Treatment of the Mycobacterium chelonae Infection after Fat Injection
Article information
Abstract
For recent years, use of autologous fat injection has increased significantly in facial contouring surgery. Along with such increase in use, complications like atypical mycoplasma infection have been also on the increasing trend. The authors report two cases of Mycobacterium chelonae infection that occurred after autologous fat injection. Patients were treated as infection that resistant to common antibiotics and results were negative to routine culture and Gram staining. Acid-fast bacillus stain, polymerase chain reaction (PCR) test and mycobacterial cultures were conducted for diagnosis under suspicion of atypical mycoplasma infection. Then, combination antibiotics therapy, surgical treatment, and steroid injection were performed for treatment. Both patients were diagnosed with Mycobacterium chelonae in PCR test. They were positive to mycobacterial cultures. Combination antibiotics therapy was repeated to improvement of symptom. However, they could not be free from side effects such as deformation in facial contour, scar and pigmentation even after full recovery. When chronic wound infections after autologous fat injection, we must suspect atypical or mycobacterial infection and conduct examinations for a early diagnosis and proper antibiotic therapy that is effective to the nontuberculous mycobacteria.
INTRODUCTION
Autologous fat injection has long been used for correction of facial, neck and skin contours. For recent years, frequency of minimal invasive surgery such as autologous fat injection has increased significantly for correction of facial and body contours. Rather, the procedure leads to wound infection at the relatively low rate of 1% to 5% [1]. As the number of total procedures that have been performed recently has increased, various side effects have been reported such as acute cerebral infarction, loss of sight and epidermal cyst including redness, swelling, bruise and vasoocclusion, necrosis, hypersensitivity reaction, infection, and foreign body reaction [2,3]. Among these side effects, chronic inflammation and infection and granuloma formation have been also on the increasing trend currently, which has caused many concerns. In the meantime, infection of the nontuberculosis mycobacteria (NTM) as strain that frequently causes chronic inflammation and infection may show the long-term progress and cause complications such as severe scar, notch and hollowing, and irregular facial contour. Against this background, the authors make a report on treatment of NTM infection that is resistant to common treatment and occurs after autologous fat injection based on the results of treatment that was conducted for two patients with NTM infection in this medical center.
CASE
Case 1
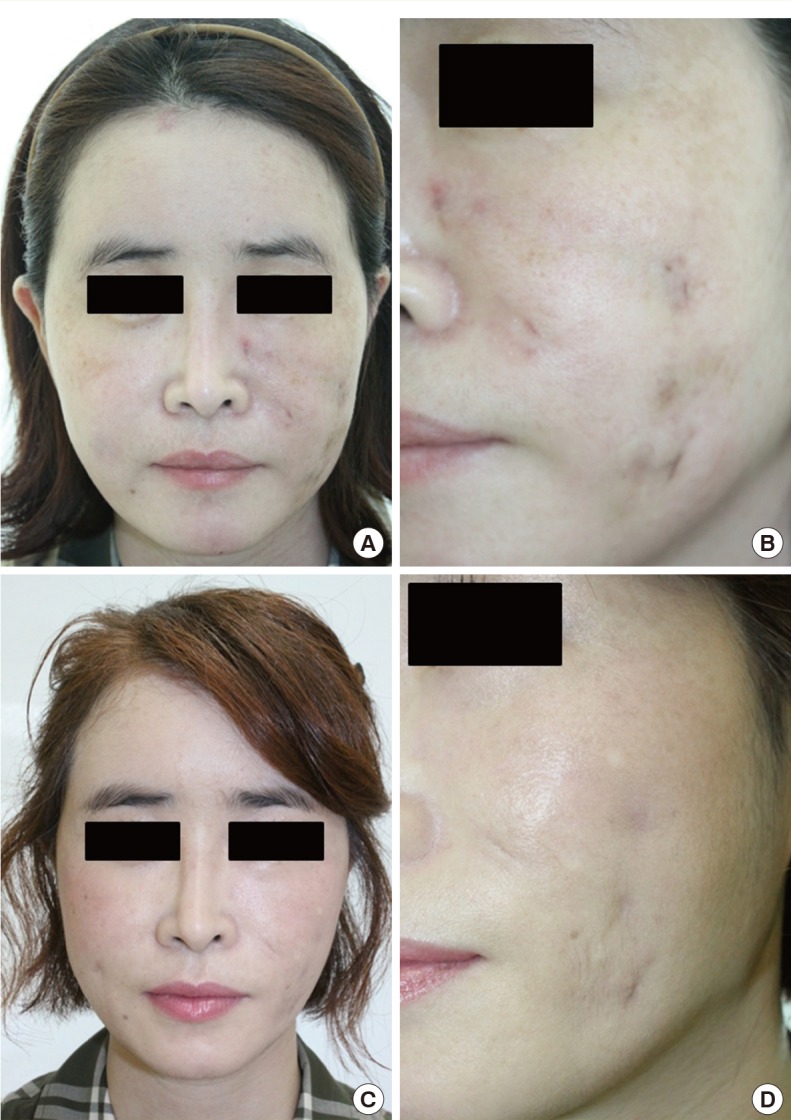
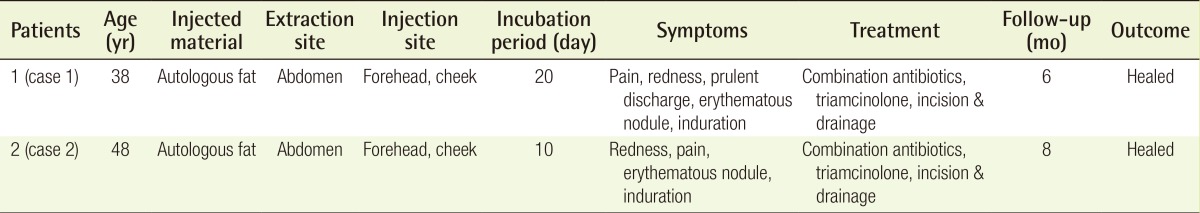
The female patient aged 38 received injection of autologous fat, which was cryopreserved for one month, on forehead and both cheeks in a private hospital. The findings from patient included painful and inflammatory nodule, hardening and abscess formation. The patient received antibiotic treatment and incision and drainage treatment in other hospital but did not have any significant improvement until 3 months after appearance of symptom. First of all, clarithromycin was injected for empirical antibiotic treatment. Gram staining and routine culture were performed repeatedly, which led to the negative results. Since infection of mycobacterium was suspected, acid-fast bacillus (AFB) staining test and real-time polymerase chain reaction (PCR) test were conducted before culture test was conducted for M. tuberculosis and nontuberculous mycobacteria. The results of AFB staining were negative, whereas the NTM was confirmed in real-time PCR test. Multiplex PCR test for bacterium identification was conducted to confirm M. chelona. The patient was hospitalized to receive the combination therapy with use of three antibiotics such as streptomycin (1 g/day), ciprofloxacin (400 mg/12 hr) and cefazedone (1 g/8 hr) for six weeks. The patient also received treatment of incision and drainage of abscess and triamcinolone injection(diluted down to 40 mg/mL) for nodules that sometimes appeared a new. Skin lesions showed improvement within 3 weeks mostly. After being discharged, the patient took clarithromycin (500 mg/12 hr) for 3 weeks in order to prevent recurrence. According to the results of culture examined in 6 weeks, the NTM was confirmed. In the period of monitoring for 6 months afterward, there was no case of complications or recurrence of symptom. However, atrophic hyperpigmented scar and irregular facial contour were observed (Fig. 1).
Case 2
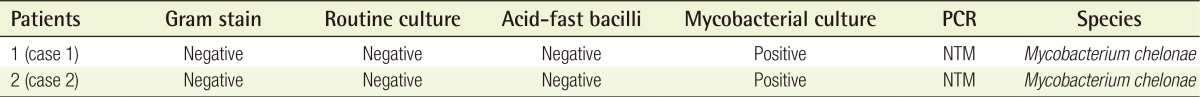
The female patient aged 48 received injection of autologous fat, which was cryopreserved, on forehead (5 mL) and both cheeks (3 mL) in a private hospital. The findings from patient include redness, swelling, erythematous nodule, and hardening in the injection sites. For about a month, the patient took antibiotics and procedures of incision and drainage in other hospital, which proved no significant improvement and it was observed that abscess was spread from cheeks to eyelid. The results were all negative in Gram staining, routine culture and AFB staining test, whereas the M. chelona was confirmed in real-time and multiplex PCR test. Surgical treatments such as drainage and curettage were conducted along with composite medication of amikacin (500 mg/day), cefoxitin (1 g/day) and ciprofloxacin (400 mg/day), which provided good treatment results. After being discharged, the patient took the oral medication of levofloxacin (500 mg/day). However, the patient experienced recurrence of symptoms such as heating sensation, swelling less than two weeks after being charged. The composite medication was administered again, which showed good responses to treatments. The NTM was detected in mycobacterial cultures about four weeks after treatment. After the end of treatment, no recurrence was found in the six-month period of monitoring. However, the patient ended up with having side effects from treatment such as transformation of facial curve, scar and pigmentation (Tables 1, 2, Fig. 2).
DISCUSSION
For supplement or expansion of soft tissues, clinical application of autologous fat injection has increased significantly in the aesthetic aspect. Against this background, infection due to autologous fat injection has been also on the increasing trend gradually. In general, infection that occurs after autologous fat injection is considered as the negative result that is attributable mostly to unhygienic instrument and improper surgical technique [4]. Therefore, it is required to avoid using unsterilized instrument and cleanse surgical instrument properly. In addition, autologous fat injection has the weak point that it is difficult to predict absorption or necrosis of fat, which is why repetitive injection of fat has been performed. For this reason, a new technique that fat is cryopreserved before being used again has been developed and used. However, cryopreserved fat shows the low number of viable cells which leads to the high possibility of fat necrosis or inflammation or infection in graft site [5]. In our cases, two patients' donor site was not infected. That may be because suction canular was not contaminated, but injection canular was contaminated. Also, stored fat may have been contaminated while it was be cryopreserved.
In regard to complications of infection that occurs after cosmetic procedure, a typical causative bacterium is S. aureus [1]. When inflammation appears a new or worsens two weeks after fat injection, it is also necessary to suspect the possibility of infection with atypical mycobacterium, particularly infection with rapid growth mycobacterium (RGM) such as M. chelonae and M. abscessus [1]. Skin infection due to M. chelonae has a variety of types, which ranges from local cellulitis to osteomyelitis. The skin infection caused by the RGMs including M. chelonae is deeply related to skin wound due to penetration procedures such as injection, liposuction, acupuncture, and rarely catheter injection [6].
The RGMs such as M. abscessus, M. fortuitum, and M. chelonae are known to cause infection on soft tissue of skin that is the most common community-acquired infection in the US. When infection is caused by the RGMs, it is generally reported to show symptoms of painful red nodule and folliculitis, swelling, ulcer, and abscess formation [7,8]. It is difficult to make diagnosis owing to such various non-specific clinical symptoms and negative responses to routine culture. This leads to delay in proper treatment, which results in aggravation of symptom. It is difficult to confirm mycobacterium tuberculosis complex or atypical mycobacterium infection in the conventional method such as histopathological examination, AFB test and culture. Microscopic detection of mycobacterium is limited due to low sensitivity. Culture shows the high sensitivity and specificity but takes a long time before results are confirmed. Compared with other diagnostic methods, the PCR test method was reported to show the highest sensitivity and accuracy for diagnosis of mycobacterium infection [9].
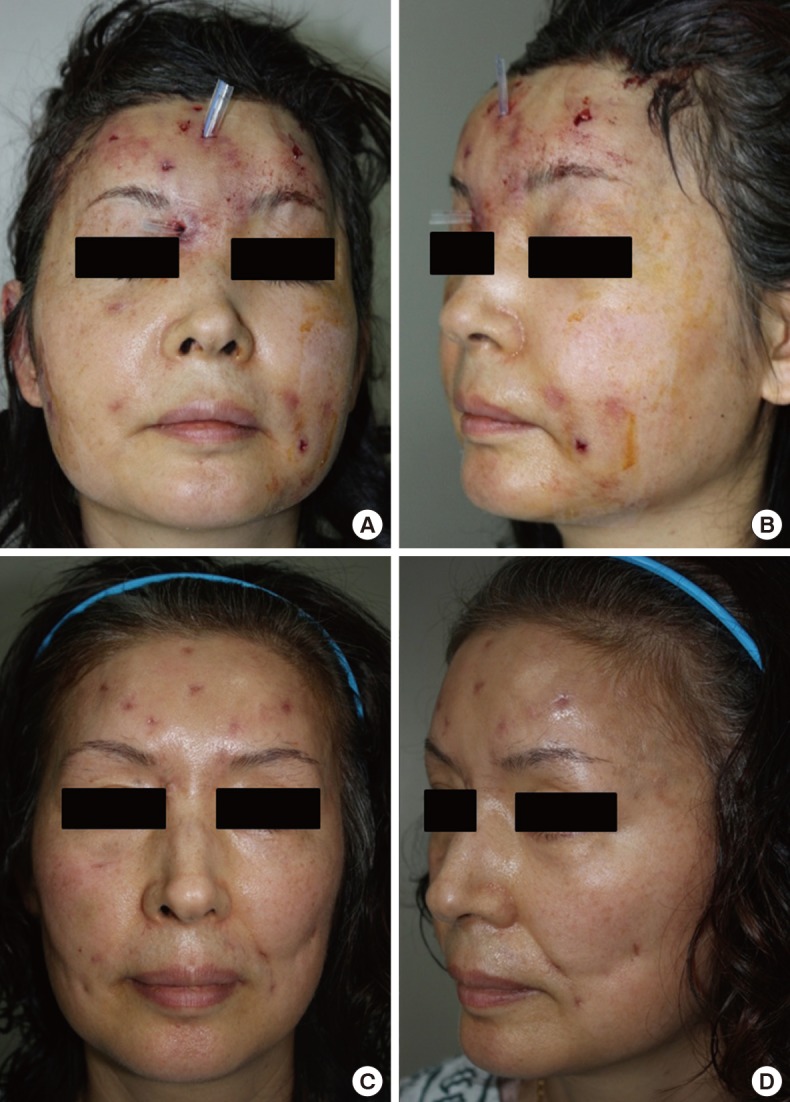
The best treatment method has been still unknown for infection of soft tissue on skin that is attributable to mycobacterium. According to current guidelines, it is recommended to conduct all of the sensitivity tests that can be performed before treatment, in case of treatment failure or after recurrence, to select antibiotic based on the results of sensitivity tests, and to continue using empirical antibiotic until the results of sensitivity tests become available [10]. Antibiotics that were proved to show sensitivity to mycobacterium in in-vitro experiment included chlarithromycin, amikacin, tobramycin, and linezolid. Furthermore, chlarithromycin and azithromycin are oral antibiotic medication that can be used before the results of sensitivity test are available. Even though the optimal period for treatment with use of antibiotic is unknown, it is believed to take at least six months or more for treatment (Fig. 3).
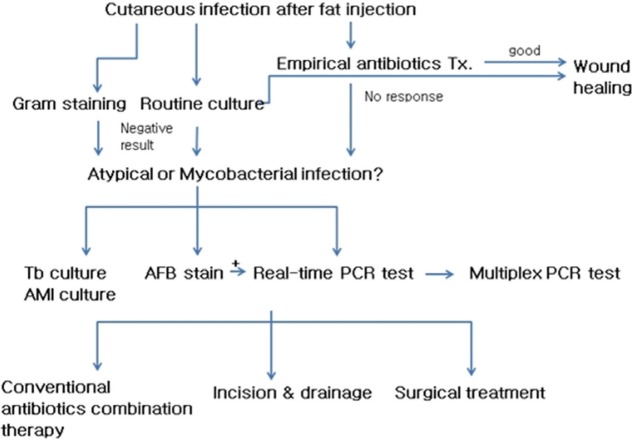
Mycobacterium flow chart
Tx., Therapy; Tb, Tuberculosis; AMI, atypical mycobacterium infection; AFB, acid-fast bacillus; PCR, polymerase chain reaction.
Mycobacterium infection may show the negative response to common Gram staining, routine culture or AFB staining. It is difficult to recognize characteristics of distinct clinical symptoms due to shortage of such characteristics and to conduct treatment. These factors have emerged as problems. Therefore, in regard to treatment of infection that occurs after autologous fat injection, if chronic lesions appear with resistance to common antibiotic treatment, medical staff should suspect atypical infection and mycobacterium infection. Then, they should quickly conduct antibiotic sensitivity test and use empirical antibiotics and simultaneously, perform additional test to diagnose mycobacterium infection. Moreover, proper surgical treatment such as incision and drainage or removal of inflammatory nodule can be helpful to control infection. However, surgical treatment may cause complications such as fistula, scar after incision and asymmetry. As a result, the surgical treatment can be used as the last resort when conservative treatment shows no effect.
Even though the optimal dose or period for injection is not established yet, it is believed that the treatment method by the authors can be properly applied to treatment of mycobacterium infection. In the future, it is required to conduct additional study on proper standard treatment method.
Notes
This study was supported by research funds from Dong-A University.
This study was presented at the 70th Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 2012 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.