Foreign-Body Granuloma after Metacarpal Fracture Treatment with Absorbable Implants
Article information
The treatment of unstable fractures or complex injuries of the hand frequently requires the implementation of rigid internal fixation. Traditionally, metallic implants have been used to achieve stability. However, the complication rates of metallic implants are high, with major complications reported in 36% of the patients considered in a series [1]. These complications included nonunion, delayed union, stiffness, plate palpation, infection, and tendon rupture. Therefore, bioabsorbable implants have been introduced to reduce these problems. The first-generation bioabsorbable implants showed a high complication rate due to weak mechanical properties and rapid degradation. This led to the development of stronger devices with improved durability. However, recently developed implants have raised concerns about late-occurring adverse reactions such as foreign body reactions. Herein, a case of foreign body granuloma after the use of an absorbable implant will be presented with a brief literature review.
A 30-year-old male visited Bucheon St. Mary's hospital with a swelling on his left hand after a slip-and-fall injury. He was diagnosed with a left fifth metacarpal bone fracture by hand computed tomography (CT) and X-rays (Fig. 1). The first operation was performed 8 days after the injury, and open reduction was performed. To stabilize the fracture segments, a bioabsorbable plate and screws (Linvatec Biomaterials Ltd., Tampere, Finland) were used for internal fixation. Although the 1-year follow-up was uneventful, the patient visited us with swelling on the previous operation site. Physical exam showed just the swelling of the soft tissue of the operation site without any fluctuation, heat, or erythema. We recommended further evaluation such as an imaging study, but the patient refused to undergo it. Therefore, we decided to observe the patient without administering any medication because there was no evidence of infection. Four months later, the patient visited us again because of another trauma at the same site. Physical examination, CT, and X-rays were conducted, and the patient was diagnosed with a refracture of the fifth metacarpal bone with increased soft tissue swelling as compared to when we first noticed it 4 months previously (Figs. 2, 3). We decided to perform a second operation for the reduction of bone and exploration of soft tissue swelling. Under general anesthesia, an incision was made on the previous operation scar, and a mass was found in the subperiosteal layer. The mass was located just above the screw holes; it measured 2 cm×1 cm and was relatively well demarcated (Fig. 4). We excised the mass and used a metallic plate for rigid fixation. The tissue biopsy for the mass showed foreign body-type multinucleated giant cells suggestive of foreign body granuloma (Fig. 5). A 6-month follow-up from the second operation demonstrated a well-healing surgical incision with no erythema or swelling and no associated signs of infection.

Preoperative X-ray of the first fracture event. The X-ray shows the fracture of the fifth metacarpal bone shaft of the left hand (red circle).

Preoperative X-ray of the second fracture event. The X-ray shows refracture and hole-defects of the fifth metacarpal bone shaft of the left hand (red circle).

Preoperative clinical photo of the second fracture event. Soft tissue swelling can be seen without signs of infection (red circle).
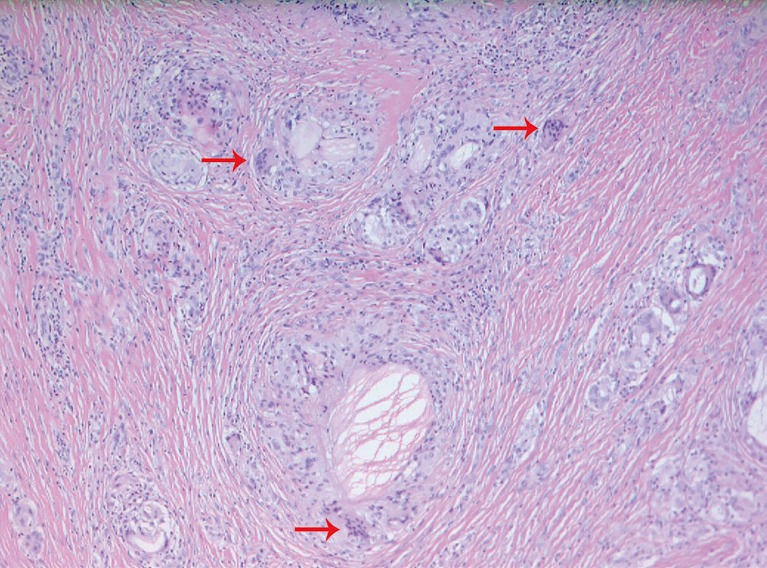
The histologic examination shows multinucleated giant cells (red arrows) suggestive of foreign body granuloma (H&E, ×100).
The use of bioabsorbable implants has increased recently because of their advantages. They may lead to less implant morbidity and subsequent stiffness and do not require hardware removal surgery. Further, they are radiolucent and limit stress shielding, and they incrementally transfer the load to healing fractures.
On the other hand, their disadvantages include poor strength compared with metallic implants [2], rapid loss of initial strength, and relatively high refracture rates [3]. Further, they are prone to inducing foreign body reactions [4]. Moreover, there are few studies on the long-term effects of bioabsorbable implants on the treatment of metacarpal fractures. In one study [5], 4 of 9 patients who were treated with bioabsorbable implants for metacarpal fractures required a second operation because of a foreign body reaction. However, all of them just had fluid accumulation and no foreign body granuloma. This rarity of the foreign body granuloma formation makes our case worthy of report.
In conclusion, although bioabsorbable implants have many advantages, we suggest paying considerable attention to their disadvantages such as their low strength and tendency to cause foreign body reactions. Moreover, hands require the ability to perform a large number of motions and need to have more extensive weight-bearing features than other body sites; therefore, bioabsorbable implants might not be appropriate for use in the treatment of hand fractures.
In conclusion, we suggest that a foreign body granuloma ought to be considered in the differential diagnosis of any mass occurring after the use of bioabsorbable implants in the treatment of metacarpal fractures.
Notes
No potential conflict of interest relevant to this article was reported.
