Clinical Experience of Morel-Lavallee Syndrome
Article information
Morel-Lavallee syndrome is closed internal degloving of subcutaneous tissue from the underlying fascia by trauma. It was first described in 1848 by French physician Victor Auguste Francosis Morel-Lavallee [1]. The cavity developed and filled with fluid such as hematoma or liquefied fat etc. It was associated with significant soft tissue injury and frequently occurred on the greater trochanter [2]. Although not common, it can be very severe with infection.
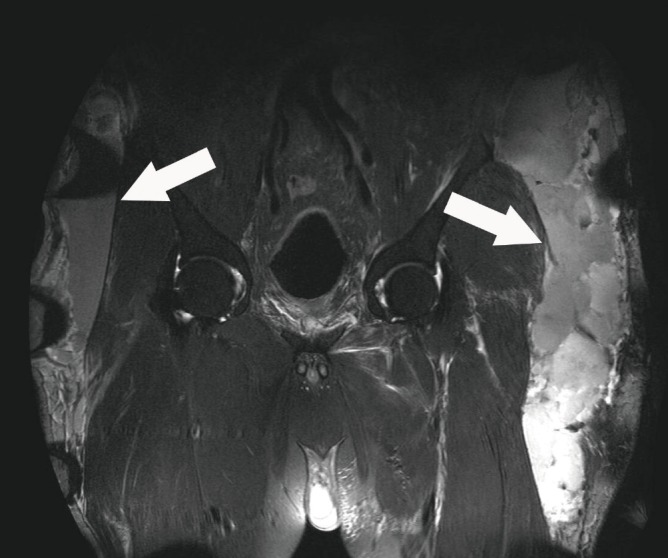
The first case was a 70-year-old man who had suffered a cultivator accident. Approximately two weeks later, swelling was observed on the left lateral thigh with fluctuation. Ultrasonography and magnetic resonance imaging (MRI) (Fig. 1) were performed and fluid collection was found. It subsided with debridement and percutaneous tube drainage (PCD) and compressive dressing. The patient was treated about 45 days. The second case was a 53-year-old man who suffered a pedestrian traffic accident. MR imaging showed a pelvic bone fracture and a huge hematoma on both thighs. (Fig. 2) He was transfer to plastic surgery 4 days later from the accident.
Pseudomonas aeruginosa infection was present on the necrotic tissue and necrosis spread like wildfire throughout the cavity. Massive debridement was performed and skin and soft tissue defects were observed on his lower back, sacral area, both buttocks, and lateral thighs. Surgical dressing was done daily and IV antibiotics were administered. The infection subsided and the defect was covered by split thickness skin graft and a local flap (Fig. 3). He was treated about seven months from the day of the accident. The third case was a 45-year-old man who suffered a fall from a ladder, with fluid collection on both thighs. PCD was attempted on both thighs and the symptoms subsided. However, femoral bursitis remained and was removed by simple excision (Fig. 4).

(A) Skin necrosis after injury. Demarcated large area of necrotic tissue was observed. (B) Local flap and split thickness skin graft. Mild contracture was observed.
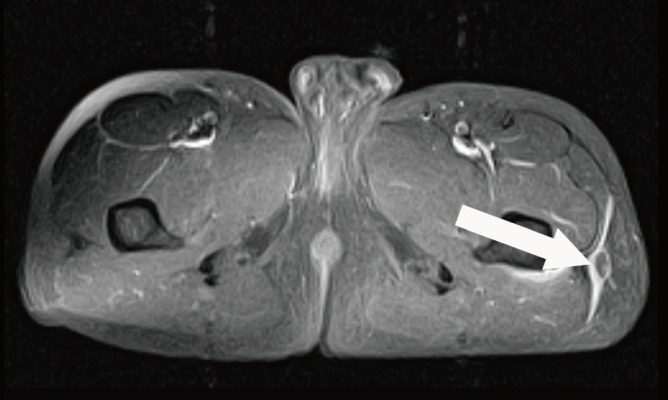
Femoral bursitis (withe arrow). He was treated for Morel Lavallee syndrome with percutaneous drainage with compression. He underwent one more operation for removal of the bursitis.
First and third cases subsided with percutaneous tube drainage and compressive dressing. But the second case, hard to relieve the infection. In this case, Morel-Lavallee syndrome was detected after infection was spread.
We report on three cases of Morel-Lavallee syndrome after severe soft tissue injury. Morel-Lavellee syndrome is uncommon and diagnosis is often delayed. MR imaging is good for assessment of Morel-Lavallee syndrome [3]. Various treatment protocols could be used, such as compressive therapy, sclerosant injection, pulse lavage, and open debridement [4,5]. It could be confuse with recalcitrant bursitis of the knee, soft tissue tumors and lymphocele. Analysis of the protein contents and of the cytology of the liquid is the clue for differential diagnosis with them. We consider that the collected fluid and the cavity increased the severity. Infection is spread through the subcutaneous tissue on the internal cavity, and fluid could be a source of bacterial growth. Therefore, drainage of fluid and removal of the cavity was needed before the infection occurred. For that reason, early detection is important, and knowledge of Morel-Lavallee syndrome and a high index of suspicion are needed.
Notes
This article was presented at the 70th Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 1-3, 2013 in Seoul, Korea.
This article was presented as a poster at the 12th Korea-Japan Congress of Plastic and Reconstructive Surgeons on May 15-17, 2014 in Incheon, Korea.
No potential conflict of interest relevant to this article was reported.