A Rare Case of an Epidermal Inclusion Cyst in the Joint Capsule of the Thumb
Article information
Epidermal inclusion cysts are one of the most common types of benign lesions that present in the subcutaneous tissue, and they are observed as fluctuating nodules [1]. They may occur in all body areas composed of squamous epithelium. However, intra-articular involvement of such cysts has been described very rarely in the literature [2]. We experienced a case of an epidermal inclusion cyst occurring in the joint capsule of the thumb in a patient with a past history of thumb trauma. Herein, we report our case and provide a review of the relevant literature.
A 75-year-old man visited us with a chief complaint of a six-month history of a mass in the interphalangeal joint of the right thumb. The patient complained of aggravated pain associated with the recently increased size of the mass (Fig. 1A). On physical examination, the patient exhibited tenderness. The patient also had fixed lesions with a firm consistency. Twenty-three years previously, the patient experienced a crushing injury to the left thumb, for which he underwent inguinal flap surgery and bone graft. However, the patient developed osteomyelitis in the bone graft site and underwent excision of the grafted bone tissue. Subsequently, the patient experienced multiple recurrences of epidermal inclusion cysts on the right thumb, which were excised. On plain radiography, the patient demonstrated radiolucent lesions accompanied by soft tissue swelling in the distal phalanx of the thumb. A connection was observed between the origin of the mass and the interphalangeal joint, based on which the mass was suspected to have occurred in the joint (Fig. 1B). In order to perform a differential diagnosis leading to the accurate diagnosis of the mass, we planned to excise and biopsy the mass under local anesthesia. By making an incision right superior to the lesion and dissecting the lesion, we were able to confirm the presence of a mass originating from the interphalangeal joint space (Fig. 2A). The mass was encapsulated and had a well-defined margin, and protruded to the epidermis in the right inferior region. It was easily dissected and then completely excised. Both the distal and proximal phalangeal joints were fixed using an arthrodesis. The excised mass was measured to be 2.0×1.5 cm. It contained keratin and lipid debris from sebaceous secretions. Moreover, histopathological examination found an abundant presence of keratin on the interior side of the cystic wall composed of stratified squamous epithelium. However, no signs of other skin appendages were observed. Based on these findings, the patient was diagnosed with an epidermal inclusion cyst (Fig. 2B). During a six-month postoperative follow-up period, the mass did not recur and no other notable findings were observed (Fig. 3).
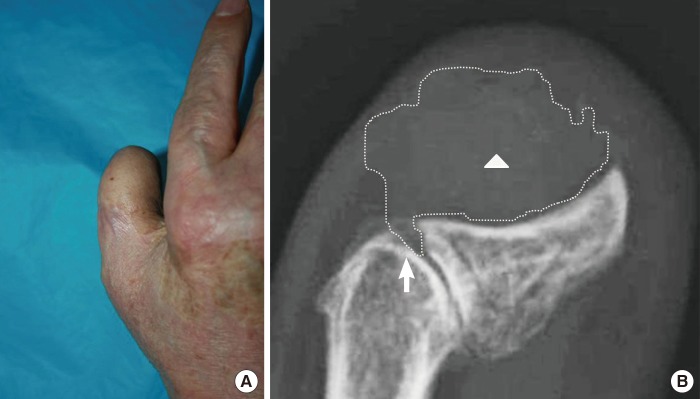
(A) A 75-year-old male who had a mass within the interphalangeal joint capsule of the right thumb. (B) Widening of the interphalangeal joint space (white arrow) was observed and the origin of the radiolucent mass (white arrowhead) appeared to be located within the joint (dotted line, the boundary of the mass).
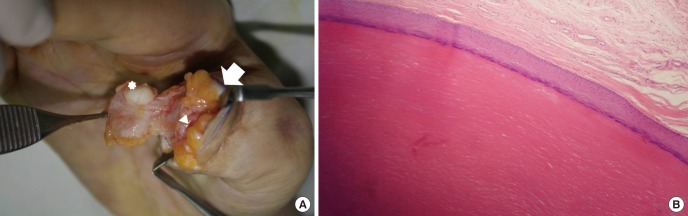
(A) The encapsulated mass (star-shaped, 2.0×1.5 cm) occurred within the interphalangeal joint (white arrowhead) of the right thumb (white arrow, distal head of proximal phalangeal bone). (B) In pathological findings, stratified squamous epithelial layers with laminated keratin layers were seen, and no hair follicles or skin appendages were present (H&E, ×100).
It is generally known that epidermal inclusion cysts occur in the dermis or subcutaneous layer. Most cases of epidermal inclusion cysts are asymptomatic. Therefore, an epidermal inclusion cyst is recognized when it protrudes to the superior region to the skin. In cases of epidermal inclusion cysts occurring in fingers, the differential diagnosis must exclude benign lesions, such as warts, fibroma, osteochondroma, and glomus tumor, as well as other conditions, such as squamous cell carcinoma and malignant melanoma. However, epidermal inclusion cysts are not associated with any typical signs and symptoms. This poses a differential diagnostic challenge for surgeons. In the current case, the patient presented with a gradual increase in a mass present in the interphalangeal joint of the thumb. It was palpable as a hardened mass, and was accompanied by intermittent pain and tenderness. The patient had a mass originating from the joint, based on which the patient was suspected of having heterotrophic ossification or osteochondroma. However, osteochondroma is characterized by heterotrophic calcification on plain radiography [3], which was not found in the current case.
According to a review of the literature, it is very rare for epidermal inclusion cysts to occur in the joint. Strauchen and Strefling [4] reported a case of an epidermal inclusion cyst occurring after arthroscopic surgery in the knee joint. However, this case occurred in the knee joint. To the best of our knowledge, no cases of epidermal inclusion cysts occurring in the interphalangeal joint have been described.
In the current case, the patient had a past history of trauma and developed the epidermal inclusion cyst at the site of the trauma. It can therefore be inferred that it is very unlikely for epidermal inclusion cysts to occur as congenital lesions. Based on other cases of epidermal inclusion cysts arising due to trauma, it is very likely that epidermal inclusion cysts in joints occur as a result of the squamous cells forming the epidermis being directly invaginated into the joint due to the trauma, or due to the invasion of a preexisting epidermal inclusion cyst into the joint [5]. Still, little is known about the exact pathophysiology underlying the intra-articular presence of epidermal inclusion cysts, which deserves further study. In conclusion, our case highlights the possibility that epidermal inclusion cysts might also occur, albeit rarely, in the interphalangeal joints of the fingers. Recognizing this may be essential for avoiding unnecessary operations and amputations of fingers. Finally, we propose that masses found in the fingers should undergo histopathological examination in order to ensure that epidermal inclusion cysts are properly diagnosed and appropriately treated.
Notes
This article was presented as a poster at the 72nd Congress of the Korean Society of Plastic and Reconstructive Surgeons on November 7–9, 2014 in Seoul, Korea.
No potential conflict of interest relevant to this article was reported.
