Peripheral Osteoma in the Mandibular Angle
Article information
Osteoma is a benign tumor that occurs from the proliferation of cancellous bone, compact bone, or their combination [1]. It can be classified into 3 types, namely, central, peripheral, and extraskeletal osteoma. Central osteoma occurs in the endosteum, peripheral osteoma occurs in the periosteum, and extraskeletal osteoma occurs mostly within muscles [2].
Osteoma mostly begins from the compact iliac bone but can be occasionally observed in the maxillofacial region. In the maxillofacial region, osteoma most frequently invades the sinuses, particularly the frontal sinus. It rarely occurs in the mandible [3].
Various pathogenesis of osteoma have been proposed, including the developmental theory, the neoplastic theory, and the reactive theory [4]. Most cases of osteoma are asymptomatic and do not require surgery, but because patients can be admitted to hospitals due to facial asymmetry, as in the case presented herein, clinicians must understand the clinical aspects and imaging characteristics of osteoma.
A 24-year-old woman with a facial asymmetry due to hypertrophy of the left mandible presented to our department. The patient had first noticed the asymmetrically large left mandible 4 years earlier, but she had observed its progress without clinical evaluation. A mass was coincidentally detected 2 years prior to presentation during orthodontic examination on panoramic radiography, which was the reason she was aware that she had an asymmetrical left mandible. The size of the mass had gradually increased since then, so the patient was admitted to our hospital for removal of the mass and reduction angloplasty for aesthetic purposes.
The patient had a history of contusion on the left mandible from a bicycle accident 12 years prior and explained that she had experienced a hematoma for several weeks at that time. No history of medication was reported, and we could not identify any abnormalities in other organs in our clinical tests.
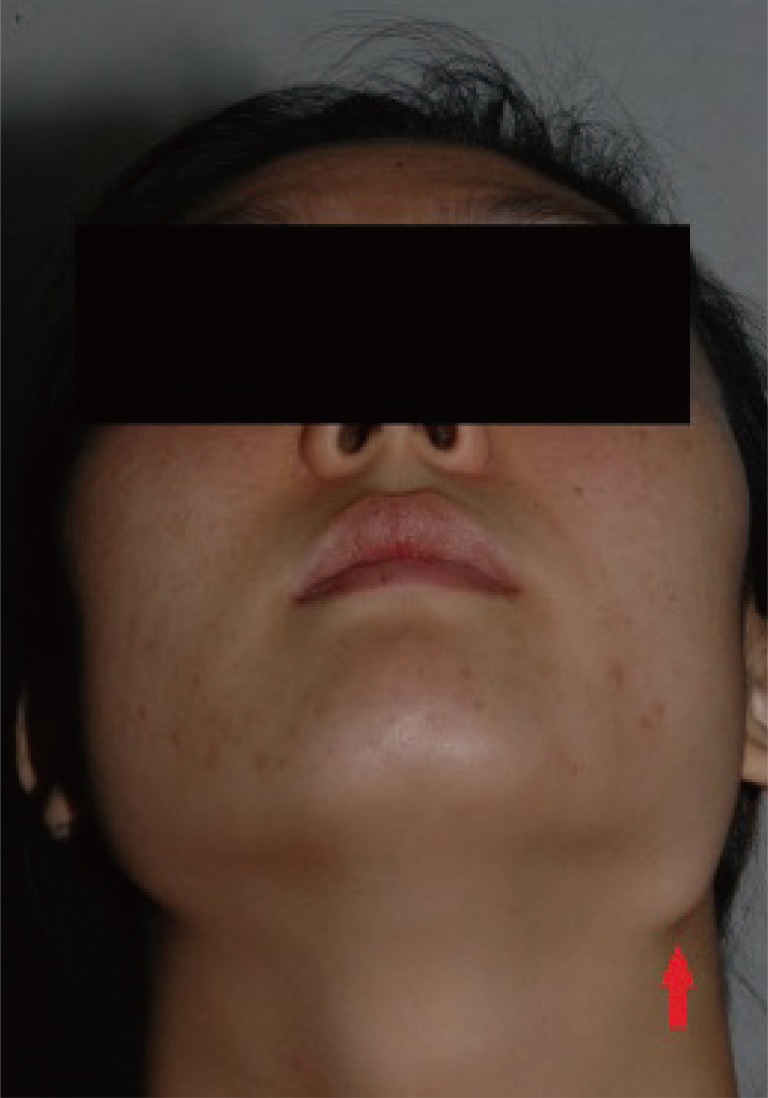
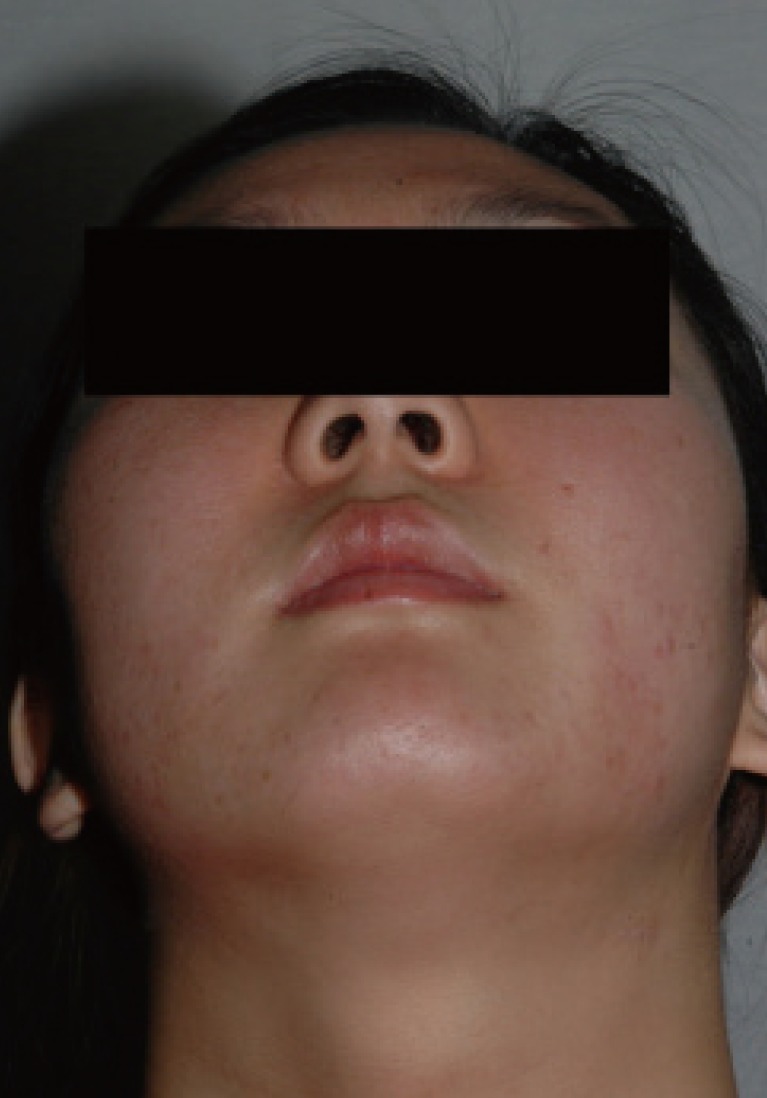
A physical examination showed that the mass was asymptomatic and had a well-defined circular shape, which was firmly fixed on the left mandibular angle region. The skin color around the lesion was normal, and the skin did not adhere to the mass (Fig. 1). As for radiological evaluation, a skull anteroposterior view was obtained, and a solitary oval, well-defined, radiopaque mass was observed (Fig. 2).
Initial panoramic radiograph showing a solitary oval, well-defined, radiopaque mass (white arrow), 13 mm×11 mm in size, abutting with the inferior border of the left angle of the mandible.
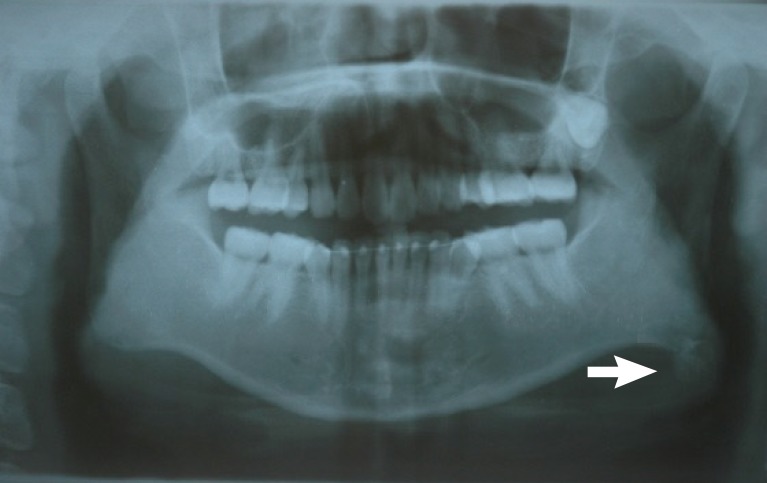
Under general anesthesia reduction angloplasty was performed by performing a resection inside the mouth. Along with the left mandibular angle, the mandibular mass was removed. The mass, which was firmly attached to the mandibular angle, was a white solid lump, 15 mm×10 mm×12 mm in size, with a well-defined boundary (Fig. 3). A biopsy was immediately conducted on the sample. On the postoperative biopsy, an exophytic osteogenic tumor composed of cancellous trabecular bone was observed, and the pathologic diagnosis was osteoma (Fig. 4).

Surgical specimen showing a white mass on the left mandibular angle measuring 15 mm×10 mm×12 mm in size.
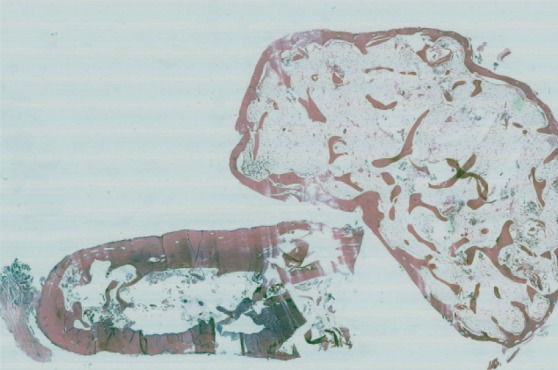
Microscopic features showing an exophytic osteogenic tumor composed of cancellous trabecular bone (H&E, ×4).
The patient wore a compressive garment for 10 days. No specific side effects or complications occurred. In the final follow-up 3 years after the surgery, we observed noticeable improvement of the facial symmetry and no recurrence of the osteoma (Fig. 5).
Peripheral osteoma can occur in the facial region in rare cases. In this region, the mandible is rarely invaded [3]. Instead, in mandibular bone, lesions most frequently develop in the condyle, angle, and margin [4].
Peripheral osteoma can be diagnosed by using conventional imaging tests such as panoramic radiography or computed tomography. On imaging examination, the osteoma appears as a unilateral, pedicled, and well-defined oval or circular mushroom-shaped mass with radio-opacity similar to that of normal bones [12]. Peripheral osteoma has developmental traits such as being asymptomatic, slowly proliferating, and having few prone regions, and thereby being the easiest form to diagnose through clinical characteristics and radiography. However, the definitive evidence for its diagnosis is biopsy findings [4].
Malignant transition of peripheral osteoma has not been reported. In fact, most cases of peripheral osteoma are asymptomatic and often found coincidentally. Hence, surgery is generally not required. However, if it causes facial asymmetry, as in this case, or if it is accompanied by pain or symptoms such as impairment of mouth-opening or swallowing functions, surgical treatment is indicated [5].
The pathogenesis of peripheral osteoma has not been elucidated, but three hypotheses can be proposed according to its cause. First, the developmental theory suggests that peripheral osteomas result from developmental abnormalities, but this is not convincing because most patients have passed their growth phase. Second, the neoplastic theory contradicts the fact that osteoma proliferates extremely slowly. Third, the reactive theory can explain the case of osteoma that occurs after trauma. The subperiosteal hematic extravasation caused by the injury could have facilitated neoplastic degeneration of the injured tissues [4].
We report here a case of osteoma in the mandibular angle. As osteomas can induce clinical symptoms such as facial asymmetry and pain, clinicians must carefully conduct physical examinations during patients' preliminary medical examination. Diagnosis can be made according to the results of preoperative evaluation and appropriate imaging tests, which can be the foundation for surgical planning. Through histological examination, and regular clinical and imaging follow-up after surgery, full recovery can be achieved. We believe that this study can be helpful for clinicians and researchers investigating facial osteoma.
Notes
No potential conflict of interest relevant to this article was reported.