Outcomes of Surgical Treatment of Vascular Anomalies on the Vermilion
Article information
Abstract
Background
The vermilion plays an important role in both the aesthetic and functional aspects of facial anatomy. Due to its structural features, the complete excision of vascular anomalies on the vermilion is challenging, making it difficult to determine the appropriate treatment strategy. Thus, the authors analyzed the results of surgical treatment of vascular anomalies on the vermilion.
Methods
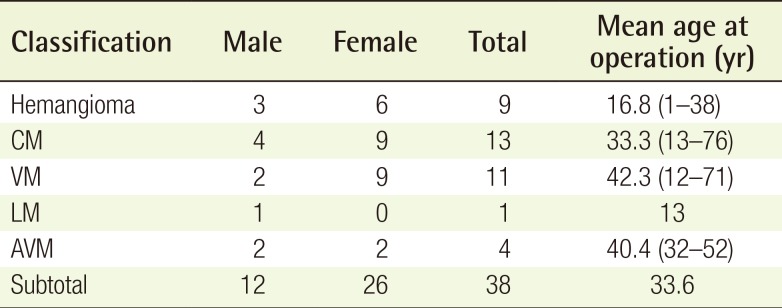
The medical records of 38 patients with vascular anomalies on the vermilion who underwent surgery from 1995 to 2013 were analyzed. Nine of the cases had an involuted hemangioma, and 29 cases had a vascular malformation; of the vascular malformations, 13, 11, one, and four cases involved were capillary malformations (CMs), venous malformations (VMs), lymphatic malformations (LMs), and arteriovenous malformations (AVMs), respectively. We investigated the surgical methods used to treat these patients, the quantity of surgical procedures, complications and instances of recurrence, and self-assessed satisfaction scores.
Results
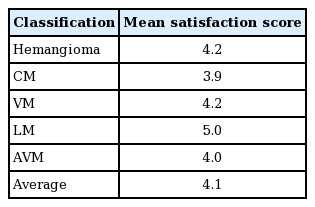
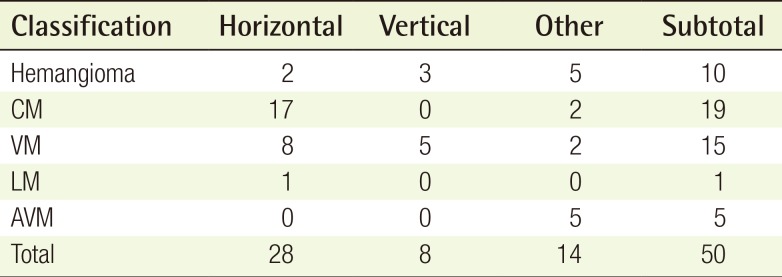
A total of 50 operations were carried out: 28 horizontal partial excisions, eight vertical partial excisions, and 14 operations using other surgical methods. All cases of AVM underwent complete excision. Six cases experienced minor complications and one case of recurrence was observed. The overall average satisfaction score was 4.1 out of 5, while the satisfaction scores associated with each lesion type were 4.2 for hemangiomas, 3.9 for CMs, 4.2 for VMs, 5.0 for LMs, and 4.0 for AVMs.
Conclusions
It is difficult to completely excise vascular anomalies that involve the vermilion. This study suggests that partial excision focused on correcting the overall contour of the lips is effective and leads to satisfactory results.
INTRODUCTION
Although hemangiomas and vascular malformations are two separate types of vascular anomalies with distinct clinical symptoms and progress, confusion has existed in their naming and classification. The first steps in their classification were taken by Mülliken and Glowacki [1], followed by the classification by Jackson et al. [2]. The classification of the International Society for the Study of Vascular Anomalies is now generally accepted [3]. Although hemangiomas and vascular malformations invade a variety of body parts, the vermilion is notable because it plays a crucial role in pronunciation and food ingestion. The physical aspects of its structure are also unique, most notably its three-dimensional structure and free margin.
Tumors occurring in the vermilion, and especially vascular anomalies, cause patients significant discomfort and often result in serious deformities that may require surgical treatment. Due to its unique structural features and the characteristics of most vascular anomalies, reports on the outcomes of the surgical treatment of such lesions are rare, making it difficult to establish clinical treatment plans for patients with such tumors. Therefore, the authors performed surgical treatment in patients with vascular anomalies occurring on the vermilion and investigated the types of operations that were performed, as well as the results, prognosis, and complications.
METHODS
Subjects
In this study, the medical records of 38 patients with vascular anomalies who underwent surgery from 1995 to 2013 were analyzed in a follow-up study. All operations were performed by a single surgeon in a single center. The average follow-up period was approximately 16 months, with a range of follow-up duration extending from three months to 10 years.
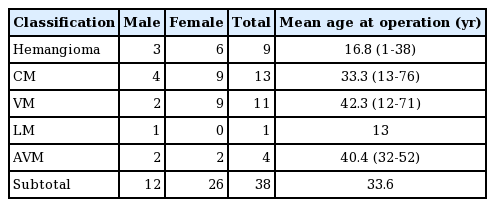
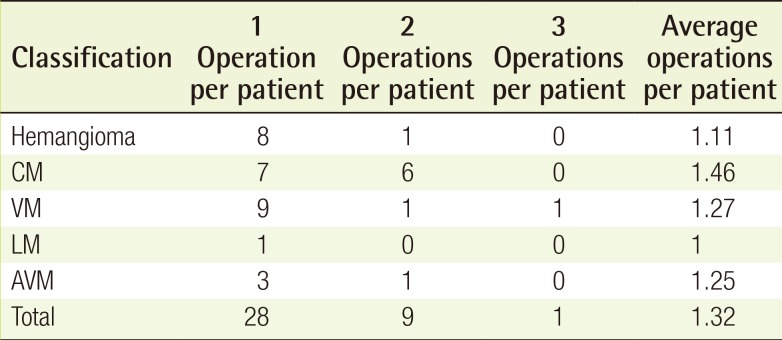
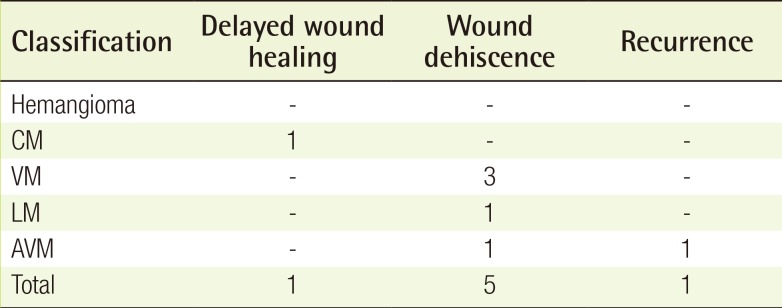
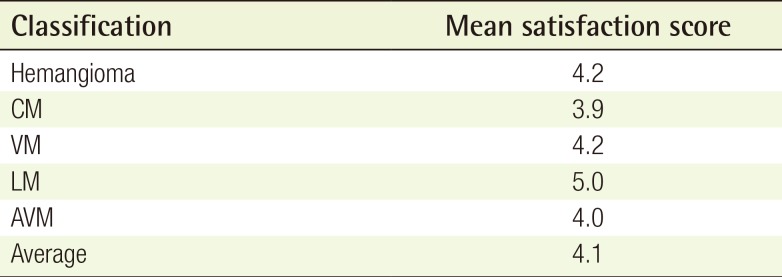
Nine cases had an involuted hemangioma and 29 cases had a vascular malformation. The cases of vascular malformation included 13 cases of capillary malformation, 11 cases of venous malformation, four cases of arteriovenous (AV) malformation, and one case of lymphatic malformation. The patients ranged from one to 76 years of age, and the mean age at the time of surgery was 33.6 years (Table 1).
Methods
Based on a retrospective review of the patients' medical records, we recorded the surgical techniques, number of operations, complications, recurrence, and the satisfaction of patients after surgery.
Surgical techniques
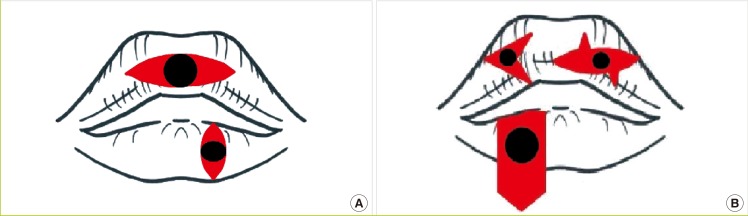
Complete resection of the lesion is ideal. However, complete excision was often difficult to perform due to the structural features of the vermilion and the characteristics of the lesion. Thus, the goal of each operation was to correct the overall contour of the lips. The surgical procedures were classified as follows: horizontal elliptical excisions; vertical elliptical excision; and others, including wedge-shaped and star-shaped excisions (Fig. 1).
Number of operations
The number of operations was determined, in light of the fact that some staged excisions were performed due to the location and size of the lesions, as well as the possibility of reoperation due to recurrence.
Complications and recurrence
Instances of complications and recurrence after surgery were investigated by assessing the medical records of patients and questionnaires filled out by the patients.
Satisfaction evaluation
Patients were asked to evaluate their level of satisfaction when visiting the hospital for follow-up or by telephone. The patients rated their overall satisfaction regarding their overall appearance, symptoms, function/daily activities, and quality of life. They were asked to evaluate the results of the surgery and their satisfaction using a scale in which scores of 1, 2, 3, 4, and 5 indicated poor, fair, average, good, and excellent levels of satisfaction, respectively. The survey was performed at least six months after treatment. The average postoperative follow-up period was 55 months, ranging from six months to 10 years. Patients who underwent more than one operation were asked to answer the questionnaire based on their experience after all procedures were completed.
RESULTS
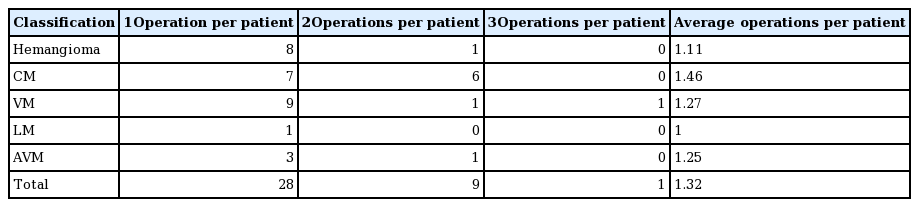
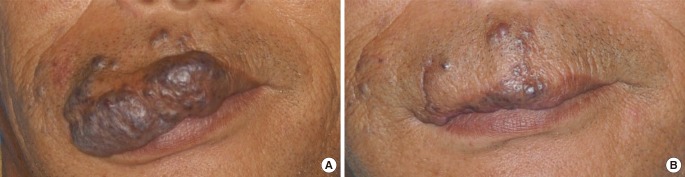
A total of 50 operations were performed on 38 patients. Among the hemangioma cases, two operations were horizontal partial excisions, three were vertical partial excisions, and five were excisions with another design. Among the cases of capillary malformation, 17 operations were horizontal partial excisions and two cases involved excisions with another design. The cases of venous malformation included eight horizontal partial excisions, five vertical partial excisions, and two excisions with another design. Horizontal partial excision was carried out in the one case of lymphatic malformation. In cases of AV malformations, a different surgical procedure was performed. In this procedure, the blood vessel related to the nidus that entered and exited the malformation was identified, and exfoliation was performed as distantly from the lesion as possible, the blood vessel was then ligated, and the lesion was removed (Table 2, Fig. 2).
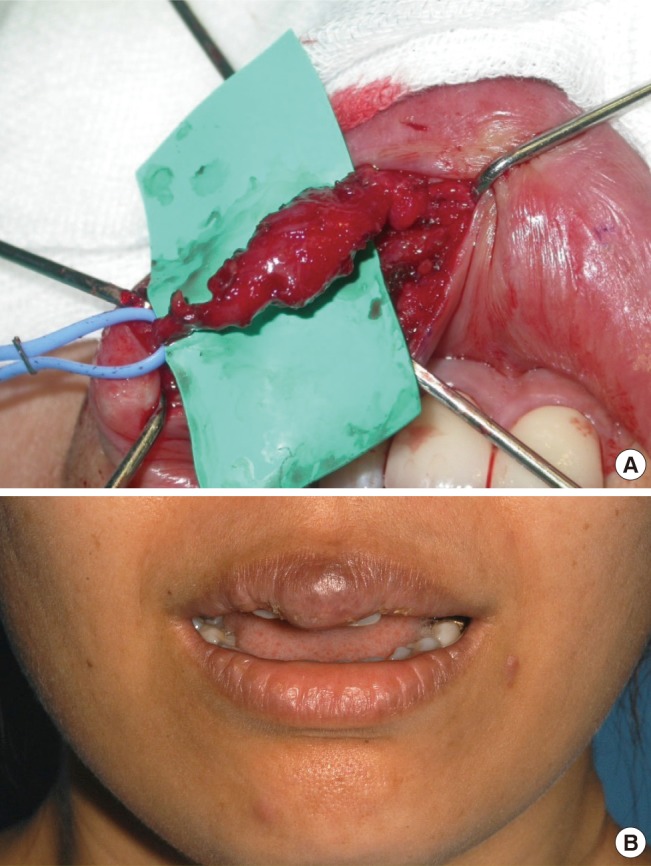
Surgical procedures in the excision of AV malformations
A patient with an AV malformation. (A) An intraoperative image. (B) A preoperative image. (C) A postoperative image taken 14 months after excision. AV, arteriovenous.
Of the 38 patients, 28 underwent surgery once, nine patients underwent surgery twice, and one patient underwent surgery three times. Among the patients who underwent surgery twice or more, one case involved reoperation due to recurrence of the lesion, while the other cases involved staged excision due to the size and locations of the lesions (Table 3).
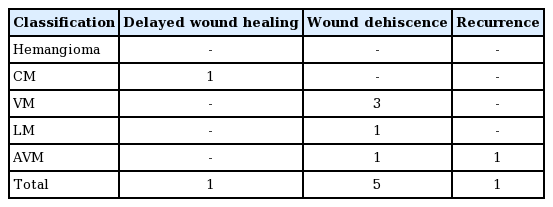
In five cases, dehiscence occurred in the operation site, requiring resuturing, and wound recovery was delayed in one case, in which the patient required approximately one month to recover. In one case of AV malformation, the lesion recurred (Table 4).
Of the 38 patients, 24 (approximately 64%) responded to the satisfaction survey. Overall, patients reported a satisfaction score of 4.1 out of 5 points, reflecting an evaluation of their satisfaction as between good and excellent. When the scores were broken down according to the type of lesion, a score of 4.2 was reported by patients with a hemangioma, 3.9 by patients with a capillary malformation, 4.2 by patients with a venous malformation, 5 by patients with a lymphatic malformation, and 4.0 by patients with an AV malformation (Table 5, Figs. 3, 4, 5, 6, 7).
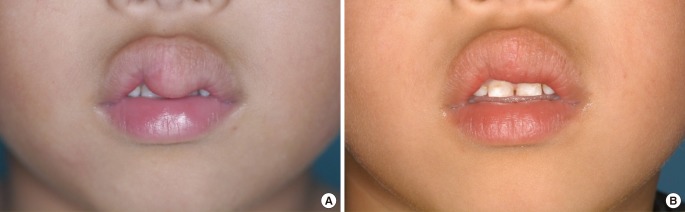
An involuted hemangioma patient
A five-year-old male with an involuted hemangioma on the upper lip. A star-shape excision was performed to correct the deformity on vermilion tubercle. (A) A preoperative image. (B) A postoperative image taken seven months after excision.

A capillary malformation patient
A 76-year-old female with a capillary malformation on the upper lip. A horizontal partial excision was carried out to correct the deformity on the upper lip. (A) A preoperative image. (B) A postoperative image taken four months after partial excision.
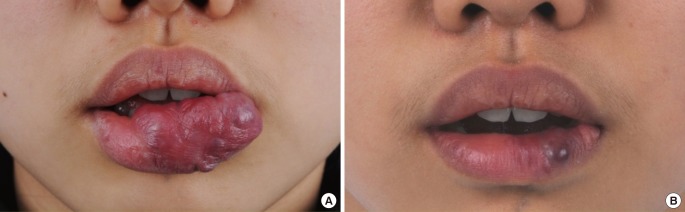
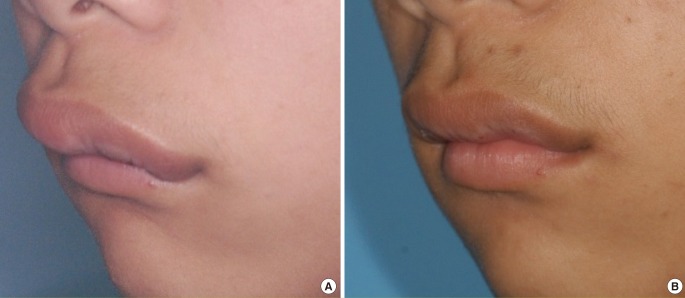
A venous malformation patient
A 14-year-old female with a venous malformation on the lower lip. A horizontal partial excision was performed to correct the deformity on the lower lip. (A) A preoperative image. (B) A postoperative image taken 16 months after partial excision.
A venous malformation patient
A 52-year-old male with a venous malformation on the upper lip. A horizontal partial excision was performed to correct the deformity on the upper lip. (A) A preoperative image. (B) A postoperative image taken 13 months after partial excision.
DISCUSSION
Although the pathogenesis of vascular tumors and vascular malformations, which are classified as vascular anomalies, has not yet been fully elucidated [4], vascular tumors are known to be generated by an increase of endotheliocytes during fetal life or after birth, and vascular malformations are known to be caused by developmental abnormalities in vascular elements during embryogenesis [456789].
Combination treatment involving a multidisciplinary approach is required for such lesions on many parts of the body. Selective surgical treatment is generally performed on hemangiomas during their involuted phase. Capillary malformations are treated with a pulse-dye laser, venous malformations require sclerotherapy or surgical resection, lymphatic malformations are treated with sclerotherapy, and AV malformations are generally treated with a combination of sclerotherapy and surgical resection [456789].
However, difficulties are encountered in the application of several treatment methods to vascular anomalies in the vermilion. For example, laser treatment is difficult when the dermatomal pattern of a unique structure such as the vermilion is involved [101112]. Moreover, laser therapy is inconvenient in that the treatment is implemented in many phases over a number of years, and non-acceptance of laser treatment is also a challenge [10].
No standardized surgical indications for the treatment of vascular anomalies yet exist. Depending on the type of vascular anomaly, nonoperative procedures, such as laser therapy or sclerotherapy, could be carried out, but operative procedures should be considered if nonoperative procedures do not lead to improvement. We consider operative procedures to be reasonably feasible if surgical treatment is likely to lead to contour improvement and if the patient agrees.
Due to the shape of the vermilion and its functional involvement in pronunciation and food intake, it is undesirable to sacrifice the vermilion when resection is performed. On the contrary, when considering the projecting shape and functional aspects of the vermilion, reducing its size adequately helps patients have a normal life. The authors made an effort to preserve preoperative function by not performing extensive resection that could have resulted in postoperative functional loss. Thus, functional improvement was achieved by reducing the volume of the vermilion and improving its contours.
In summary, resectional therapy is required, but in many cases partial excision is necessary, leading to concerns about recurrence of the remaining lesion. Some reports have described cases of recurrence after the surgical treatment of vascular anomalies [13141516], as well as reoperations due to recurrence [131415]. Some researchers have insisted that recurrence of a larger lesion will result from subtotal resections, depending on the type of lesion, but the opposite opinion has also proposed [1718].
In many studies, researchers have asked patients to assess the results of treatment, as well as investigating complications and recurrence [21819]. Since recurrence may not be clearly detectable if the remaining lesion is still present after partial resection, it is especially important to investigate how surgical treatment help patients in their everyday life, which is a question that can be explored through a subjective satisfaction survey.
The authors performed surgical treatment with a focus on contouring in 38 patients with vascular anomalies. In 28 of the patients (approximately 73%), adequate treatment was achieved by one operation, but the other 10 cases (approximately 27%) required two or more operations. Regarding surgical technique, out of a total of 45 operations (with the exception of operations performed to treat AV malformations), partial excision with a horizontal elliptical shape was performed in 28 cases (approximately 62%), making it the most frequent surgical procedure. Six cases of minor complications (approximately 12%) were observed, but the patients recovered without any particular aftereffects after adequate treatment. Recurrence occurred in one case of AV malformation (2%) and a secondary operation was performed. No recurrence has been observed subsequently. The patients reported an average satisfaction level of good or higher.
Performing total excision is seldom possible to treat vascular anomalies of the vermilion because the lesion often involves structures that must be preserved.
A possibility of recurrence exists after the partial excision of vascular anomalies, especially vascular malformations. However, we experienced stable results after partial excisions focused on contouring. Contouring surgery on the vermilion, which has a free margin, showed good results. Additionally, most patients were also satisfied with the results of the operation, indicating that our surgical method focused on contouring has therapeutic value.
Notes
This work was supported by a clinical research grant from Pusan National University Hospital in 2015.
The content of this article was presented at the 72nd Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 7–9, 2014 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.