Salivary Duct Carcinoma of the Deep Lobe of the Parotid Gland: A Rare Clinical Finding
Article information
Salivary duct carcinoma is a rare malignant tumor that resembles high-grade breast ductal carcinoma. It was first described by Kleinsasser et al. [1] in 1968, and is characterized by aggressive behavior, early metastasis, local recurrence, and a high mortality rate. It most commonly occurs in the parotid gland. Previously reported cases of salivary duct carcinomas involved only the superficial lobe of the parotid gland or both the superficial and deep lobes [2]. This study reports an unusual case of salivary duct carcinoma confined to the deep lobe of the parotid gland.
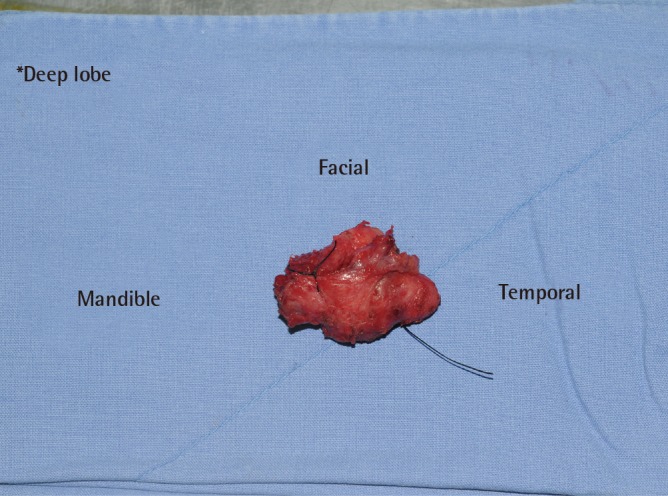
A 59-year-old man presented with a long history of a painless lump on the left preauricular area that had gradually enlarged over the previous year. He denied pain, numbness, and facial weakness. Physical examination showed a well-defined 4×3-cm mass in the left parotid region. The mass was firm, non-compressible, and non-tender on palpation. His left facial nerve function was intact (House-Brackmann grade I). Neither cervical lymphadenopathy nor abnormalities within the oral cavity were found. Fine needle aspiration, which is not diagnostic, was not performed. Computed tomography (CT) (Fig. 1) revealed a 2.5×3.2×4.1-cm, well-enhanced, huge, lobulated, and predominantly solid tumor in the superficial lobe of the left parotid gland. The preoperative laboratory data, including electrocardiography, urinalysis, and a chest radiograph, were unremarkable. A benign tumor, such as pleomorphic adenoma, was strongly suspected, and the patient was therefore taken to the operating room with the intention of performing a left superficial parotidectomy. During the operation, the branches of the facial nerve were preserved via a modified Blair incision. Subsequently, tumor involvement in the deep parotid lobe was identified (Fig. 2). Malignancy was identified in the frozen section of a sample taken from the mass located on the deep lobe. The excision of the superficial part of the parotid gland was completed, the branches of the facial nerve were subsequently elevated, and the deep lobe of the parotid gland was resected. The lesion was classified as cT2NxM0.

Intraoperative photograph showing the mass located on the deep lobe of the parotid gland. The forceps are shown retracting the superficial lobe.
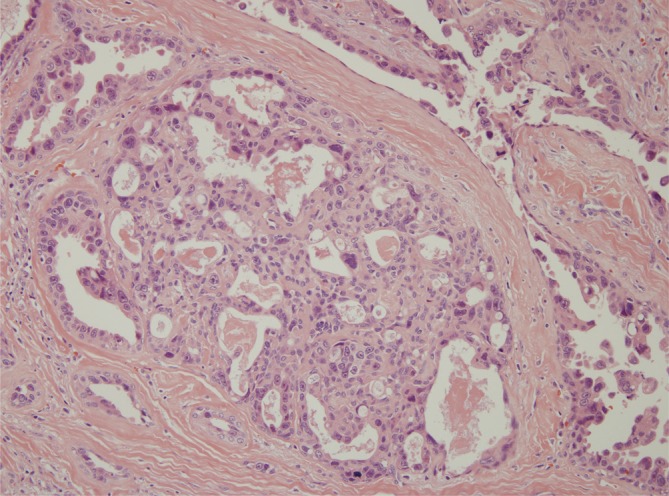
The gross specimen showed a roughly ovoid, nodular, gray-white mass with an irregular border (Fig. 3). The histology report indicated that the tumor was an invasive ductal lesion with cribriform patterns and comedonecrosis (Fig. 4). The resected superfical lobe showed a normal parotid architecture and no tumor. The final diagnosis was salivary duct carcinoma of the deep lobe of the left parotid gland. One of the surgical margins was focally positive for malignancy. No perineural invasion or lymphovascular involvement was found. Control chest CT and positron emission tomography (PET)-CT were negative. Since postoperative CT and magnetic resonance imaging revealed no definitive evidence of perineural spread or metastatic lymphadenopathy, elective neck dissection was not performed. The patient received postoperative chemoradiation therapy with 60 Gy administered in 30 fractions and biweekly cisplatin monotherapy. Following temporary facial nerve paralysis (House-Brackmann grade IV), the patient recovered fully functional left facial movement (House-Brackmann grade I) five months after the operation. He has received regular follow-up for one year with no signs of recurrence or metastasis.
Salivary duct carcinoma represents <1.8% of all major salivary gland tumors. It mainly affects men (73%) in their seventh decade of life. Although it predominantly arises in the parotid gland (72%), the submandibular glands and minor salivary glands may occasionally be involved [2]. It may develop on the basis of pre-existing pleomorphic adenoma in some cases (20%), but generally occurs de novo [3]. Clinically, these tumors are typically characterized by a rapidly growing mass with pain, palpable cervical lymphadenopathy, and facial nerve dysfunction. Fine needle aspiration rarely leads to a diagnosis of salivary duct carcinoma. The finding of tumoral calcifications on CT scans may be suggestive in only 33% of cases. Histologically, these tumors appear as high-grade adenocarcinoma, resembling mammary ductal carcinoma with duct formation. They are solid, with a papillary or cribriform growth pattern and intraductal comedonecrosis. Several histological variants have been described, including mucin-rich, sarcomatoid, and micropapillary types. Perineural invasion has been reported in 60% of cases, and around 30% of cases show lymphovascular invasion [3]. Although total parotidectomy with or without neck dissection and postoperative radiation therapy is the standard treatment, the local recurrence rate is high, associated with both cervical nodal involvement and distant metastasis, and resulting in a poor prognosis. Chemotherapy is generally reserved for metastatic forms [4]. Some recent studies have shown favorable treatment results using trastuzumab-based therapy.
Deep lobe parotid gland tumors are rare, comprising approximately 5% of parotid gland tumors. Approximately 80%–90% of them are benign mixed tumors, such as pleomorphic adenoma, and the others are adenoid cystic, mucoepidermoid, and acinic cell carcinoma, as well as lipoma [5]. Their outward growth displaces the superficial lobe, and they therefore present as a soft preauricular mass. Deep lobe parotid tumors presenting as preauricular masses are often clinically indistinguishable from lesions of the superficial lobe, making it difficult to establish a definitive preoperative diagnosis of a lesion lying deep to the facial nerve.
Based on a literature review, the salivary duct carcinoma presented in this report is unusual, because it arose in the deep lobe of the parotid gland, did not correlate with CT findings, and presented with no symptoms and an absence of perineural and lymphovascular involvement. Therefore, a better prognosis may be expected than is commonly observed in cases of salivary duct carcinoma. This case was reported because of its rarity, and also to add one more case to the existing literature on these tumors.
Notes
No potential conflict of interest relevant to this article was reported.
This article was presented at the Fourth Research and Reconstructive Forum on April 3–4, 2014, in Busan, Korea.