Alternative Treatment of Osteoma Using an Endoscopic Holmium-YAG Laser
Article information
Abstract
Osteoma is one of the most common tumors of the cranial vault and the facial skeleton. For osteoma in the facial region, endoscopic resection is widely used to prevent surgical scarring. Tumors in a total of 14 patients were resected using an endoscopic holmium-doped yttrium aluminium garnet (Ho:YAG) laser with a long flexible fiber. Aside from having the advantage of not leaving a scar due to the use of endoscopy, this procedure allowed resection at any position, was minimally invasive, and caused less postoperative pain. This method yielded excellent cosmetic results, so the endoscopic Ho:YAG laser is expected to emerge as a good treatment option for osteoma.
INTRODUCTION
Osteomas are the most common tumors of the cranial vault and facial skeleton. They can occur in any part of the skull, both in the frontal and parietal bones. They are typically detected in young adults and are more common in women than in men [1]. They are usually benign, and their symptoms are facial deformity, facial pain, and headache. Their treatment is indicated when their symptoms are present, and it is desirable to remove them for cosmetic purposes. A simple resection is generally performed, but it scars the skin. Thus, in recent years, attention has increasingly been focused on using endoscopic surgery to treat osteomas in the facial region. The advantages of endoscopic surgery are better cosmetic results because the scars are not noticeable due to the non-visible incision line, and reduction of postoperative pain and complications because of its minimal invasiveness.
The procedure currently used for edoscopic surgery involves applying an incision to the hairline. Endoscopy is then performed at the periosteum level to approach the tumor site, followed by tumor removal, which is often performed using an osteotome with another incision. In such cases, the rigidity of endoscopic tools, however, due to the osteotome when the osteoma is being directly removed, makes it difficult to remove an osteoma that has a bulging head and one that is far from the hairline. Therefore, a long and flexible fiber was used to treat frontal osteoma with the holmium-doped yttrium aluminium garnet (Ho:YAG) laser. The frontal osteoma was easily reached with a hidden incision line, and was easily removed no matter where it was located. As such, we herein report on a total of 14 patients that had been diagnosed with frontal osteoma in which the tumors were successfully removed using an endoscopic Ho:YAG laser.
CASE
A 28-year-old woman presented with a palpable mass, which had occurred 10 years earlier, in the forehead and the resulting contour deformity. Though the mass caused no pain or headache, the patient wanted the mass excised because of aesthetic concerns. Facial three-dimensional computed tomography confirmed the mass to be an osteoma; thus, surgery was performed under general anesthesia.
During the operation, an endoscope was used with a 30-degree-type angle-vision with a light source. The endoscope was connected to a camera, and the endoscopic images were transferred to a television monitor. At two sites, 1 cm skin incisions were made at 1.5 cm superior to the hairline on the scalp above the forehead. One of these incisions was for inserting the endoscope, and the other was for inserting the surgical instruments (Fig. 1). The incisions were made at the periosteum, and some subperiosteal undermining was performed using a periosteal elevator. When the endoscope was inserted, the dissection continued until the osteoma was seen and the area was exposed. To ensure a large enough operating space, one suture was applied on the skin just above the osteoma, and the skin was lifted. Continuous irrigation helped maintain a clear view. The flexible fiber of the Ho:YAG laser was then inserted. The Ho:YAG laser energy was set at an intensity of 0.8 J at a rate of 5 Hz and with 60 watts of power. As the tip of the endoscopic fiber came into contact with the cranial surface with the frontal osteoma the energy was gradually increased, and the osteoma was excised under direct vision due to continuous saline irrigation (Fig. 2). Finally, the wound was closed, and the incision site on the forehead was covered with a soft-pressure elastic bandage. The patient was discharged 1 day postoperatively. Computed tomography was performed 4 weeks postoperatively, and the complete resection of the tumor and a smooth facial contour were observed. Three months later, the outcome was assessed to be aesthetically excellent, and the patient was also satisfied with the outcome (Figs. 3, 4).
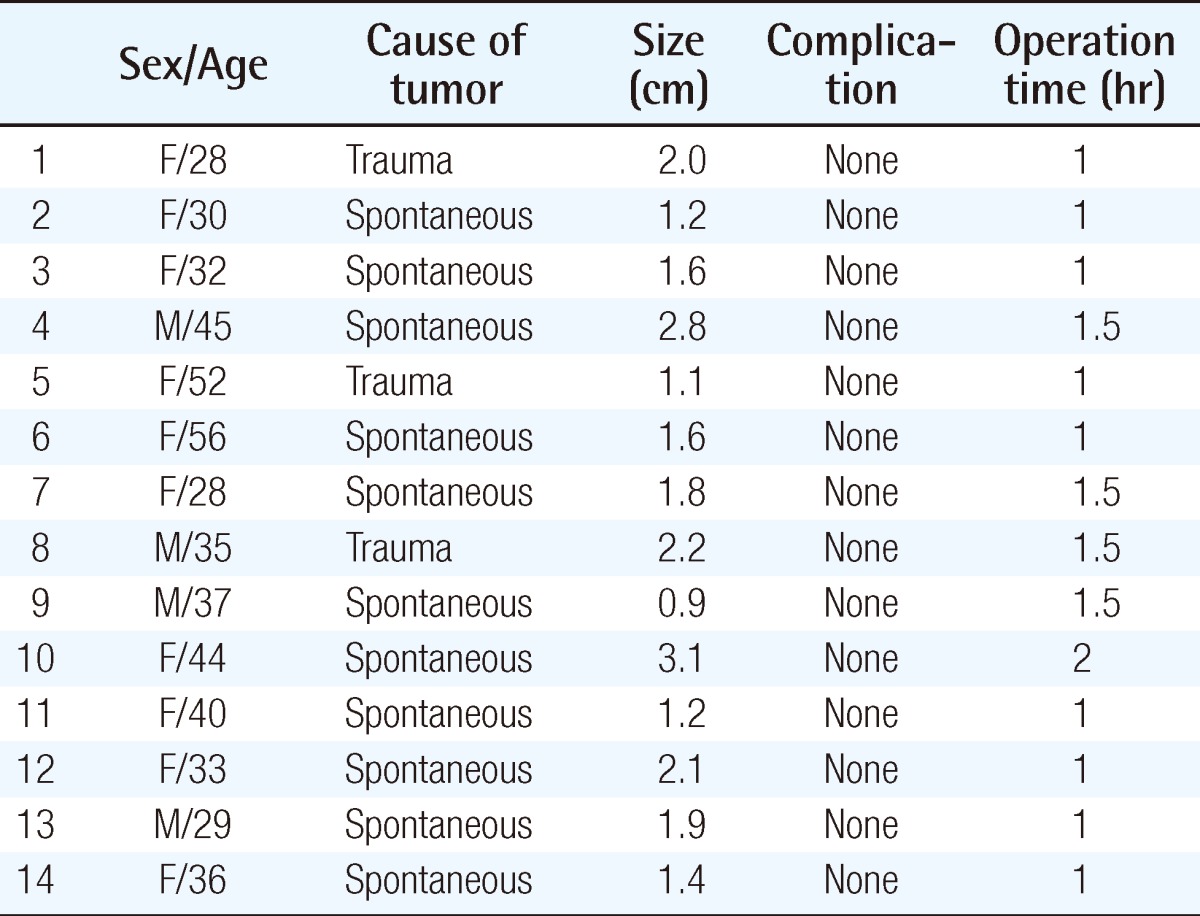
Schematic diagram of the operative procedure
The operation is performed by inserting an endoscope and laser fiber through the two incisions made in the region covered with hair.
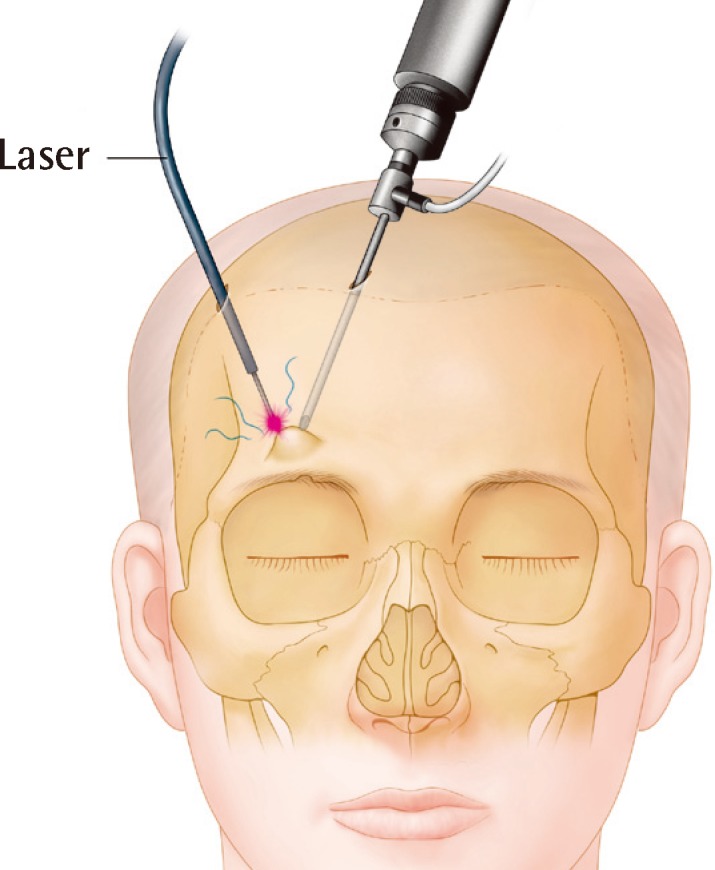
Intraoperative endoscopic finding
The tip of the endoscopic fiber came into contact with the cranial surface, osteoma was excised under direct vision.
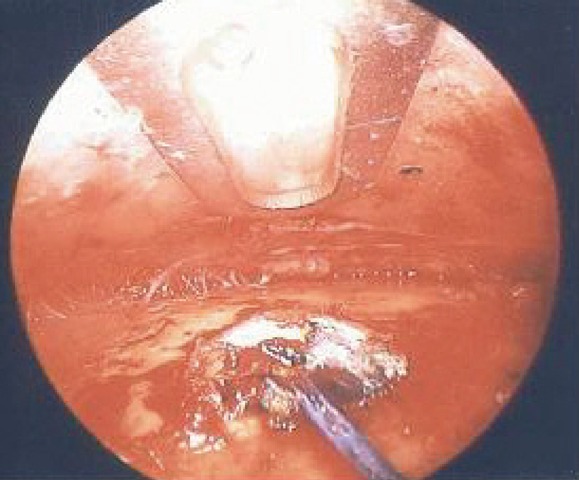
Preoperative and postoperative photographic findings
A preoperative picture (A) showing an osteoma of the forehead (blue arrow, osteoma of the forehead). A postoperative picture (B) at 4-weeks follow-up.
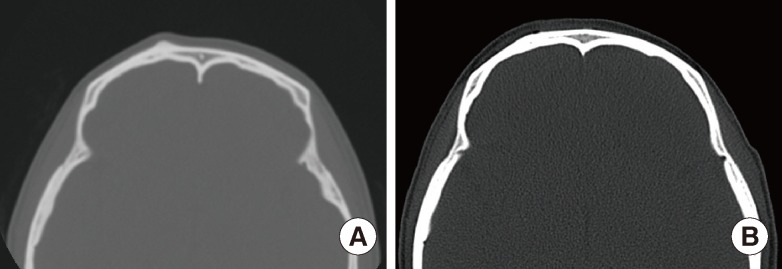
Preoperative and postoperative computed tomographic findings
(A) Computed tomographic scans of a patient's head revealing a preoperative small nodule with a frontal bone osteoma. (B) A postoperative scan was performed 4 weeks after and showed a smooth contour of the forehead after the osteoma was removed.
DISCUSSION
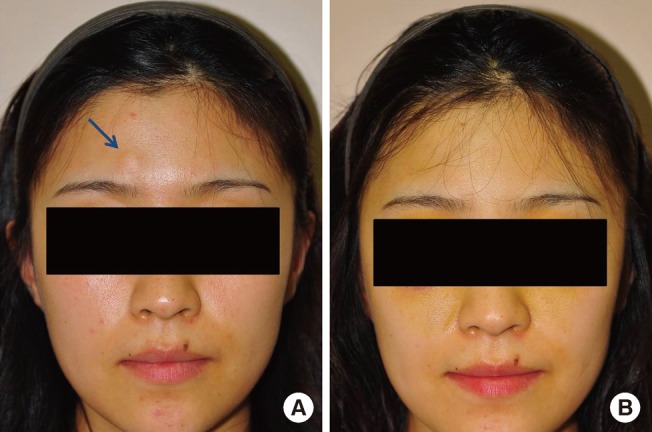
The surgery was performed in a total of 14 patients with frontal bone osteomas in the period from October 2010 to August 2011. The chief complaint of all of the patients was a palpable contour deformity with or without pain, which was surgically evaluated. The patients included 10 women and 4 men, with ages ranging from 28 to 56 years (Table 1). All of the patients were treated by a single surgeon.
Osteomas are unusual but not rare [2]. According to Jung et al. [3], frontal osteoma usually occurs in the midline of the frontal bone, and females are more prone to it than males. Altman et al. [4] have recommended the removal of osteomas while they are still small, rather than after the symptoms of their extension appear. Although osteomas are usually benign and slow-growing, they may occasionally lead to dangerous sequelae over time [5]. In this study, the patients considered the aesthetic problems caused by the mass the most important factor rather than recognizing other symptoms and risks of the mass. As the masses were in the face, an endoscopic surgical approach to the hairy portion of the mass is important to achieve good aesthetic outcomes.
Osteomas in the cranio-maxillofacial region are commonly removed through a direct incision above the tumor. This method is simple and easy, but it leaves a scar, and the incision may need to be lengthened according to the size of the osteoma. Onishi et al. [6] have removed an osteoma in the forehead using an endoscope and a curved osteotome after making an incision on the hairy portion. This procedure is presently common because it does not leave scars, it usually removes the osteoma through a less than 1 cm long incision, it is minimally invasive, and does not cause nerve or vessel injury. In the present authors' experience, however, there are instances when a complete resection is difficult to perform with this method because energy is not properly transmitted when the tumor is resected through an osteotome, and the osteotomy devices as well as the rigidity and thickness of the endoscopic fiber make it too difficult to reach the curved spot. There have been some cases where it was difficult to approach. These include cases of patients with frontal bossing, when the tumor was in an area far apart from the hairline such as the eyebrow area, when the incision line had to be extended, or even in cases where the osteoma had to be removed through bicoronal approach. Thus, in this study, we sought a method for approaching all of the locations to deliver energy easily to the protruding mass and to reduce injury to the surrounding soft tissue. Unlike when an osteotome is used, when a tumor is resected using a Ho:YAG laser, no matter where the incision is made on the hairy portion, it is easy to reach the tumor through a flexible fiber. Moreover, complete resection was easier with gradual resection through a laser than with resection through an osteotome. A smooth contour was visible even in the postoperative computed tomography findings in the majority of cases. Due to such advantages, the operative time did not differ significantly based on the removal method, which consisted of endoscopy and osteotome; in the case of a mass that required the bicoronal approach due to its size and distance from the hairline, the operative time could be significantly reduced. The two incisions superior to the hairline on the scalp in the forehead were both 1 cm, and the extent of swelling due to the wound after the surgery was performed was also similar. The patients did not complain of headaches or pain in the resection site after surgery. Though an osteotome had been used in the previous procedure delivering direct impact to the cranial vault, pain is considered to have been reduced due to resection using a laser.
The Ho:YAG laser emits a holmium wavelength (2,140 nm, non-visible/infrared) that is strongly absorbed by water and is in the near-infrared range of the electromagnetic spectrum [7]. It provides excellent hemostasis but with an absorption depth of only 0.4 mm [8]. It is a pulsed laser, and with each pulse a burst of energy is transmitted at the kilowatt range that leads to precise tissue vaporization at the tip of the laser fiber. Unlike the CO2 laser typically used in the past for resecting osteomas, the Ho:YAG laser is ideal for use with endoscopy because it is capable of delivering energy through a fiber-optic device, energy is immediately dissipated under a liquid-filled environment, and it does not damage the surrounding tissue. In our cases, resection was performed while continuous irrigation was applied to take advantage of this heat dissipation, and we were able to accurately perform resection of the tumor without causing heat injury to the nearby bones or soft tissue because we applied energy only to the target site.
A Ho:YAG laser, which is often used to make an incision on cartilaginous material, osteophytes, and for lithotripsy, was used to treat osteoma with 60 watts of power; this is enough energy to detach the osteoma from the forehead. As such, the Ho:YAG laser has been in standard use for treating the genitourinary tract such as in endoscopic prostatectomy and urinary lithotripsy. Furthermore, its use in orthopedic surgery or otolaryngology is gradually increasing. Although there are reports that osteomas of the sacral area have been removed using a Ho:YAG laser, there is no literature on the use of the Ho:YAG laser in the maxillofacial region or the removal of a bone tumor such as an osteoma. By successfully removing bone tumors such as osteomas from the forehead using a Ho:YAG laser, this study found much potential for using a laser in maxillofacial surgery.
The method of treating osteoma using an endoscopic Ho:YAG laser is minimally invasive, easily enables approaching the areas and contours of the osteoma, and reduces soft tissue damage and postoperative pain. This method also has excellent cosmetic results. Thus, the endoscopic Ho:YAG laser should be a good treatment option for osteoma.
Notes
No potential conflict of interest relevant to this article was reported.