radiation pneumonitis and cardiac compromise [3]. However, in the case of a positive IMC node, loco-regional radiation therapy does increase survival rates [4], and if it is negative, as it was in our patient, the side effects of radiation can be avoided. Additionally several physicians consider a positive IMC node an indication for adjuvant systemic therapy [14].
Studies performed by breast surgeons have reported that they never resect a rib to access IMC nodes due to increased morbidity [15]. Plastic surgeons perform this procedure frequently when preparing recipient vessels during breast reconstruction, and can comfortably perform the same procedure to access the IMC SLN immediately following a mastectomy. In the more difficult case where there is not a mastectomy, the use of the vertical mastopexy incision can allow access to the rib cartilage and the IMC without creating a parasternal incision, which would cause an unsightly scar. For these reasons, a plastic surgeon performs SLNB of IMC nodes at our institution.
This case demonstrates the safety and efficacy of IMC SLN node biopsy when done by the reconstructive plastic surgeon, and how knowledge of IMC nodal status can influence the course of treatment. In a multidisciplinary approach to the treatment of breast cancer, the plastic surgeon is responsible for reconstruction but can also be instrumental in determining staging and treatment. IMC SLN biopsy is an important technique in the evaluation of early breast cancer in select patients, and we believe that the plastic surgeon has the ideal skill set to perform it safely and effectively.
Notes
This study was presented at Midwestern Association of Plastic Surgeons 53rd annual scientific meeting on May 10th, 2014 in Chicago, IL, USA.
No potential conflict of interest relevant to this article was reported.