Excision of a Lower Eyelid Inflammatory Pseudotumor Combined with Lower Blepharoplasty
Article information
Inflammatory pseudotumor (IPT)—known as the "great mimicker"—is a rare, benign condition mimicking other benign or malignant tumors. It may be found in almost any organ system. Confirmation of a diagnosis of IPT involves a process of exclusion because IPT mimics other malignant or benign tumors. The mainstay treatment of IPT is corticosteroids. However, in cases of orbital pseudotumor presenting with an eyelid mass, excision of the mass with combined lower or upper blepharoplasty is an aesthetically favorable and appropriate diagnostic option. In the present report, we describe a case of lower eyelid IPT excision combined with lower blepharoplasty. A 57-year-old man presented to our outpatient clinic with mass-like lesions in the right lower eyelid area (Fig. 1). He first noticed the mass 4 months before his outpatient visit. The mass was non-tender and highly movable. Our first clinical impression was that the lesion was an epidermal cyst; however, following ultrasonography, a highly vascularized mass with no definite fluid or abscess pocket formation and nonspecific soft tissue inflammation was detected (Fig. 2). Because the patient also complained of baggy lower eyelids, surgical exploration and excision of the mass in combination with lower blepharoplasty was planned. Through a subciliary approach, two tiny masses were identified in the medial fat pad of the right lower eyelid (Fig. 3). The masses were excised, and biopsy specimens were obtained (Fig. 4A). Openings were made at the orbital septum, and fat was partially removed for the correction of the bulging of the lower eyelid. Lower blepharoplasty was then performed for the opposite side in a similar manner (Fig. 5). The patient was discharged 1 day after surgery. The patient seemed very satisfied with the results, and the stitches were removed on postoperative day 6. Biopsy results showed chronic sclerosing inflammation with fibrosis, plasma cell infiltration, and lymphoid aggregates with multinucleated giant cells and several Immunoglobulin G (IgG)4+ plasma cells (Fig. 4B). Based on these findings, the presence of IPT was suspected, and immunohistochemistry was performed to confirm this diagnosis. Immunohistochemistry confirmed that the mass was an IPT, with no evidence of IgG4-related disease. The patient did not report any complications during the follow-up period.

A 57-year-old man presented to the outpatient center with a palpable mass around the right lower eyelid. Because he complained of baggy lower eyelids, we decided to confirm our diagnosis with an excisional biopsy combined with lower blepharoplasty of both lower eyelids. For the preoperative design, three segments of orbital fat were marked.
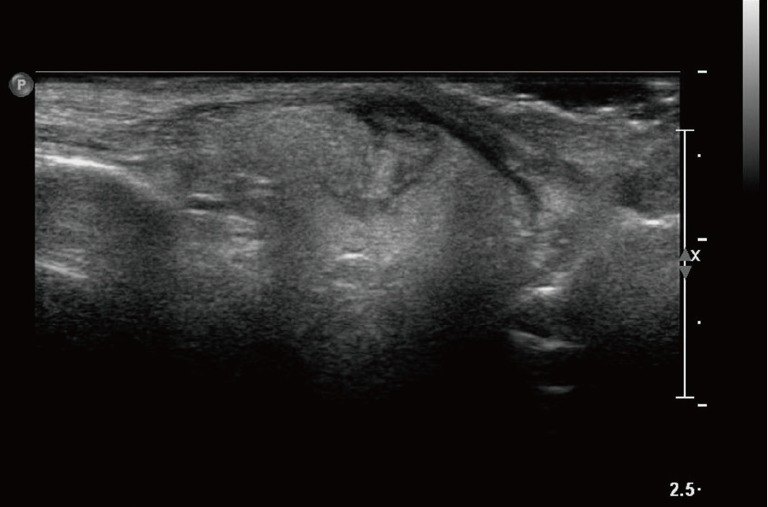
The preoperative ultrasound images revealed a highly vascularized mass with no definite fluid or abscess pocket formation and nonspecific soft tissue inflammation.

Intraoperative image showing two tiny masses in the medial fat pad of the right lower eyelid. Biopsy specimens were obtained to confirm the diagnosis.
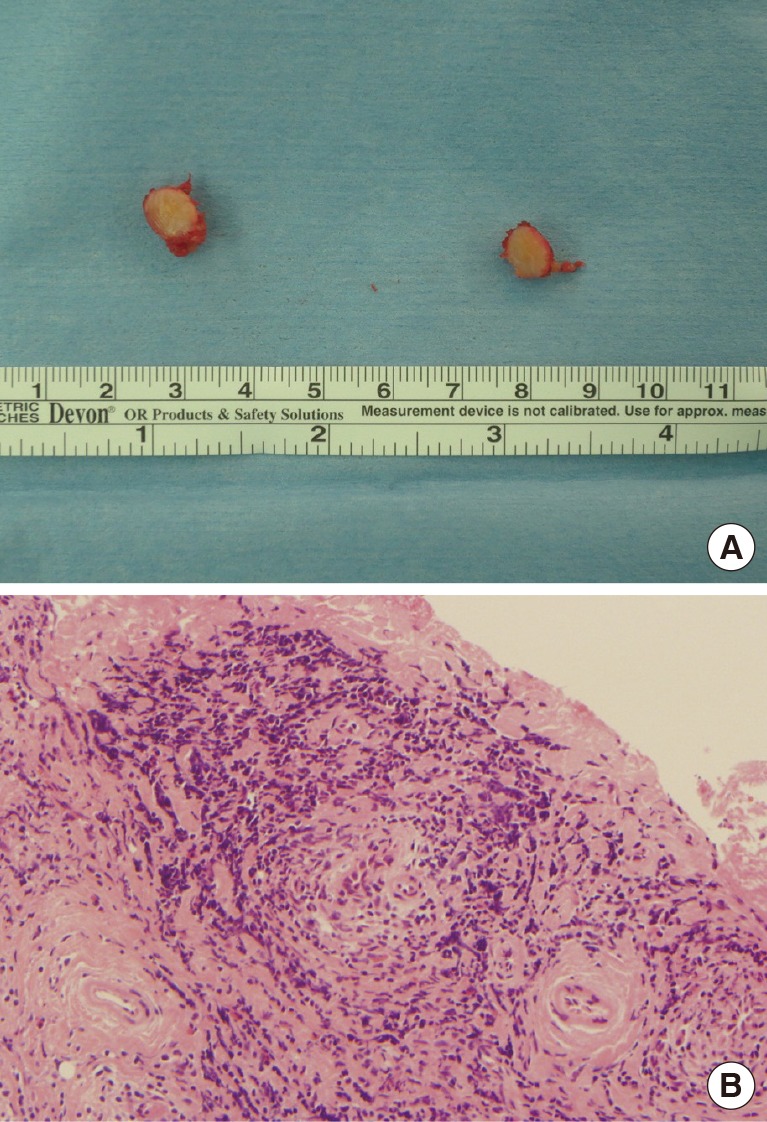
(A) Two tiny masses were excised. The excised masses underwent a pathology examination for analysis. (B) Histopathology showed chronic sclerosing inflammation with fibrosis, plasma cell infiltration, and lymphoid aggregates with multinucleated giant cells and several Immunoglobulin G (IgG)4+ plasma cells (H&E, ×100).
Also known as idiopathic orbital inflammation, IPT is a non-infectious, benign condition that is often misdiagnosed as another benign or malignant tumor or other type of ophthalmopathy. It is the third most common disorder of the orbit following Graves' ophthalmopathy and lymphocytopathy. It accounts for almost 10% of all cases of orbital masses [1]. In 2007, Chirapapaisan et al. [2] reviewed the medical records of 49 patients with orbital pseudotumor (24 males and 25 females; mean age, 43.75 years), most of whom were in their mid-40s or 50s. In terms of chief complaints, 49% presented with proptosis, 22.4% presented with lid swelling or a lid mass, and 12.2% presented with orbital pain; the remaining patients showed diplopia, visual loss, or ptosis [2].
The etiology of IPT is unknown, but many studies suggest a strong relationship between IPT and the immune system. Many rheumatologic disorders are associated with IPT, such as Wegener granulomatosis, giant cell arteritis, and systemic lupus erythematosus. Therefore, many different immunosuppressive therapies can be administered in cases involving IPT. Garrity et al. [3] treated idiopathic orbital inflammation with infliximab, and Hatton et al. [4] successfully treated orbital pseudotumor with mycophenolate mofetil. These findings suggest that orbital IPT is strongly related to autoimmune disease. Many studies indicate that the pathogenesis of IPT involves tissue damage and fibrosis mediated by cytokines and growth factors, which may be associated with various viral infections, a genetic predisposition, or environmental factors [5]. No flowchart exists to diagnose this disease, and the diagnosis of orbital IPT involves a process of exclusion. Other ophthalmopathies, such as Graves' ophthalmopathy, must be excluded before the diagnosis of orbital IPT. Moreover, various rheumatoid disorders should be excluded, because these disorders can present as orbital IPTs. Orbital cellulitis, metastatic carcinomas, dermoid cysts, and epidermal cysts should be excluded on the basis of radiographic characteristics on ultrasonography, computed tomography, or magnetic resonance imaging. Orbital IPTs typically show diffuse infiltration of the orbit or inflammation of the adjacent orbital tissue. Orbital pseudotumors related to orbital masses typically have poorly defined margins. When there is a discrete mass or mass-like lesion, surgical excision with tissue biopsy is an option; however, due to the prompt and marked response to corticosteroids observed in such cases, surgery is not suggested as a first-line treatment. The mainstay of treatment for orbital IPT is corticosteroids. In most cases, patients treated with corticosteroids show a marked improvement in symptoms. A good response to corticosteroid treatment is often viewed as pathognomonic for orbital IPT. In cases of incomplete response to steroids or in patients who cannot receive steroid treatment, radiotherapy can be used as second-line therapy. Many immunosuppressive agents, such as cyclosporin A, methotrexate, azathioprine, and mycophenolate mofetil, are currently being used in clinical practice. Infliximab, a suppressor of tumor necrosis factor (TNF)-alpha, can be indicated in cases of intractable or recurrent orbital IPT. Hence, medical treatment is considered the first-line treatment, and surgical excisional biopsy is not suggested routinely. This is because only approximately 20% of cases of orbital IPT present as an eyelid mass, and medical treatment is very effective in most cases. However, in cases with obvious mass-like lesions, surgical excision and pathology results can be considered for confirmation of diagnosis and treatment. The histopathologic findings of orbital IPT include nonspecific polymorphic, lymphocytic infiltrates with macrophages, polymorphonuclear leukocytes, and eosinophils. Increased connective tissue with fibrosis and edema is also commonly seen. In the case presented here, we could grossly recognize the well-defined mass in the subcutaneous layer, which was not very deep from the skin layer. Therefore, diagnostic excision was one of the best options. Moreover, the patient's needs were considered, and surgical excision with lower blepharoplasty was performed. A diagnosis of orbital IPT was confirmed on the basis of the histopathology results, and during the follow-up period, the patient did not report any complications or recurrence. Both the medical team and the patient were highly satisfied with the surgical results. We present a case of orbital IPT that was excised in combination with lower blepharoplasty. Because most orbital IPTs develop in patients who are in their 40s and 50s, aesthetic surgical procedures for the eyelid can be considered in combination with tumor excision. Therefore, in cases of orbital IPT presenting with an eyelid mass, excision combined with lower or upper blepharoplasty is an aesthetically favorable and appropriate diagnostic option.
Notes
This article was presented as a poster at the 2014 International 72nd Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 7–9, 2014 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.
