Induced Hypothermia: Implications for Free Flap Survival
Article information
Plastic surgeons may not be aware that the new advanced cardiac life support (ACLS) guidelines released in 2010 include induced hypothermia as an adjuvant treatment to improve neurologic outcomes following cardiac arrest [1]. Induced hypothermia (IH) is thought to mitigate ischemic damage by lowering metabolic demand and preventing noxious byproducts of resuscitation. IH is recommended for patients who experience the return of spontaneous circulation after cardiac arrest, but remain unconscious [2]. The hypothermia protocol involves the reduction of body temperature to 32℃–34℃ for 12 to 24 hours, followed by slow rewarming [12]. However, the use of induced hypothermia in microvascular free tissue transfer has not been studied. We present the case of a patient who underwent IH following free-flap reconstruction of a head and neck cancer defect.
A 69-year-old male with a history of coronary artery disease and three-vessel coronary artery bypass grafting presented with recurrent basal cell carcinoma of the left ear canal. He underwent total auriculectomy and lateral temporal bone resection, and the defect was reconstructed with a left vertical rectus abdominis myocutaneous free flap. On the second postoperative day, the patient was found unresponsive in pulseless electrical activity cardiac arrest. The ACLS protocol was initiated, including mechanical ventilation and vasopressors for hemodynamic support. The patient was successfully resuscitated but suffered a second cardiac arrest with ventricular fibrillations. He was resuscitated again but remained unresponsive. Hypothermia was induced, with the patient cooled to 32℃ for 48 hours (Fig. 1). The free flap remained well perfused with an audible Doppler signal during the cardiac arrests, vasopressor therapy, hypothermic cooling, and the remainder of his hospitalization (Fig. 2). Unfortunately, the patient had no meaningful neurologic recovery and magnetic resonance imaging showed diffuse hypoxic brain injury. Therefore, the family elected to withdraw care on postoperative day 10.
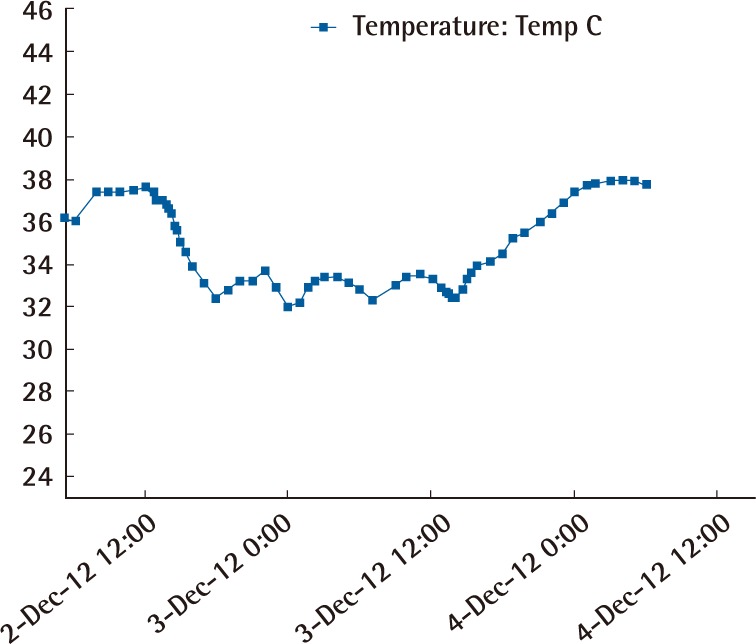
Temperature curve showing induced hypothermia to 32℃–34℃, from postoperative day three until postoperative day five.

A 69-year-old male underwent composite resection of the left auriculotemporal area and temporal bone for recurrent basal cell carcinoma, and the defect was reconstructed with a left vertical rectus abdominis myocutaneous free flap.
The effects of systemic hypothermia on free tissue transfer are not fully understood. Limited animal and human studies have demonstrated conflicting results. Some data have suggested that hypothermia causes decreased perfusion, vasospasm, and thrombosis, while other animal experiments have shown a protective effect of mild hypothermia on free flaps [345]. Clotting enzymes, platelets, and leukocytes function less effectively in a hypothermic setting; however, no reports have been published on the effect of severe hypothermia (<34℃) on free flap survival in humans.
This is the first reported case of induced hypothermia after free tissue transfer. Plastic surgeons should be aware of ongoing changes to the ACLS algorithm and its impact on perioperative care. In this case, a free tissue transfer remained viable despite induced hypothermia and vasopressors, which is a single data point suggesting that free flaps can tolerate such interventions. However, further research is needed to clarify the effects of hypothermia on free tissue transfer.
Notes
No potential conflict of interest relevant to this article was reported.