Extra-Abdominal Desmoid Tumor in the Donor Site of an Extended Latissimus Dorsi Flap
Article information
Desmoid tumors are slow-growing fibrous neoplasms, arising from deep musculoaponeurotic structures, and can occur in the abdominal wall, abdominal cavity, or outside the abdomen. Although desmoid tumors are histologically benign and do not metastasize, they are often regarded as semimalignant lesions due to their tendency towards local invasion and repetitive recurrence.
Reports suggest that desmoid tumors represent about 0.03% of tumors and less than 3% of all soft tissue tumors. The incidence of desmoid tumors is known to be about two to four persons per million members of the general population per year [1]. Although desmoid tumors are usually associated with Gardner's syndrome, which is a variant of familial adenomatous polyposis, they can arise sporadically.
The exact etiology of the development of sporadic desmoid tumors is unknown; however, there have been reports of desmoid tumor development following trauma or abdominal surgery, such as appendectomy, laparotomy, laparoscopic surgery, and cesarean section. In most cases, the tumor occurred within 2 years of the operation, but these tumors can appear at any time, even more than 20 years later.
A 51-year-old woman who was previously healthy underwent breast reconstruction with an extended latissimus dorsi flap immediately following a total mastectomy for left breast cancer (Fig. 1). After discharge, she required frequent visits to the outpatient clinic for repeated tapping of refractory seroma and for wound revision because of dehiscence of the back donor site.

Back view of a patient who underwent breast reconstruction with an extended latissimus dorsi flap. Patient complained of a palpable mass with stabbing pain in her donor site.
Two years postoperatively, the patient started to complain of a palpable mass with stabbing pain in her donor site just under the linear scar. We removed the capsule under the donor site scar and collected the fluid inside the capsule. The histology revealed chronic inflammation with dense fibrosis. Unfortunately, the excision site needed an additional surgical procedure due to wound infection.
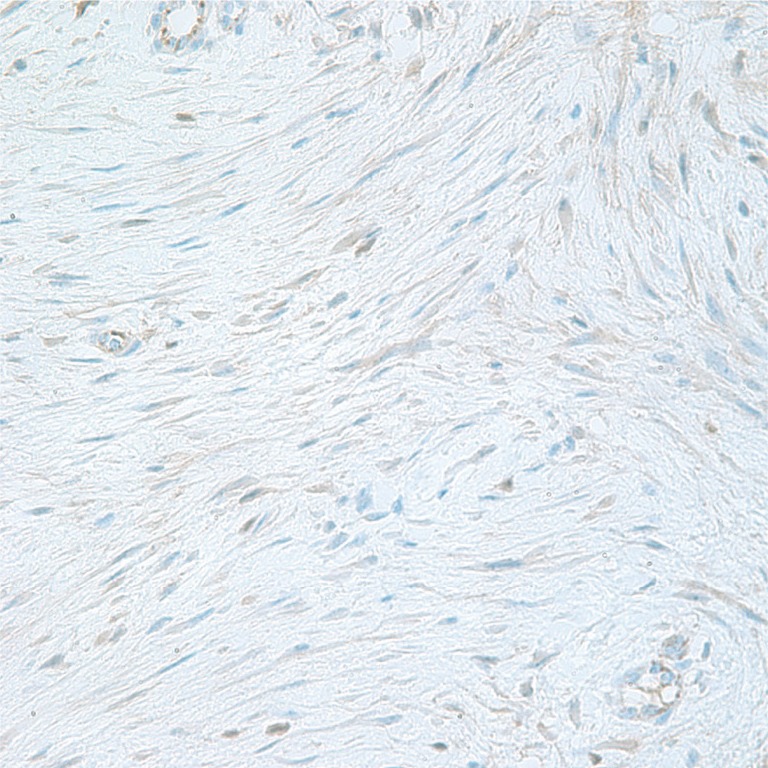
As there had been no improvement in the pain with the first excision of the mass, 8 months after the last operation date, we decided to explore the donor site. We found a white mass measuring 4 cm×5 cm in the subcutaneous layer under the incision site. The tumor was composed of a fibrotic component and associated with a small fluid collection in the patient's back (Fig. 2). After removal of the mass, we found no remnant mass on gross examination. Hematoxylin and eosin staining revealed an extra-abdominal desmoid tumor. Immunohistochemical nuclear staining with beta-catenin was positive; this finding is seen in about 85% of sporadic desmoids following mutation of the CTNNB1 gene encoding beta-catenin (Fig. 3).
After the operation, the patient had partial return of the pain. Follow-up magnetic resonance image at 12 months post-surgery revealed no sign of recurrence (Fig. 4).
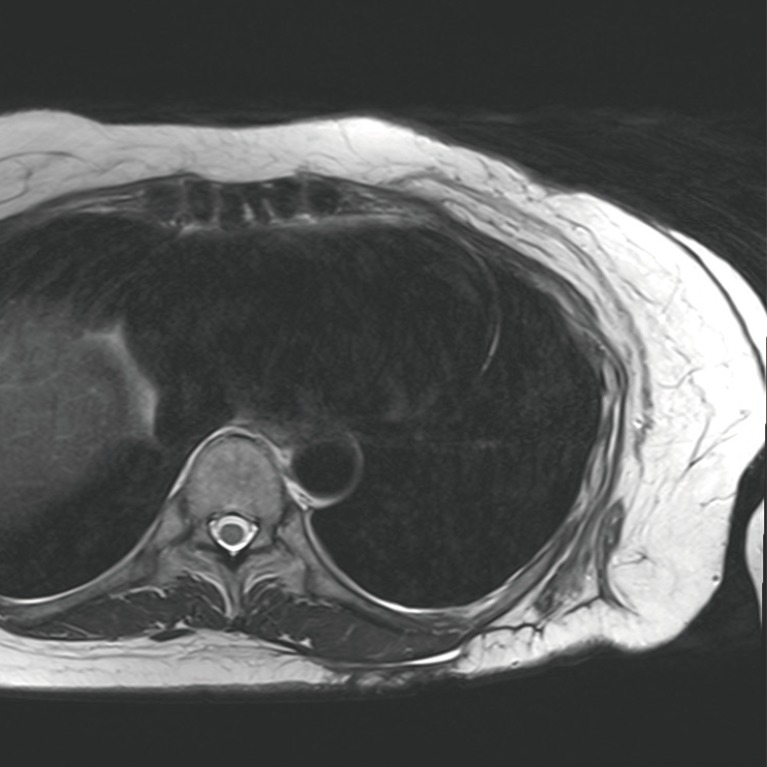
Axial magnetic resonance imaging (T2-weighted image) at 12 months post-surgery. There is no sign of recurrence.
The course of development of desmoid tumors is unpredictable, and symptoms vary from patient to patient. Some patients suffer from aggressive progression and recurrence, whereas others exhibit no symptoms.
A wide excision with clear margins has long been accepted as the first-line treatment modality. Although a free resection margin is associated with a low rate of recurrence, there remains controversy about the amount of tissue that needs to be resected. Furthermore, the complications of wide tumor resection sometimes outweigh the advantages, as it may result in permanent functional sequelae.
Nakayama et al. [2] reviewed clinical outcomes and changes in tumor size in 11 consecutive patients with extremity and trunk desmoid tumors, and suggested that simple observation is a non-invasive and function-preserving treatment.
Radiation therapy has been shown to be an effective method to control primary or recurrent lesions in some reports. Cytotoxic chemotherapy has been used in progressive, recurrent, or unresectable tumors. However, the benefit of radiation therapy and chemotherapy remains controversial, due to the risk of complications and the fact that only a small number of patients have been treated by either method so far. The effects of various types of therapy, involving anti-estrogen or non-steroidal anti-inflammatory drugs have also been reported [3].
Treatment strategies can vary from observation to surgery and adjuvant therapy. Given the potential morbidity associated with some of the strategies, the decision should be tailored to the individual and discussed with the patient.
Kovacs et al. [4] reported a case of desmoid tumors arising at the latissimus dorsi flap donor site. The patients underwent abdominal resection and reconstruction with a latissimus dorsi free flap for intra-abdominal desmoid tumors. However, the patients had Gardner's syndrome, which is known to be a risk factor of desmoid tumors. They consider this to have been triggered by operative trauma; however, the possibility of iatrogenic metastasis from the abdomen could not be excluded. Paradol et al. [5] also reported a desmoid tumor occurring in a scar at the donor site of a latissimus dorsi flap for breast reconstruction following total mastectomy. In this case, the patient had no history of fibromatosis or polyposis such as Gardner's syndrome. One month after the excisional biopsy revealed the desmoid tumor, wide excision with a 5-cm safety margin, and reconstruction with a local advancement flap were performed to prevent recurrence [5].
In our case, we could not confirm the presence of a negative margin during the operation. However, because there was no evidence of recurrence during the 1-year follow-up period, we decided to adopt a wait-and-watch approach with regular follow-up examinations every 6 months rather than performing prophylactic wide excision, which might lead to cosmetic dissatisfaction or functional sequelae.
It is not easy to diagnose a desmoid tumor because this type of tumor may arise in any location in the body and resemble a capsule or scar tissue in a post-operative site. Therefore, we recommend that clinicians perform a biopsy for early detection in cases where desmoid tumors are suspected, and consider an individualized approach when discussing treatment modalities.
Notes
No potential conflict of interest relevant to this article was reported.